Category: Cardiology
Keywords: electrocardiography, posterior, myocardial infarction (PubMed Search)
Posted: 9/26/2010 by Amal Mattu, MD
(Updated: 10/3/2010)
Click here to contact Amal Mattu, MD
Approximately 4% of acute MIs will present as an isolated posterior MI (AKA "true posterior MI"). These are easily misdiagnosed as simply anterior ischemia because of the ECG findings. However, the distinction is critically important because posterior STEMI is now considered an indication for immediate reperfusion (PCI or lytics), whereas anterior ischemia is not.
The diagnosis of posterior STEMI is made by looking for:
1. ST segment depression, typically in leads V1-V3
2. upright T-waves in leads V1-V3
3. development of tall R-waves (R > S in amplitude) in V1-V3 over the course of a few hours (this is analogous to Q-waves forming in the posterior portion of the ventricle)
Early on, you may not be able to rely on the presence of tall R-waves to help you. Therefore, it's best to simply do the following: whenever you find ST-segment depression in leads V1-V3, always repeat the ECG using posterior leads (simply place a couple of the V leads on the left mid-back area). These leads will "look" directly at the posterior heart. If those leads show ST elevation, the diagnosis is posterior STEMI. If those leads don't show ST elevation, you can then make the diagnosis of simply anterior ischemia and hold off on immediate PCI or lytics.
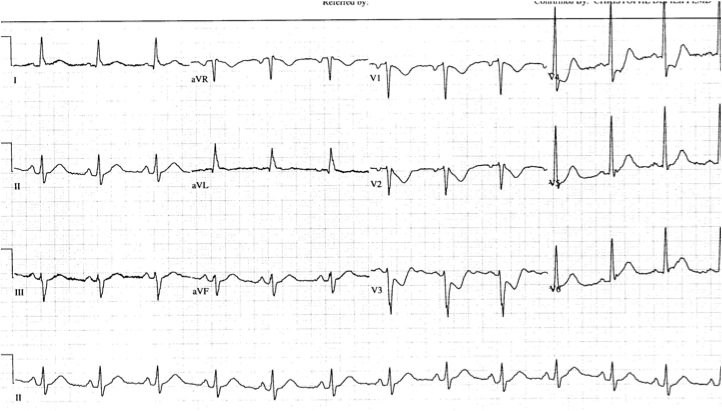
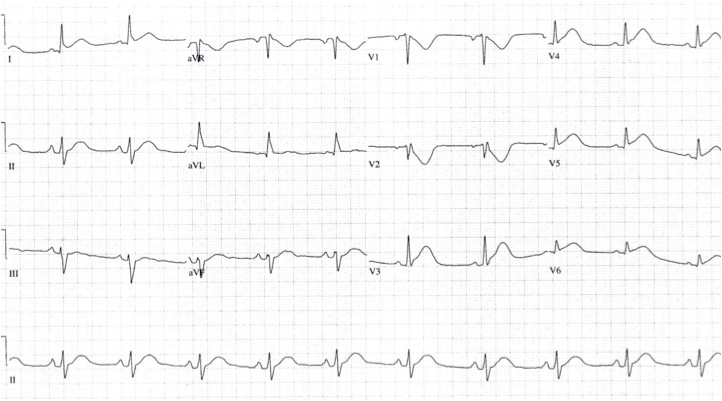
The first ECG below shows ST depression in the anteroseptal leads, suspicious for posterior STEMI. The ECG was then repeated, second ECG, with leads V3-V6 placed wrapping around to the left mid-back area. The ST elevation in these leads confirmed the presence of a posterior STEMI and justified immediate reperfusion therapy.