Category: Ultrasound
Keywords: POCUS, GI, Hernia (PubMed Search)
Posted: 1/19/2026 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
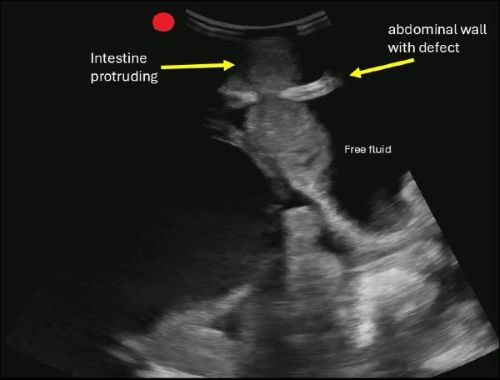
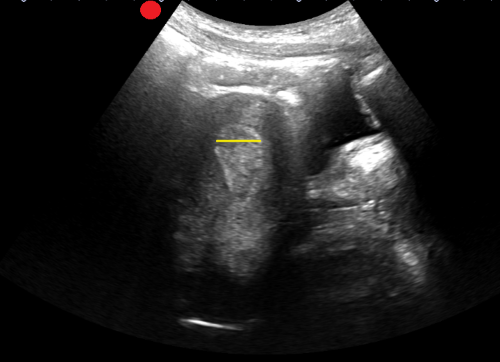
POCUS can help you identify signs of a hernia.
Begin by asking the patient to localize the point of maximal tenderness, then place a linear or curvilinear transducer over the area of concern. If there is concern for an inguinal hernia, you can have the patient perform a Valsalva maneuver while holding the probe in the area to evaluate dynamic changes.
A hernia is diagnosed when omental fat or intestinal contents are seen protruding through a defect in the abdominal wall.
If you are concerned about an incarcerated hernia, sonographic findings may include absence of peristalsis, presence of surrounding free fluid, with preserved blood flow on color Doppler. If a hernia progresses to strangulation, you may notice the absence of flow on color and power Doppler.
Boccatonda A, Brighenti A, Tiraferri V, Doglioli M, Iazzetta L, De Meis L, Safai Zadeh E, Dietrich CF, Serra C. POCUS for acute abdominal pain: practical scan protocols on gastrointestinal diseases and an evidence review. J Ultrasound. 2025 Dec;28(4):851-871. doi: 10.1007/s40477-025-01088-7.
Category: Ultrasound
Keywords: POCUS, arterial occlusion, limb ischemia (PubMed Search)
Posted: 1/5/2026 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be a valuable tool for screening both peripheral venous and arterial pathology.
If you suspect critical limb ischemia, you can use a similar approach to venous evaluation to assess for arterial occlusion.
Evaluate for:
Conclusion: POCUS can expedite diagnosis and resources prior to definitive testing with CT angiography.
Gonzalez AA, Brenner DS. Arterial Thrombosis Diagnosed With Point-of-Care Ultrasound. Cureus. 2024 Sep 13;16(9):e69357. doi: 10.7759/cureus.69357.
Frederick MK, Stolz LA, Duran-Gehring PE. Vascular Ultrasound. Emerg Med Clin North Am. 2024 Nov;42(4):805-818. doi: 10.1016/j.emc.2024.05.011.
Drake A, Dreyer N, Hoffer M, Boniface K. Point-of-care Ultrasound for the Evaluation of Acute Arterial Pathology in the Emergency Department: A Case Series. Clin Pract Cases Emerg Med. 2022 Feb;6(1):1-7. doi: 10.5811/cpcem.2021.11.54904.
Category: Ultrasound
Keywords: dental infection; POCUS (PubMed Search)
Posted: 12/15/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
Dental pain is a common reason for emergency department visits. These patients often experience prolonged length of stay and additional radiation exposure while awaiting CT imaging of the face. A recent case study highlights the potential role of POCUS in evaluating suspected dental abscesses.
In this report, clinicians used a high-frequency linear probe placed externally along the jawline. By orienting the probe to visualize the bony cortex of the mandible or maxilla and the dental root insertion, they identified a hypoechoic collection abutting the bone. When absent on the contralateral side and interpreted in the appropriate clinical context, this finding can suggest an abscess.
For further details, including imaging examples and technique demonstrations, see the referenced article and supplemental videos.
Hoffer JT, Park R, Brenner DS. "Is My Face Swollen?"-Utilizing Point-of-Care Ultrasound to Diagnose Odontogenic Infections. J Emerg Med. 2025 Oct 25;80:165-176. doi: 10.1016/j.jemermed.2025.10.032.
Category: Ultrasound
Keywords: POCUS, testicular pain (PubMed Search)
Posted: 12/1/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
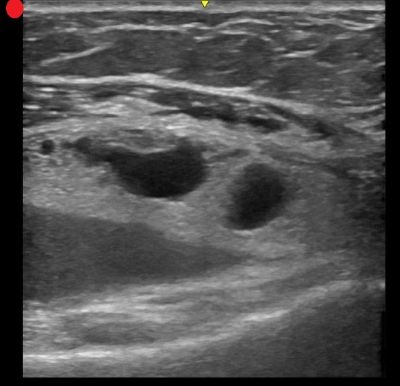
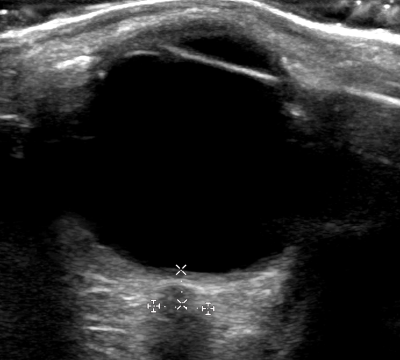
POCUS can be performed at the bedside to evaluate for acute scrotal conditions, including testicular torsion and inflammatory processes such as epididymo-orchitis.
A high-frequency linear transducer is typically used to scan the scrotum in two different planes. Additionally, a coronal "buddy view"—displaying both testes side by side—can aid in comparing echogenicity and vascularity.
On B-mode imaging, both testicular torsion and inflammatory conditions may present with testicular swelling and decreased homogeneity. However, color and power Doppler imaging can help to differentiate:
Inflammatory conditions (e.g., epididymo-orchitis) typically show increased vascular flow on color and power Doppler.
Testicular torsion usually demonstrates reduced or absent flow in the affected testis. However, in cases of intermittent torsion-detorsion, vascular flow may appear preserved or even increased. In such scenarios, repeat Doppler imaging after one hour may help clarify the diagnosis.
Kumar K, Kumari M, Kumar V, Suman SK. Evaluation of Scrotal Pathologies by Ultrasound and Color Doppler. Cureus. 2023 Mar 27;15(3):e36776. doi: 10.7759/cureus.36776
Acuña JG, Adhikari SR. Small Parts – Testicular Ultrasound. Sonoguide. American College of Emergency Physicians. Published April 1, 2025. Accessed December 1, 2025. https://www.acep.org/sonoguide/advanced/testicular
Category: Ultrasound
Keywords: POCUS; Pediatrics; Cardiology; left ventricular function (PubMed Search)
Posted: 11/3/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
E-point septal separation (EPSS)—the distance between the anterior mitral valve leaflet and the interventricular septum during early diastole—is a well-established marker of left ventricular (LV) systolic function in adults. A threshold of 7.0 mm is commonly used to screen for severely depressed LV function. But how well does this cutoff translate to pediatric populations?
A recent retrospective study set out to explore this very question. Researchers reviewed 770 pediatric echocardiograms, including 148 with abnormal LV function and a 4:1 random sample of normal studies. Using post-exam ultrasound software, blinded operators measured EPSS across three age groups: 0-3 years, 4-12 years and 13-18 years.
Results:
Among children with LV systolic dysfunction, EPSS values increased progressively with severity:
When applying the adult 7.0 mm threshold: Sensitivity: 76.4% (95% CI: 68.5–82.8%) Specificity: 95.8% (95% CI: 93.8–97.2%)
However, the study-derived optimal threshold of 6.0 mm improved sensitivity to 81.8% (95% CI: 74.4–87.4%) while maintaining high specificity at 91.4% (95% CI: 88.9–93.5%).
Special Consideration for the Youngest Patients
In children aged 0–3 years, a lower threshold of 4.9 mm outperformed the adult cutoff: Sensitivity at 4.9 mm: 77.8% (95% CI: 51.9–92.6%) vs sensitivity at 7.0 mm: 55.6% (95% CI: 31.3–77.6%)
While these findings are promising, further research is needed to validate EPSS thresholds in emergency department (ED) settings using point-of-care ultrasound (POCUS), and to assess their feasibility in real-time clinical workflows.
Bottom Line: For older children an EPSS threshold of 7.0 mm appears to be accurate in identifying children with LV systolic dysfunction, but a lower threshold may be needed for children ages 0-3. Further studies are needed.
Chen E, Ramgopal S, Lorenz D, Jone PN, Horowitz R. Use of e-point septal separation to screen for left ventricular function in children. Am J Emerg Med. 2025 Sep 6;99:39-45. doi: 10.1016/j.ajem.2025.09.013
Category: Ultrasound
Keywords: CPR, POCUS, pulse checks (PubMed Search)
Posted: 10/6/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
A recent systematic review compared the timing and diagnostic accuracy of manual pulse check versus point-of-care ultrasound (POCUS) pulse checks (this means placing an ultrasound probe on the carotid or femoral artery to evaluate for a doppler pulse).
The review included seven studies encompassing a total of 469 patients.
Six of the studies assessed the duration of pulse checks, revealing a mean time difference of –1.39 seconds (95% CI: –2.20 to –0.57) in favor of ultrasound.
Three of the studies reported the sensitivity and specificity of POCUS pulse checks, yielding pooled estimates of 99% sensitivity (95% CI: 87%–100%) and 96% specificity (95% CI: 85%–99%). In contrast, two studies evaluated manual pulse checks, with pooled sensitivity of 62% (95% CI: 22%–91%) and specificity of 91% (95% CI: 88%–93%).
As with many systematic reviews, the studies included demonstrated high heterogeneity and generally low methodological quality, indicating that further investigation may still be needed.
Neto ES, Scapin M, Lazaro-Paulina F, Campbell RL, Molinari DF, Kummer T. Duration of resuscitation interruption using point-of-care ultrasound versus traditional manual pulse check: A systematic review and meta-analysis. Am J Emerg Med. 2025 Aug 23;98:145-152. doi: 10.1016/j.ajem.2025.08.049.
Category: Ultrasound
Keywords: Bladder Ultrasound, Foley, POCUS (PubMed Search)
Posted: 9/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
If a patient is experiencing issues with their Foley catheter, consider using POCUS.
Using a curvilinear probe over the suprapubic region, you can obtain a transverse view of the bladder by orienting the marker towards the patient’s right side, or a sagittal view by orienting the marker towards the patient’s head.
In a properly functioning Foley, the bladder will appear decompressed, and you may only see the Foley balloon.
In cases of obstruction or malposition, you may notice a distended bladder. The next step is to attempt to visualize the Foley balloon. If you do not see a Foley balloon within the bladder, try deflating the balloon and advancing the catheter.
If you notice debris blocking the foley or heterogenous material in a patient with hematuria, you can attempt to flush the catheter, but if the patient has a large amount of hematuria, you may need to replace the current Foley with a three-way catheter for continuous bladder irrigation.
Boivin Z, Li JJ, Gottlieb M, Liu RB. Troubleshooting Foley Catheter Problems using Point-of-Care Ultrasound, Journal of Emergency Medicine (2025). doi.org/10.1016/j.jemermed.2025.07.049
Category: Ultrasound
Keywords: POCUS; Pulmonary Embolism; Cardiac Ultrasound; Doppler (PubMed Search)
Posted: 7/21/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
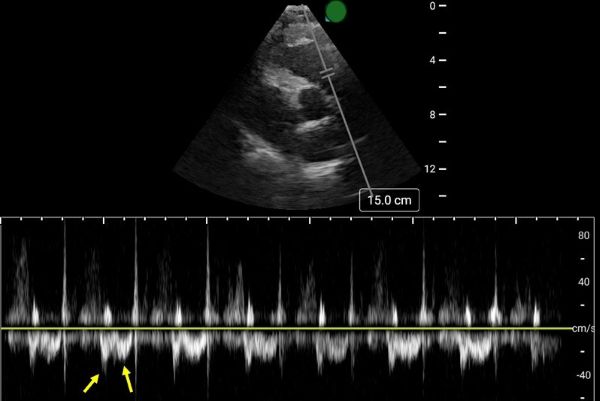
Early Systolic Notching and Pulmonary Embolism
A prospective multicenter study conducted across four academic emergency departments in Turkey evaluated the diagnostic accuracy of early systolic notching (ESN) in emergency department patients. Among the 183 patients included, 52.5% were diagnosed with pulmonary embolism (PE), while 19.7% exhibited the ESN finding. ESN demonstrated a sensitivity of 34% (95% CI: 25–45%) and a specificity of 97% (95% CI: 90–99%) for PE. Sensitivity increased to 69% in patients classified as high or intermediate-high risk. Overall, ESN exhibits moderate to high specificity but low sensitivity, consistent with other sonographic signs of PE. Notably, ESN may also be present in patients with chronic thromboembolic disease secondary to prior pulmonary hypertension.
How to Obtain ESN
To detect ESN, acquire a parasternal short axis view at the base of the heart to visualize the right ventricular outflow tract and pulmonic valve. Position the pulse wave Doppler gate just proximal to the pulmonic valve, with the cursor traversing the outflow tract. ESN is characterized by a sharp systolic spike with a notch, followed by a dome-shaped waveform
Aslaner MA, Karbek Akarca F, Aksu ?H, Yazla M, Can Ö, Ku? G, Çelik A, Özkan S, ?bze S, Yamano?lu A, Yaz?c? MM, Yürüktümen Ünal A, Demircan A. Diagnostic Accuracy of Early Systolic Notching in Pulmonary Embolism. J Ultrasound Med. 2022 Mar;41(3):637-644. doi: 10.1002/jum.15744.
Category: Ultrasound
Keywords: POCUS, MSK, finger injuries, nerve blocks (PubMed Search)
Posted: 7/7/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
Digital nerve blocks are commonly used to provide anesthesia for finger injuries such as lacerations and dislocations. However, the procedure can be painful, as it often requires multiple injections into sensitive areas.
A recent single-center, unblinded randomized study compared the subjective discomfort and analgesic efficacy of traditional digital nerve blocks with ultrasound-guided peripheral nerve blocks. The study included 106 patients, with 53 in each group.
Results showed that patients in the peripheral nerve block group reported higher satisfaction rates. They also experienced less pain during the initial injection and longer-lasting analgesia compared to those who received digital nerve blocks. While digital blocks had a faster onset of anesthesia, they were associated with a higher rate of block failure.
Chororia, Samata et al. Dorsal Digital Nerve Block vs. Ultrasound-Guided Selective Peripheral Nerve Block for Finger Analgesia: A Randomized Controlled Study. Journal of Emergency Medicine. Article in Press. doi: 10.1016/j.jemermed.2025.05.005.
Category: Ultrasound
Keywords: POCUS, Hip Effusion, MSK (PubMed Search)
Posted: 6/16/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A hip effusion can cause pain with leg movement in both pediatric and adult patients.
A recent multicenter, prospective study assessed the diagnostic accuracy of POCUS performed by pediatric emergency physicians in detecting hip effusion.
They found that POCUS had a sensitivity of 89.3% (95% CI 80.6 to 95.0%) and specificity of 99.2% (95% CI 97.0 to 99.9%).
To scan the hip:
-Position the patient supine with the patient’s hip externally rotated.
-Place the probe transversely across the patient’s leg with the marker towards the patient’s right and scan proximally.
-Upon reaching the proximal femur, rotate the probe marker so it points towards the patient’s umbilicus.
-Look for an anechoic stripe at the femoral neck, preceding the femoral head.
An anechoic stripe measuring at least 5 mm in the anterior synovial space or an asymmetry exceeding 2 mm compared to the opposite, asymptomatic hip is diagnostic for hip effusion in BOTH pediatric and adult populations.
Jones RM, Malia L, Snelling PJ, Riera A, Mak W, Moote D, Brimacombe M, Chicaiza H. Diagnostic Accuracy of Point-of-Care Ultrasound for Hip Effusion: A Multicenter Diagnostic Study. Ann Emerg Med. 2025 Jun 7:S0196-0644(25)00279-3. doi: 10.1016/j.annemergmed.2025.04.033. Epub ahead of print. PMID: 40481828.
Category: Ultrasound
Keywords: soft tissue; point of care ultrasound (PubMed Search)
Posted: 5/19/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
When evaluating foreign bodies in soft tissue, an imaging interface- such as a standoff pad- can improve imaging of superficial structures.
Common image interfaces include gel, commercial standoff pads, saline bags, and water baths.
Water baths are primarily used for imaging the hands and feet, but a recent study explored a water-filled patient belongings bag as a novel alternative. This method gives the benefit of the same elevated standoff that water baths provide, while accommodating larger extremities that may not fit in traditional setups.
The study found no significant difference between the patient belonging bag and a water bath for identifying a FB in a porcine model. Saline bags had the lowest image quality.
Vega C, Lindsay R, Shokraneh K, et al.. POCUS Standoff: Comparing Ultrasound Interfaces for Soft Tissue Foreign Body Imaging. Pediatric Emergency Care. 2025; 41 (5): 354-358. doi: 10.1097/PEC.0000000000003359.
Category: Ultrasound
Keywords: Point-of-care ultrasound; Cholecystitis; Gallbladder distention; Biliary ultrasound (PubMed Search)
Posted: 5/5/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
The normal gallbladder dimensions on ultrasound are approximately 3 cm in width by 10 cm in length.
A recent study evaluated the diagnostic test characteristics of gallbladder distension on POCUS for cholecystitis.
The authors conducted a retrospective cohort study of 227 patients who were admitted to the hospital after undergoing a POCUS biliary study in the emergency department.
They found the prevalence of gallbladder distension to be 30% in their study population. When combined with other sonographic findings, the presence of distension increased the specificity for cholecystitis to 95.6%.
Gallbladder wall distension was associated with the presence of an obstructing stone in the gallbladder neck and with acute cholecystitis.
Additionally, gallbladder wall distension was associated with longer operative times (mean 114 minutes) compared to those without distension (mean 89 minutes; p=0.03), suggesting more severe disease and potentially more complex surgical intervention.
Bottom Line: When gallbladder wall distension is present, it is important to carefully evaluate the gallbladder neck for signs of an obstructing stone.
Cannata D, Chin KA, Anslip A, et al. Association of biliary distention with a diagnosis of acute cholecystitis. Am J Emerg Med. 2024 Jul;81:130-135. doi: 10.1016/j.ajem.2024.04.056.
Category: Ultrasound
Keywords: POCUS; GI; Diverticulitis (PubMed Search)
Posted: 4/7/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A recent systematic review and meta-analysis evaluated the diagnostic accuracy of ultrasound in detecting acute diverticulitis. The analysis included 12 studies with a total of 2,056 patients. Ultrasound demonstrated a sensitivity of 92.5% (95% CI: 86.9%–95.8%) and a specificity of 87.7% (95% CI: 75.7%–94.2%).
The most commonly used diagnostic criteria across the studies included:
Similar to prior research on POCUS for nephrolithiasis, these findings support a POCUS-first approach for patients at low risk for serious alternative diagnoses. Ultrasound is a great alternative for patients with contraindications to contrast-enhanced CT, such as those with contrast allergies.
As the authors state, while ultrasound may be effective in identifying acute diverticulitis and its complications, such as abscess, additional imaging with CT may still be required to assess the severity of complications.
Shokoohi H, Peksa GD, Hutchison A, Al Jalbout N, Montoya K, Westrick JC, Goldsmith A, Nazerian P, Gottlieb M. Ultrasound accuracy in acute diverticulitis: A systematic review and Meta-analysis. Am J Emerg Med. 2025 Mar 10;92:96-103. doi: 10.1016/j.ajem.2025.03.002.
Category: Ultrasound
Keywords: POCUS; MSK; fracture (PubMed Search)
Posted: 3/17/2025 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
On ultrasound, lipohemarthrosis—the presence of blood and fat in the joint cavity—is a key clinical indicator of an intra-articular fracture.
Lipohemarthrosis appears as three distinct layers near the joint line.
Salerno A. Lipohemarthrosis. Floating fat in an intra-articular fracture. Visual Journal of Emergency Medicine. 2022, 26:101236.
Category: Ultrasound
Keywords: POCUS, OB, retained products of conception (PubMed Search)
Posted: 3/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A recent study evaluated the accuracy of POCUS in detecting retained products of conception (RPOC) in the emergency department.
In this study, a patient was considered positive for RPOC if they had heterogenous material in the endometrium measuring 10 mm or more. Color Doppler was not used for further evaluation, though it has been cited in obstetric literature as a helpful tool.
Among the 265 patients included, the prevalence of RPOC was 21.5%. POCUS had a sensitivity of 79.0 % and a specificity of 93.8 %.
The authors caution against the use of POCUS to diagnose RPOC in the setting of early pregnancy, as the endometrium can have a variable appearance, increasing the risk of a misdiagnosis. Of the 22 false positives identified, more than half were potentially viable pregnancies. Uterine fibroids can also lead to a heterogenous appearance of the uterus and can be another potential false positive.
Boivin Z, Barber D, Chimileski B, et al. Accuracy of point-of-care ultrasound in diagnosing retained products of conception. Am J Emerg Med. 2025;90:65-70. doi:10.1016/j.ajem.2025.01.032.
Category: Ultrasound
Keywords: ONSD, POCUS, ocular exam, intracranial pressure (PubMed Search)
Posted: 2/24/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Point-of-care ultrasound (POCUS) measurement of the optic nerve sheath diameter (ONSD) has been shown to correlate with increases in intracranial pressure (ICP).
In adults, an ONSD measurement of less than 5 mm is considered normal, while a measurement greater than 6 mm suggests elevated ICP.
How to Measure the Optic Nerve Sheath Diameter:
A small cross-sectional study examined whether ONSD measurements varied when taken at different depths. The findings indicated that ONSD increased by 0.32 mm at a depth of 4 mm and decreased by 0.54 mm at a depth of 2 mm.
These variations highlight the importance of maintaining a consistent measurement depth. To ensure accuracy and avoid misinterpretation, the ONSD should always be measured 3 mm posterior to the retina.
Gottlieb M, Kayarian F, Johnson J, Peksa GD. Differences in mean optic nerve sheath diameter measurements based on depth. Am J Emerg Med. 2024 Aug;82:197-198. doi: 10.1016/j.ajem.2024.06.013.
Category: Ultrasound
Keywords: aorta; POCUS; aortic dissection (PubMed Search)
Posted: 2/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
The suprasternal notch view is a valuable tool for assessing the aorta and identifying signs of thoracic aortic dissection. Proper technique is essential to obtain a clear image and improve diagnostic accuracy.
Steps to Obtain the Suprasternal Notch View:
Position the Patient:
Ideally, place the patient in a supine position.
If the patient cannot tolerate lying flat, the scan can be performed with the patient in an upright position.
Probe Selection & Orientation:
Use a phased array probe in cardiac mode.
Direct the probe marker slightly toward the patient’s left shoulder (or right hip if using abdominal mode).
Optimize Patient Positioning:
Ask the patient to extend their neck to improve visualization.
Having the patient rotate their head to the side may further enhance imaging.
Placing a rolled towel under the shoulders can help achieve optimal neck extension.
Probe Manipulation:
Angle the probe inferiorly toward the chest.
Adjust the depth to clearly visualize the aortic arch.
Kinnaman KA, Kimberly HH, Pivetta E, Platz E, Chudgar A, Adduci A, Stone MB, Rempell JS. Evaluation of the Aortic Arch from the Suprasternal Notch View Using Focused Cardiac Ultrasound. J Emerg Med. 2016 Apr;50(4):643-50.e1. doi: 10.1016/j.jemermed.2015.12.002.
Category: Ultrasound
Keywords: POCUS, ventricular arrythmia, nerve blocks (PubMed Search)
Posted: 1/20/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Stellate Ganglion Blocks (SGB) have been reported in case reports as a last-line treatment for patients with refractory ventricular arrhythmias.
A recent multicenter study evaluated the efficacy and safety of SGB in managing refractory ventricular arrhythmias.
The study included 117 critically ill patients, with 9 on ECMO, 5 with Impella devices, and 15 with LVADs.
70% were given long-acting bupivacaine, 28% were given ropivacaine and 1 patient received lidocaine.
SGBs were primarily performed by anesthesiologists during short periods of when the patients were not in ventricular arrhythmia
The median 24-hour episodes of VT/VF decreased from 9.0 (interquartile range [IQR]: 3.0–31.0) pre-SGB to 1.0 (IQR: 0.0–5.0) post-SGB.
2 patients had complications; recurrent laryngeal nerve block with resultant hoarseness and brachial plexus block.
Limitations: This study was conducted in a controlled setting (ie not in active arrest, not in the emergency department) and involved a selective cohort. Randomized controlled trials (RCTs) are needed to validate these findings.
Chouairi F, Rajkumar K, Benak A, Qadri Y, Piccini JP, Mathew J, Ray ND, Toman J, Kautzner J, Ganesh A, Sramko M, Fudim M. A Multicenter Study of Stellate Ganglion Block as a Temporizing Treatment for Refractory Ventricular Arrhythmias. JACC Clin Electrophysiol. 2024 Apr;10(4):750-758. doi: 10.1016/j.jacep.2023.12.012.
Category: Ultrasound
Keywords: POCUS, vascular access, pediatrics (PubMed Search)
Posted: 12/16/2024 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
In adult patients, ultrasound-guided long catheter IVs for difficult venous access have been shown to provide increased duration of use, reduced complication rates, and greater cost-effectiveness.
However, there are relatively few studies examining the use of ultrasound for IV access in pediatric patients.
A recent study, the DIAPEDUS study, investigated the success rate of peripheral IV access with and without ultrasound assistance in pediatric patients with difficult venous access.
The study included 110 pediatric patients. IVs were placed by 25 nurses and 6 pediatricians, each of whom had completed departmental training involving at least 20 ultrasound-guided IV placements prior to the study.
The results showed a significantly higher success rate on the first attempt with ultrasound-guided techniques (90% vs. 18%), along with reduced procedural time and fewer attempts overall.
Bottom Line: For patients with known difficult venous access, ultrasound-guided IV placement should be the first-line approach.
D'Alessandro M, Ricci M, Bellini T, Chianucci B, Calevo MG, Piccotti E, Moscatelli A. Difficult Intravascular Access in Pediatric Emergency Department: The Ultrasound-Assisted Strategy (DIAPEDUS Study). J Intensive Care Med. 2024 Mar;39(3):217-221. doi: 10.1177/08850666231199050
Bahl A, Johnson S, Hijazi M, Mielke N, Chen NW. Cost effectiveness of ultrasound-guided long peripheral catheters in difficult vascular access patients. J Vasc Access. 2024 Jul;25(4):1204-1211. doi: 10.1177/11297298231154297.
Category: Ultrasound
Keywords: POCUS, Lung ultrasound, EMS (PubMed Search)
Posted: 12/2/2024 by Alexis Salerno Rubeling, MD
(Updated: 1/31/2026)
Click here to contact Alexis Salerno Rubeling, MD
Early treatment of congestive heart failure (CHF) exacerbations is associated with improved mortality rates and shorter hospital length of stay. Lung ultrasound is a valuable tool in diagnosing CHF exacerbations. Recently, several studies have explored the use of lung ultrasound in the prehospital settings to expedite diagnosis and treatment.
A recent systematic review and meta-analysis evaluated the diagnostic accuracy and clinical impact of prehospital lung ultrasound. The authors found similar test characteristics to point-of-care ultrasound (POCUS) performed in the emergency department.
The eight studies included in the analysis utilized varying lung ultrasound protocols, analyzing between 2 and 8 lung zones. Notably, only two studies involved paramedics performing the ultrasounds, yet no significant difference in diagnostic accuracy was observed.
Further research is needed to evaluate the training requirements for prehospital providers and the broader impact of prehospital lung ultrasound on treatment strategies and patient outcomes.
