Category: Misc
Keywords: sample size calculation, biostatistics (PubMed Search)
Posted: 7/25/2024 by Mike Witting, MD
(Updated: 7/27/2024)
Click here to contact Mike Witting, MD
Free Biostatistics Software Options
EpiCalc 2000 – available for Windows. Capabilities include sample size calculation, inferential statistics (p values, 95% CI), simple stratified analysis, paired and independent analyses. Right clicking allows you to do many things. (http://www.brixtonhealth.com/epicalc.html). I've had the most experience with this one.
Epi Info – supported by CDC. Available for Windows and for hand-held. (https://www.cdc.gov/epiinfo/index.html)
P/S – Power and Sample Size Calculation – available for Mac and Window. Supported by Vanderbilt biostatistics. (https://biostat.app.vumc.org/wiki/Main/PowerSampleSize)
Epicalc: http://www.brixtonhealth.com/epicalc.html
Epi Info: https://www.cdc.gov/epiinfo/index.html
Category: Administration
Keywords: Administration, Meetings, Workforce satisfaction (PubMed Search)
Posted: 7/24/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Participation in meetings is an expected part of most (if not all) of our jobs. How many of these meetings are necessary? Could some of the “work” of meetings be accomplished with a few emails or other asynchronous forms of communication? Are meetings cluttering your schedule and making it impossible to get any real work done?
Some answers to these questions are offered in a Harvard Business Review article from March 2022.
Key points include:
Advantages to fewer meetings:
Authors recommend holding meetings only when “absolutely” necessary. That typically includes:
Laker B, Pereira V, Malik A, and Soga L. Meeting Management: Dear Manager, You’re Holding Too Many Meetings. Harvard Business Review. March 9, 2022.
Category: Critical Care
Posted: 7/23/2024 by William Teeter, MD
(Updated: 7/27/2024)
Click here to contact William Teeter, MD
Do Sepsis Alert Systems Work?
Researchers in Korea completed a high quality systematic review and meta-analysis of sepsis alert systems for adult ED patients
Using high quality methods, they identified over 3000 studies with 22 meeting criteria.
They found these systems were associated with:
Electronic alerts were further associated with:
Summary (+ a little editorialization)
As annoying as we may find these systems in our daily practice, there is growing evidence that they do provide some benefit with impacts on task saturation and decreasing cognitive load in addition to real patient benefit. While there is also recent evidence that physician gestalt performs well against these systems, there is a suggested benefit in their inclusion in clinical decision making as a safety net or as an “assist”.
The incorporation of rule-based algorithms like these in more advance machine learning methods are covered quite well in a recent opinion piece on “The AI Future of Emergency Medicine”. However, it is important to always know the source of any “algorithm” that you are using, whether rule or mathematically based, given real concerns for bias and error.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821277
https://www.sciencedirect.com/science/article/pii/S019606442400043X
https://www.sciencedirect.com/science/article/abs/pii/S0196064424000994
Category: Hematology/Oncology
Keywords: Hematology, Anemia (PubMed Search)
Posted: 7/22/2024 by Sarah Dubbs, MD
Click here to contact Sarah Dubbs, MD
Iron-deficiency anemia affects 10% of women of child-bearing age. Guidelines to treat iron deficiency recommend daily oral iron, but this may decrease fractional iron absorption and increase side effects which also impacts medication adherence. A double-masked, randomized, placebo-controlled trial, which included 150 women demonstrated that:
at equal total iron doses, compared to consecutive day dosing of iron, alternate day dosing did not result in higher serum ferritin but reduced iron deficiency at 6 months and triggered fewer gastrointestinal side effects.
Take home point: Dosing iron every other day had similar effect with less side effects. Consider prescribing it this way to your patients, especially if they have had issues with side effects in the past!
von Siebenthal HK, Gessler S, Vallelian F, Steinwendner J, Kuenzi UM, Moretti D, Zimmermann MB, Stoffel NU. Alternate day versus consecutive day oral iron supplementation in iron-depleted women: a randomized double-blind placebo-controlled study. EClinicalMedicine. 2023 Nov 3;65:102286. doi: 10.1016/j.eclinm.2023.102286. PMID: 38021373; PMCID: PMC10659995.
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00463-7/fulltext
Category: Trauma
Keywords: Txa, TBI, seizure, risk (PubMed Search)
Posted: 7/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
According to this study, no TXA 2g bolus was not found to increase the number of seizures in TBI pts.
TXA has been shown to improve mortality in inter cranial hemorrhage trauma patients if given within 2 hours. TXA is also known to lower seizure threshold. This study was a secondary analysis of a larger study comparing placebo to 1 g TXA bolus plus 8 hour infusion or 2g bolus TXA in the prehospital setting. There was no difference in the number of pts experiencing seizure or outcome in those receiving the 2g bolus of TXA.
The Association Between Tranexamic Acid and Seizures in Moderate or Severe Traumatic Brain Injury
David V. Deshpande BS a, W. Ian McKinley MD, MS b, Andrew J. Benjamin MD, MS c, Martin A. Schreiber MD, FACS, FCCM d, Susan E. Rowell MD, MBA, MCR
Volume 301, September 2024, Pages 359-364 https://doi.org/10.1016/j.jss.2024.06.035
Category: Pediatrics
Keywords: mental health, sedation, home medications (PubMed Search)
Posted: 7/19/2024 by Jenny Guyther, MD
(Updated: 7/27/2024)
Click here to contact Jenny Guyther, MD
Emergency department visits for pediatric mental health and behavioural concerns have been increasing. This study attempted to further characterize medications, both home and for sedation, that were given to these patients.
This study included 670,911 youth with a mental or behavioral health diagnosis over a 9 year inclusion period. The most common diagnses were depressive disorder, suicide or self injury and disruptive, impulse control and conduct disorder. During this time, a total of 12.3% of patients had a psychotropic medication given while in the ED. The percentage and odds of administering these medications increased from 7.9% in 2013 to 16.3% in 2022. Those with intellectual disability and autism spectrum disorder had the highest frequency of medication administration.
Bottom line: As mental health visits in pediatrics continue to increase along with boarding times, clinicians should become more familiar with psychotropic medications used in this population and become comfortable in making sure that these patients have their home medications and have a plan for chemical sedation if other areas of de escalation fail.
Category: Pulmonary
Keywords: pulmonary embolism, intervention, scoring, out come (PubMed Search)
Posted: 7/18/2024 by Robert Flint, MD
(Updated: 7/27/2024)
Click here to contact Robert Flint, MD
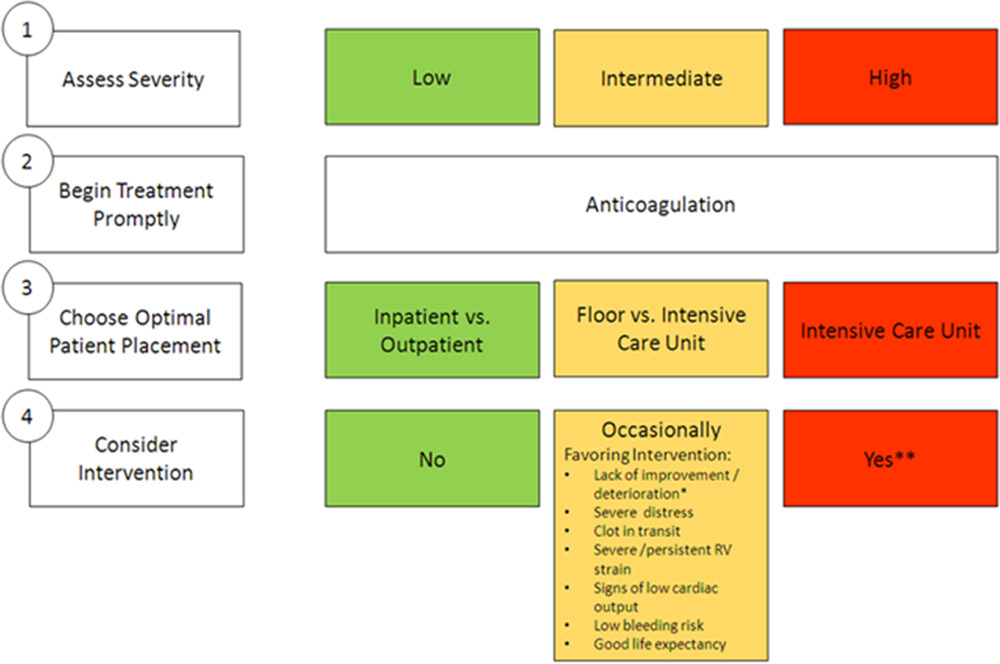
Deciding which pulmonary embolism patient needs thrombolytics/catheter based intervention is a shared decision among emergency physicians, intensivists, interventionalists, hospitalists, and the patient/family. This article provides evidence to help guide this decision. Keep in mind “The use of either CDL or catheter-based embolectomy in patients with intermediate-risk PE has, thus far, been correlated only with more rapid improvement of RV dysfunction than anticoagulation alone, not short- or long-term clinical or functional outcomes.”
"1. Massive (AHA) or high risk (ESC): Hypotension, defined as a systolic blood pressure <90 mm?Hg, a drop of >40 mm?Hg for at least 15 minutes (this latter criterion may be difficult to ascertain in some clinical circumstances), or need for vasopressor support, identifies these patients. They account for ?5% of hospitalized patients with PE and have an average mortality of ?30% within 1 month.
2.Submassive (AHA) or intermediate risk (ESC): RV strain without hypotension (see above) primarily identifies these patients. RV strain includes RV dysfunction on computed tomography pulmonary angiography or echocardiography (RV/left ventricular [LV] ratio >0.9)6,7 or RV injury and pressure overload detected by an increase in cardiac biomarkers such as troponins or brain natriuretic hormone.
3.Low risk (ESC and AHA): These patients do not meet criteria for submassive (AHA) or intermediate-risk (ESC) PE"
Interventional Therapies for Acute Pulmonary Embolism: Current Status and Principles for the Development of Novel Evidence: A Scientific Statement From the American Heart Association
Jay Giri, MD, MPH, FAHA, Chair, Akhilesh K. Sista, MD, FAHA, Vice Chair, Ido Weinberg, MD, MSc, Clive Kearon, MB, PhD, Dharam J. Kumbhani, MD, FAHA, Nimesh D. Desai, MD, PhD, Gregory Piazza, MD, MS, FAHA, Mark T. Gladwin, MD, FAHA, Saurav Chatterjee, MD, Taisei Kobayashi, MD, Christopher Kabrhel, MD, MPH, and Geoffrey D. Barnes, MD, MSc, FAHAAUTHOR INFO & AFFILIATIONS
Circulation
Category: Administration
Keywords: osteomyelitis, antibiotics, golden hour, trauma, open fracture (PubMed Search)
Posted: 7/17/2024 by Jenny Guyther, MD
(Updated: 7/27/2024)
Click here to contact Jenny Guyther, MD
Early administration of antibiotics for open fractures can reduce serious bone and soft tissue infections, with a common goal being antibiotic administration within one hour of injury.
In this study, there were 523 patients treated by EMS who had an open extremity fracture.
The median time from EMS dispatch until antibiotic administration was 31 minutes. 99% of the patients who received antibiotics received them within one hour of EMS dispatch. Prehospital times were on average 10 minutes longer for those patients who received antibiotics. The majority of these patients received cefazolin, followed by ceftriaxone, ampicillin, gentamicin and piperacillin/tazobactam. None of these patients required management for an allergic reaction or anaphylaxis. Five patients (1%) who received prehospital antibiotics and 159 patients who did not (1.4%) had a subsequent infection based on ICD codes.
Bottom line: In this small group, it was safe to administer antibiotics to a patient with an isolated open extremity fracture and the medication was able to be delivered earlier. Larger studies will be needed to see the impact of this practice on the development of osteomyelitis or soft tissue infections.
Muniz AD, Gregorio DJ, Studebaker SA, et al. Time Savings and Safety of EMS Administration of Antibiotics for Open Fractures. Prehosp Emerg Care. Published online April 25, 2024. doi:10.1080/10903127.2024.2347291
Category: Critical Care
Posted: 7/16/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
The CLOVERS trial (NEJM 2023) examined one of the eternal questions of critical care, liberal vs restrictive fluid management in sepsis… and found no difference. But there are criticism of CLOVERS, and while some other trials agreed with this result, there are also signals in the literature that restrictive fluid strategies are beneficial. Furthermore, we know that these trials suffer from issues of heterogeneity, and often lump together very different patients.
Jorda et al recently published in Critical Care a posthoc re-analysis of CLOVERS looking specifically at patients with advanced CKD (eGFR < 30). This is a challenging group of patients to manage. On the one hand their renal function is already marginal, so the last thing we want to do is potentially deprive starved kidneys of necessary intravascular volume, but on the flip side their septic shock puts them at high risk of full blown renal failure (transient or permanent) and they're thus at very high risk of fluid overload with aggressive resuscitative fluids and potentially limited ability to clear those fluids renally in the next few days. So how did these patients do in CLOVERS?
They did significantly better with the restrictive fluid strategy (mortality 22% vs 39%, HR CI 0.29-0.85). They also had more pressor free days and vent free days.
Bottom Line (my opinion): While a restrictive vs liberal fluid strategy in septic shock remains a bit up for debate, the evidence continues to slowly tip towards restrictive fluids (i.e. earlier pressors) as the preferred approach. In patients with advanced CKD (eGFR < 30), there is probably now sufficient evidence to favor vasopressors over IV fluid administration when resuscitating septic shock.
Jorda A, Douglas IS, Staudinger T, Heinz G, Bergmann F, Oberbauer R, Sengölge G, Zeitlinger M, Jilma B, Shapiro NI, Gelbenegger G. Fluid management for sepsis-induced hypotension in patients with advanced chronic kidney disease: a secondary analysis of the CLOVERS trial. Crit Care. 2024 Jul 11;28(1):231. doi: 10.1186/s13054-024-05019-6. PMID: 38992663; PMCID: PMC11238412.
National Heart, Lung, and Blood Institute Prevention and Early Treatment of Acute Lung Injury Clinical Trials Network; Shapiro NI, Douglas IS, Brower RG, Brown SM, Exline MC, Ginde AA, Gong MN, Grissom CK, Hayden D, Hough CL, Huang W, Iwashyna TJ, Jones AE, Khan A, Lai P, Liu KD, Miller CD, Oldmixon K, Park PK, Rice TW, Ringwood N, Semler MW, Steingrub JS, Talmor D, Thompson BT, Yealy DM, Self WH. Early Restrictive or Liberal Fluid Management for Sepsis-Induced Hypotension. N Engl J Med. 2023 Feb 9;388(6):499-510. doi: 10.1056/NEJMoa2212663. Epub 2023 Jan 21. PMID: 36688507; PMCID: PMC10685906.
Category: Ultrasound
Keywords: POCUS, fluid resuscitation, Inferior Vena Cava (PubMed Search)
Posted: 7/15/2024 by Alexis Salerno, MD
(Updated: 7/27/2024)
Click here to contact Alexis Salerno, MD
Many may look at the Inferior Vena Cava (IVC) to get a sense of a patient's “fluid responsiveness.” However, there are many pitfalls to using the IVC. An article by Via et al outlines these pitfalls and is an interesting read!
To summarize, IVC can be affected by:
Bottom Line: Think twice before using IVC to evaluate for fluid responsiveness.
Via G, Tavazzi G, Price S. Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med. 2016 Jul;42(7):1164-7. doi: 10.1007/s00134-016-4357-9.
Category: Pulmonary
Keywords: pulmonary embolism, BOVA Sscore, intervention (PubMed Search)
Posted: 7/11/2024 by Robert Flint, MD
(Emailed: 7/14/2024)
(Updated: 7/14/2024)
Click here to contact Robert Flint, MD
The Bova score has been validated to predict mortality and complications in hemodynamically stable patients with intermediate to high-risk pulmonary embolisms. There is some literature on using the Bova score to decide on thrombolytics/interventional therapy as well.
Scoring Criteria:
Interpretation:
Category: Orthopedics
Posted: 7/13/2024 by Brian Corwell, MD
(Updated: 7/27/2024)
Click here to contact Brian Corwell, MD
A 2020 meta-analysis attempted to estimate the frequency of radiographically occult hip fractures in the elderly population.
26 studies evaluated the rate of surgical hip fractures with no obvious findings on plain film.
Median age 80.3 years (67-82 years).
MRI used as gold standard.
The overall rate of radiographically occult hip fracture requiring surgery was 39%.
This percentage is higher than reported in other studies which may have included non-elderly patients, retrospective bias or other issues.
Overall, 18% had femoral neck fractures, 17% had intertrochanteric fractures and 1% had subtrochanteric fractures.
Elderly patients with acute hip pain and negative or equivocal findings with initial plain film imaging have a high frequency of occult hip fractures. Strongly consider advanced imaging in this population
Category: Pharmacology & Therapeutics
Keywords: Hyponatremia, Correction, 3% Sodium Chloride, Hypertonic Saline (PubMed Search)
Posted: 7/11/2024 by Wesley Oliver
Click here to contact Wesley Oliver
At our institution we have developed a guideline for the use of hypertonic saline in hyponatremia.
Administration of 3% sodium chloride for acute or symptomatic hyponatremia
Acute hyponatremia with severe symptoms
Acute hyponatremia with moderate symptoms
Hyponatremia Fluid Rate Calculations (**Be Careful with Online Calculators**)
FYI: 3% Sodium Chloride (1.95 mL/mEq; 513 mEq/1 L); 0.9% Sodium Chloride (6.5 mL/mEq; 154 mEq/1 L)
Equations for Calculations
***See Visual Diagnosis for an Example with Calculations***
Example:
70 kg male patient with a current sodium of 115 mEq/L (not hyperglycemic)
3% Sodium Chloride
0.9% Sodium Chloride
**Popular Online Calculator Using Same Example**
3% sodium chloride: 54 mL/hr
0.9% sodium chloride: 551 mL/hr
Be aware that the default setting of the calculator is to correct by 12 mEq/L over 24 hours leading to larger rates of infusion.
Adult Hypertonic Aline for Use in Hyponatremia, Medication Use Guideline. University of Maryland Medical System. Accessed July 2024.
Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines.
JASN. 2017; 28(5):1340-1349.
Jones GN, Bode L, Riha H et al. Safety of continuous peripheral infusion of 3% sodium chloride solution in neurocritical care patients. Am J Crit Care. 2017; 26(1): 37-42.
Sodium chloride preparations. Lexi-Drugs. Lexicomp. Wolters Kluwer Health, Inc. Riverwoods, IL. Available at: http://online.lexi.com. Accessed June 2018.
Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatremia. Intensive Care Med. 2014; 40:320-331.
Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, Evaluation and Treatment of Hyponatremia: Expert Panel Recommendations. Amer J Med. 2013; 126:S1-S42.
Category: Gastrointestional
Keywords: analgesia (PubMed Search)
Posted: 7/10/2024 by Neeraja Murali, DO, MPH
(Updated: 7/27/2024)
Click here to contact Neeraja Murali, DO, MPH
I don't know about you, but I'm always eager to hear new and alternative methods of pain control…
This study examined the effectiveness of transcutaneous electrical nerve stilumlation (TENS) in patients with abdominal pain. Patients were randomized to TENS or sham applied to the abdomen. The primary outcome of interest was change in pain score 30 min after the intervention, and secondary outcome was percentage of patients requiring rescue analgesia. Pain scores were measured on a verbal numeric score scale with a range from 0 to 10, with any adult patients with a minimum score of 5 being eligible.
The mean reductions in pain scores after the intervention were also similar in patients treated with TENS and sham TENS (1.9 vs. 1.7 respectively, p = 0.81). THe use of rescue analgesia was 49% in patients treated with TENS and 51% in those who received sham TENS (p=0.66). No adverse events were noted.
The authors did note that there is a challenge in blinding due to toeh absence of electrical stimulation in the sham group; nonetheless, TENS was not found to be more effective than sham. It also did not reduce the need to rescue analgesia.
Guess I'll keep looking…
McMahon B, Prabhu A, Thode HC Jr, Singer A. Transcutaneous electrical nerve stimulation (TENS) versus sham TENS in adult ED patients with abdominal pain: A clinical trial. Am J Emerg Med. 2024;76:7-12. doi:10.1016/j.ajem.2023.10.035
Category: Critical Care
Keywords: Corticosteroids, septic shock, ARDS, acute respiratory distress syndrome, community acquired pneumonia, CAP, dexamethasone, methylprednisolone, hydrocortisone (PubMed Search)
Posted: 7/9/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
This May, the Society of Critical Care Medicine (SCCM) published new recommendations [1] for the use of corticosteroids in critical illness (separate from patients with known adrenal insufficiency or on chronic steroids), namely:
Bottom Line:
For severe bacterial pneumonia and septic shock, ED physicians should feel comfortable administering a dose of hydrocortisone 50mg IV as hydrocortisone 200mg/day is an accepted regimen for these disease processes.
For patients with ARDS who remain boarding in the ED, EM docs should discuss initiation of steroids with their intensivists, whether the institutional preference is for dexamethasone 20mg IV (per DEXA-ARDS) [6] or methylprednisolone 1mg/kg/day (per Meduri)[7].
Category: Ultrasound
Keywords: POCUS, GI, SBO (PubMed Search)
Posted: 7/8/2024 by Alexis Salerno, MD
Click here to contact Alexis Salerno, MD
POCUS has been shown to have a 92.4% sensitive (95% CI 89.0% to 94.7%) and 96.6% specific for identifying SBO.
Some characteristics of SBO include:
-dilated fluid filled bowel
-contents of bowel moving to and fro like a washer machine
-wall thickening and ability to see plicae circulares
- in high grade obstruction you may also notice intraperitoneal fluid near the dilated bowel.
Gottlieb M, Peksa GD, Pandurangadu AV, Nakitende D, Takhar S, Seethala RR. Utilization of ultrasound for the evaluation of small bowel obstruction: A systematic review and meta-analysis. Am J Emerg Med. 2018 Feb;36(2):234-242. doi: 10.1016/j.ajem.2017.07.085.
Category: Trauma
Keywords: facial trauma, orbit, fracture (PubMed Search)
Posted: 7/7/2024 by Robert Flint, MD
(Updated: 7/27/2024)
Click here to contact Robert Flint, MD
Patient struck in left eye. The patient was asked to look up during exam and this is the finding. What imaging modality would you order if so inclined, what is the injury, and what is the disposition/plan?

Concern for a left orbital “blowout” fracture with muscle entrapment. Also called the trapdoor fracture. CT is the imaging modality of choice not plain films. This injury requires emergent consultation with a face surgeon (plastics, ENT or oculoplastics.). Right orbital fracture in the photo below.
-668ade5e780f0.jpg)
1.https://www.researchgate.net/figure/Girl-with-blowout-fracture-of-the-left-orbit-and-enophthalmos_fig1_351847537
2.|The Lancet. VOLUME 395, ISSUE 10221, P370, FEBRUARY 01, 2020
Paul Geraeds Kemps, BSc Michaël Herman Frank, MD
Published: February 01, 2020DOI:https://doi.org/10.1016/S0140-6736(19)33223-4
Category: Orthopedics
Keywords: Hip fracture (PubMed Search)
Posted: 7/6/2024 by Robert Flint, MD
(Updated: 7/27/2024)
Click here to contact Robert Flint, MD
Category: Pediatrics
Keywords: pediatrics, electrolyte, potassium (PubMed Search)
Posted: 7/5/2024 by Kathleen Stephanos, MD
Click here to contact Kathleen Stephanos, MD
Hypokalemia is a common electrolyte abnormality found in pediatric patients. The cut off for low potassium is based on age, with young infants having higher baseline levels of potassium when compared to older children and adults. The most common cause of hypokalemia in children is GI losses (diarrhea), though other considerations include malnutrition, congenital adrenal hyperplasia, renal abnormalities and medication effects.
Typically, hypokalemia is well tolerated, and the focus of management is based on treating the underlying cause, rather than repleting the potassium.
Medications should ONLY be initiated in patients who have potassium levels < 3.0 mmol/L OR with those with levels < 3.5 mmol/L with ECG changes.
In patients receiving treatment, oral potassium administration is typically recommended unless any of the following criteria are met:
In these patients IV potassium should be given (typically KCl at 0.5-1mEq/kg/DOSE - Max of 40 mEq/dose).
Just like in adults, ALL patients require continuous cardiac monitoring when receiving potassium infusions.
Brown DH, Paloian NJ. Hypokalemia/Hyperkalemia and Hyponatremia/Hypernatremia. Pediatr Rev. 2023 Jul 1;44(7):349-362. doi: 10.1542/pir.2021-005119. PMID: 37391630.
Category: Obstetrics & Gynecology
Posted: 7/4/2024 by Michele Callahan, MD
(Updated: 7/27/2024)
Click here to contact Michele Callahan, MD
Spontaneous coronary artery dissection (SCAD) occurs when there is an intimal tear that develops within the wall of an epicardial coronary artery, leading to intramural hematoma and false lumen formation with compromised coronary blood flow. This tear develops in the absence of atherosclerosis, trauma, or iatrogenic injury. SCAD is believed to account for 4% of acute coronary syndromes, and has been found to be the cause of ACS in 35% of women under the age of 50. Women comprise the majority of cases of SCAD( 87-95%).
Patients with Pregnancy-associated SCAD (P-SCAD) will often present with higher-risk features and more severe presentations compared with non-pregnancy related SCAD. They are more likely to present with STEMI (>>NSTEMI), impaired left ventricular function, left main and multivessel disease, and shock than other cohorts of SCAD patients.
The peak timing of P-SCAD is within the first month postpartum (with the highest incidence within the first week), although cases can occur throughout all trimesters of pregnancy or many months postpartum.
Keep SCAD in your differential for patients without typical risk factors who present with signs/symptoms of ACS. A strong index of suspicion is necessary to prevent bad outcomes and improve morbidity and mortality from this disease entity.
