Category: Pediatrics
Keywords: CPR, peds, ventilation, BVM, compression ratio (PubMed Search)
Posted: 12/19/2025 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Pediatric CPR without an advanced airway in place requires 15 compressions to 2 ventilations per AHA and ILCOR guidelines. This can lead to a 2-4 second pause in compressions due to the time the ventilations take. The Maryland hiccup method is a novel description of two brief pauses for ventilations during the upstroke of compressions 14 and 15. This method was shown to improve the compression fraction and compressions per minute with no significant differences between standard CPR and the Maryland hiccup method in ventilation volume or compression depth determined on simulation mannequins. 38 Maryland EMS clinicians participated in this study.
A video demonstration of the Maryland Hiccup method is linked in the article and also available at: https://www.youtube.com/watch?v=RvFxhj7hzsQ .
Anders JF, Anderson C, Wright-Johnson C, O'Connell KJ. Improving the Quality of Pediatric Basic Life Support Cardiopulmonary Resuscitation With a Novel Method: The Maryland Hiccup. Cureus. 2025 Feb 9;17(2):e78783. doi: 10.7759/cureus.78783. PMID: 39931503; PMCID: PMC11808343.
Category: EMS
Keywords: altered mental status, trauma, EMS (PubMed Search)
Posted: 12/17/2025 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
EMS is taught to assess levels of consciousness through the Glasgow Coma Scale (GCS) and AVPU (alert/responsive to verbal stimuli/responsive to painful stimuli/unresponsive).
This study aimed to find a cut off point for where GCS and AVPU scales correlate. The National EMS Information System data set was used to look at over 4 million patient encounters that had both GCS and AVPU documented.
Lower AVPU scores correlated with life-sustaining procedures, including those for airway management, seizure, and cardiac arrest. Optimal GCS cut points obtained via a grid-based search were 14 to 15 for alert (A), 11 to 13 for verbal (V), 7 to 10 for pain (P), and 3 to 6 for unresponsive (U).
Ramgopal S, Horvat CM, Cash RE, Pelletier JH, Martin-Gill C, Macy ML. Comparing AVPU and Glasgow Coma Scales Among Children Seen by Emergency Medical Services. Pediatrics. 2024;154(2):e2024066168. doi:10.1542/peds.2024-066168
Category: Critical Care
Posted: 12/16/2025 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Pitfalls in Lactate Interpretation
Levy B, et al. Lactate dynamics as a marker of perfusion: physiological interpretation and pitfalls. Intensive Care Med. 2025; 51:2145-8.
Category: Ultrasound
Keywords: dental infection; POCUS (PubMed Search)
Posted: 12/15/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
Dental pain is a common reason for emergency department visits. These patients often experience prolonged length of stay and additional radiation exposure while awaiting CT imaging of the face. A recent case study highlights the potential role of POCUS in evaluating suspected dental abscesses.
In this report, clinicians used a high-frequency linear probe placed externally along the jawline. By orienting the probe to visualize the bony cortex of the mandible or maxilla and the dental root insertion, they identified a hypoechoic collection abutting the bone. When absent on the contralateral side and interpreted in the appropriate clinical context, this finding can suggest an abscess.
For further details, including imaging examples and technique demonstrations, see the referenced article and supplemental videos.
Hoffer JT, Park R, Brenner DS. "Is My Face Swollen?"-Utilizing Point-of-Care Ultrasound to Diagnose Odontogenic Infections. J Emerg Med. 2025 Oct 25;80:165-176. doi: 10.1016/j.jemermed.2025.10.032.
Category: Trauma
Keywords: shock, CAB, resuscitation, trauma, circulation (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/14/2025)
Click here to contact Robert Flint, MD
This review article reminds us that circulation needs to be prioritized over airway in trauma patients. This means bleeding control (pressure on wound, tourniquet, surgery/IR intervention), correcting tension pneumothorax, correcting pericardial tamponade, as well as resuscitation to return physiologic homeostasis (blood products, vasopressors where needed, warm the patient, etc.) before intubation. Altered mental status/low GCS may be due more to hypoperfusion than neurologic injury. Correcting the hypotension may alleviate that need to intubate.
Ferrada, Paula MD, FACS, FCCM, MAMSE; Duchesne, Juan MD, FACS, FCCM, FCCP; Piehl, Mark MD, MPH. Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 679-683, November 2025. | DOI: 10.1097/TA.0000000000004618
Category: Orthopedics
Posted: 12/13/2025 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Midshaft Clavicle Fractures
Have been in the sports headlines over the last several months
http://www.orthopaedicsone.com/wp-content/uploads/2024/06/379191373.png
About 3 - 3.5% of all adult fractures
Typical patient is young and active, usually males < 30 years old
Most clavicle fractures (up to 80%) involve the middle third
Mechanism: Typically direct impact or FOOSH
“S” shaped bone with thinnest & narrowest segment at junction between middle and distal third
Appearance: 2/3 non-displaced
Displaced fractures
Because of the effects of gravity, attempt to get clavicle series in upright position
Otherwise supine view may underestimate degree of displacement
What to look for on plain film
Displacement
Category: Pediatrics
Keywords: pediatric, bowel obstruction, ultrasound, volvulus, malrotation (PubMed Search)
Posted: 12/12/2025 by Kathleen Stephanos, MD
(Updated: 2/2/2026)
Click here to contact Kathleen Stephanos, MD
Malrotation is estimated to occur in 1 in every 500 children, and while many are asymptomatic, volvulus can occur resulting in a high rate of morbidity and mortality from ischemic bowel. Most of these patients will present within the first month of life.
Bilious emesis in an infant should immediately prompt consideration of this life-threatening condition, but what is the testing modality of choice?
While Fluoroscopic Upper GI Series (UGIS) has historically been looked to as the gold standard there are many issues with this method. It requires contrast, radiation exposure and an in-house radiologist to perform the imaging, oftentimes necessitating a transfer. Due to this, many algorithms have moved to Ultrasound (US) as the first test for these patients.
UGIS has a sensitivity for malrotation of 93-100%, but only as high as 89% for volvulus while US has a sensitivity and specificity of 94% and 100% respectively for midgut volvulus.
US findings suggestive of volvulus include the classic “whirlpool sign” with twisting of the superior mesenteric vein around the superior mesenteric artery seen on Doppler, dilated proximal duodenum, or free fluid in the abdomen.
So next time there is an infant presenting with bilious emesis, consider ultrasound as your first step to save a baby's bowel!
McCurdie FK, Meshaka R, Leung G, Billington J, Watson TA. Ultrasound for infantile midgut malrotation: Techniques, pearls, and pitfalls. Pediatr Radiol. 2024 Dec;54(13):2099-2111. doi: 10.1007/s00247-024-06067-4. Epub 2024 Oct 15. PMID: 39404889.
Category: Pharmacology & Therapeutics
Posted: 12/9/2025 by Ashley Martinelli
(Updated: 12/11/2025)
Click here to contact Ashley Martinelli
Sympathetic crashing acute pulmonary edema (SCAPE) is an acute, aggressive pulmonary edema that occurs in patients with hypertensive emergencies. Nitroglycerin (NTG) is often utilized in combination with non-invasive positive pressure ventilation to prevent decompensation; however, data is lacking regarding the optimal dosing strategy.
Study design: retrospective, single-center, cohort study at an academic medical center
Inclusion: adult patients with a primary or secondary diagnosis of pulmonary edema, acute heart failure exacerbation, hypertensive emergency, or hypertensive crisis and were initiated on NTG in the ED.
Exclusion: hypertensive emergency with different BP goals (dissection, eclampsia, ICH)
Study groups: based on initial NTG dose (<100 mcg/min = low dose, ? 100 mcg/min = high dose)
Primary outcome: time from NTG initiation to oxygen weaning (removal of necessary oxygen back to baseline or home oxygen
Baseline: 61 years old, 50% male, 97% with history of hypertension, 84% history of heart failure, and 36% with ESRD. A higher percentage of patients in the high dose group has CPAP/BIPAP (49% vs 27% p<0.001)
Results: High dose NTG group had a shorter time from NTG to oxygen wean of 2.67h compared to 3.28 hours in the low group. The high dose group also was more likely to achieve goal SBP reduction of 25% within the hour (55% v 34%, p<0.001) had a shorter duration of NTG infusion overall 4.9h vs 6.9h, p0.033) and had decreased ICU LOS by 0.5 days. There were more cases of hypotension in the high dose group which was primarily driven by acute drops in SBP >30%.
Bottom Line: Consider using NTG 100 mcg/min initially to manage patients with SCAPE in the ED.
Henry K, Pelsue B, Hartman H, Gulbis B. Low versus high dosing strategies of intravenous nitroglycerin for the management of sympathetic crashing acute pulmonary edema. Am J Emerg Med. 2025; 98:41-45.
Category: Gastrointestional
Keywords: TXA, GI bleeding (PubMed Search)
Posted: 12/10/2025 by Neeraja Murali, DO, MPH
(Updated: 2/2/2026)
Click here to contact Neeraja Murali, DO, MPH
A recent study in AJEM reviewed the utility of TXA in GI bleeding
This is a PRISMA?guided systematic review and meta?analysis of 7 RCTs (13,608 adults, 1976–2024) evaluating IV TXA vs placebo in acute gastrointestinal bleeding, including upper and mixed GI sources across multiple countries. The largest contributor is HALT?IT (Roberts et al.), which accounts for nearly 90% of participants.
-Mortality: No statistically significant reduction in all?cause mortality with TXA (OR 0.77; 95% CI 0.56–1.07, P = 0.12).?
-Rebleeding: TXA significantly reduced rebleeding events (OR 0.64; 95% CI 0.45–0.91, P = 0.01).?
-"Failure to control" bleeding: TXA reduced failure of hemostasis (OR 0.55; 95% CI 0.32–0.93, P = 0.03).
-Thromboembolic events: Random?effects model showed no significant difference (OR 1.28; 95% CI 0.51–4.51, P = 0.46), but fixed?effect analysis suggested a statistically significant increase (OR 1.28; 95% CI 1.07–1.55, P = 0.009), highlighting a possible thrombotic signal.?
-Transfusion and LOS: No significant reduction in blood transfusion requirements with TXA (OR 0.94; 95% CI 0.61–1.43, P = 0.76); length of stay and other resource metrics were variably reported and not clearly improved.
Take-Aways:
TXA may be reasonable as an adjunct in GI bleeding when the goal is to reduce rebleeding or “failure to control” bleeding, but current evidence does not support it as a mortality?reducing therapy.?
Given a potential increased risk of thromboembolic events, TXA should be used cautiously in patients with high baseline thrombotic risk, and always as part of a broader package including resuscitation and timely endoscopy rather than as a standalone intervention.
Djoudjou T, Alamri O, Aljuwayr A, et al. Intravenous tranexamic acid in gastrointestinal bleeding: A systematic review and meta-analysis of randomized controlled trials. Am J Emerg Med. 2025;97:175-182. doi:10.1016/j.ajem.2025.07.050
Category: Critical Care
Keywords: septic shock, capillary refill time, personalized medicine, fluids, vasopressors, resuscitation (PubMed Search)
Posted: 12/9/2025 by Jessica Downing, MD
Click here to contact Jessica Downing, MD
Last month, Mark Sutherland posted an overview of a new article investigating the use of personalized MAP targets in resuscitation for septic shock (1). Now, the authors of ANDROMEDA-SHOCK-2 (2) suggest a new multimodal approach to personalize resuscitation in septic shock that largely operates outside of the traditional focus on MAP and lactate.
In 2019, the ANDROMEDA-SHOCK Trial (3) suggested that capillary refill time (CRT) may be a better resuscitation in septic shock than lactate. Now, the same group is suggesting that a stepwise algorithm to guide resuscitation may provide more optimal and “personalized” results when compared to usual care for patients with abnormal CRT:
Tier 1: If CRT is abnormal, assess pulse pressure (PP) and DBP:
Tier 2: If CRT remains abnormal despite the above, use POCUS to assess for cardiac dysfunction.
The authors found that at 6 hours, following the protocol resulted in increased use of dobutamine, lower fluid balance, and similar CVP and MAP with lower lactate levels and CRT. They reported an improvement in their composite hierarchical outcome at 28 days, primarily driven by a shorter duration of organ support (vasoactives, mechanical ventilation, renal replacement therapy) and among sicker patients. No difference in mortality was observed between groups.
Food for Thought:
Study Details:
Category: Pediatrics
Keywords: Pediatrics, CT scans, PEM (PubMed Search)
Posted: 12/5/2025 by Taylor Lindquist, DO
(Updated: 2/2/2026)
Click here to contact Taylor Lindquist, DO
A large-scale retrospective study of 3.7 million children found an association between radiation exposure from medical imaging and a small but significantly increased risk of developing hematologic cancers (primarily leukemia).
Finding: Cancer risk increased with cumulative radiation dose
Dose-Response: For the highest exposure group (50 to <100 mGy), the Relative Risk (RR) for hematologic cancer was 3.59 compared to no exposure.
Attributable Risk: An estimated 10.1% of hematologic cancers in the cohort may have been attributable to medical imaging radiation, with CT scans being a major contributor.
Vulnerability: Children are more susceptible to radiation-induced cancer due to their heightened radiosensitivity and longer life expectancy for the cancer to manifest.
Take Away: Providers should critically assess the necessity of high-dose imaging like CT scans and use the lowest effective dose or possible alternative imaging (e.g. US, MRI, etc.) to prevent unnecessary cumulative exposure.
Medical Imaging and Pediatric and Adolescent Hematologic Cancer Risk. N Engl J Med. 2025 Oct 2;393(13):1269-1278. doi: 10.1056/NEJMoa2502098. Epub 2025 Sep 17. PMID: 40961449; PMCID: PMC12445590.
Category: Ultrasound
Posted: 12/3/2025 by Kerith Joseph, MD
(Updated: 12/4/2025)
Click here to contact Kerith Joseph, MD
Summary
Objective:
The study aimed to determine how a brief educational intervention could enable emergency medicine (EM) residents to use point-of-care ultrasound (POCUS) effectively to diagnose and manage shoulder dislocations in the emergency department (ED).
Methods:
Conducted at an academic teaching hospital in Miami, Florida.
Twenty EM residents (PGY1–PGY4) with no prior shoulder ultrasound training participated.
Residents received <1 hour of in-service training, including a short lecture, video instruction, and hands-on practice using a Sonosite M-Turbo ultrasound device.
Over one year (2016–2017), residents prospectively enrolled 78 adult patients with suspected shoulder dislocation.
POCUS findings were compared with x-rays (the gold standard) for accuracy.
Time to diagnosis and reduction confirmation were recorded.
Results:
55 of 78 patients were diagnosed with dislocation; 53 anterior, 1 posterior, 1 inferior.
POCUS achieved 100% sensitivity and specificity for diagnosing and confirming successful reductions compared to x-ray.
Ultrasound results were available ~22 minutes faster for diagnosis and ~27 minutes faster for reduction confirmation than x-rays (p < 0.0001).
Residents across all training years performed equally well.
POCUS also identified 14 fractures (12 confirmed by x-ray, 2 seen only on ultrasound).
Discussion:
A short educational session enabled residents to accurately use POCUS for shoulder dislocation diagnosis and management.
POCUS reduced diagnostic time, avoided radiation exposure, and may improve ED workflow and patient comfort.
Findings support including shoulder ultrasound as a core component of EM training, filling a current gap in national ultrasound education guidelines.
Limitations:
Convenience sample and single-center design.
Some selection bias and inherent limitations of POCUS-based studies.
Conclusion:
Emergency medicine residents can learn to diagnose and manage shoulder dislocations with excellent accuracy after brief ultrasound training. POCUS should be integrated into EM residency curricula as a core skill for musculoskeletal emergencies.
Category: Toxicology
Keywords: Nitrous Oxide, Whippit, unregulated psychotropic, inhalant abuse (PubMed Search)
Posted: 12/2/2025 by Kathy Prybys, MD
(Updated: 12/3/2025)
Click here to contact Kathy Prybys, MD

Vohra V, Matthews H, Stroh-steiner G. Notes from the field: Recreational Nitrous Oxide Use-Michigan, 2019-2023. MMWR Morb Mort Wkly Rep 2025;74:210-212. DOI: http://dx.doi.org/10.15585/mmwr.mm7412a3.
Gummin D, Mowry J, Beuhler MC, et.al (17 Dec 2024): 2023 Annual Report of the National Poison Data System® (NPDS) from America’s Poison Centers®: 41st Annual Report, Clinical Toxicology, DOI: 10.1080/15563650.2024.2412423
Yockey RA, Hoopsick RA. US Nitrous Oxide Mortality. JAMA Netw Open. 2025;8(7):e2522164. doi:10.1001/jamanetworkopen.2025.22164.
https://www.fda.gov/food/alerts-advisories-safety-information/fda-advises-consumers-not-inhale-nitrous-oxide-products. FDA Advises Consumers Not to Inhale Nitrous Oxide Products 6/4/2025
Category: Critical Care
Keywords: Shock, procedures, arterial line, blood pressure, mean arterial pressure, MAP (PubMed Search)
Posted: 12/2/2025 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
We have all been there – an ED patient with circulatory shock requiring vasoactive medications and, therefore, an arterial line for accurate and close monitoring of the MAP and appropriate titration of the infusions. But does it save lives?
The recently published NEJM article by Muller et al. takes a look at noninvasive BP monitoring (NIBP) by cuff versus early arterial catheterization in patients with hypotension and evidence of tissue hypoperfusion:
Bottom Line: This trial indicates that in appropriately-selected patients with shock, such as those not on high doses of vasopressors, with BMI < 40 and an ability to consistently obtain NIBP measurements, early arterial line placement in the ED for vasopressor titration is unlikely to improve outcomes. It is important to note other potential indications for arterial line placement (severe hypoxia, inability to obtain reliable SpO2 with need for ABG monitoring, cardiac arrest, pain related to NIBP cuff monitoring, intracranial hemorrhage, etcetera) may still make arterial line placement in the ED prudent and better for overall patient care.
*France refers to norepi by the tartrate formulation dose, US refers to the base norepi dose (ratio is 2:1 tartrate: base).
Muller G, Contou D, Ehrmann S, et al.; CRICS-TRIGGERSEP F-CRIN Network and the EVERDAC Trial Group. Deferring Arterial Catheterization in Critically Ill Patients with Shock. N Engl J Med. 2025;393(19):1875-1888. doi: 10.1056/NEJMoa2502136.
Category: Ultrasound
Keywords: POCUS, testicular pain (PubMed Search)
Posted: 12/1/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be performed at the bedside to evaluate for acute scrotal conditions, including testicular torsion and inflammatory processes such as epididymo-orchitis.
A high-frequency linear transducer is typically used to scan the scrotum in two different planes. Additionally, a coronal "buddy view"—displaying both testes side by side—can aid in comparing echogenicity and vascularity.
On B-mode imaging, both testicular torsion and inflammatory conditions may present with testicular swelling and decreased homogeneity. However, color and power Doppler imaging can help to differentiate:
Inflammatory conditions (e.g., epididymo-orchitis) typically show increased vascular flow on color and power Doppler.
Testicular torsion usually demonstrates reduced or absent flow in the affected testis. However, in cases of intermittent torsion-detorsion, vascular flow may appear preserved or even increased. In such scenarios, repeat Doppler imaging after one hour may help clarify the diagnosis.
Kumar K, Kumari M, Kumar V, Suman SK. Evaluation of Scrotal Pathologies by Ultrasound and Color Doppler. Cureus. 2023 Mar 27;15(3):e36776. doi: 10.7759/cureus.36776
Acuña JG, Adhikari SR. Small Parts – Testicular Ultrasound. Sonoguide. American College of Emergency Physicians. Published April 1, 2025. Accessed December 1, 2025. https://www.acep.org/sonoguide/advanced/testicular
Category: Infectious Disease
Keywords: sepsis, intrabdominal, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/30/2025)
Click here to contact Robert Flint, MD
Intraabdominal infections leading to sepsis can come from cholecystitis, small bowel perforation, gastric perforation, left sided colonic diverticulitis, right sided diverticulitis and appendicitis. When to initiate source control and antibiotics is controversial. These authors propose breaking patient populations into three groups:
From this they propose algorithms to treat these intraabdominal infections such as (note the different approach to right and left diverticulitis):
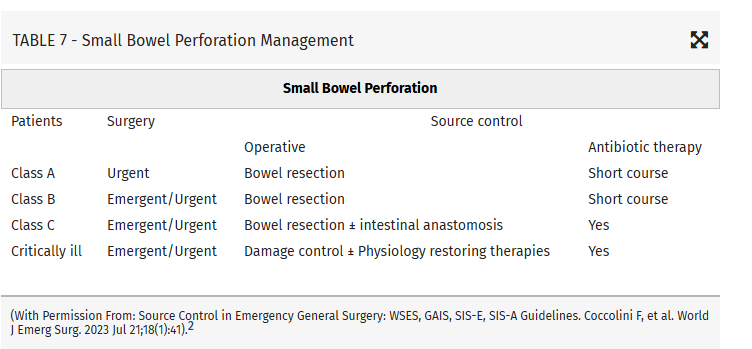
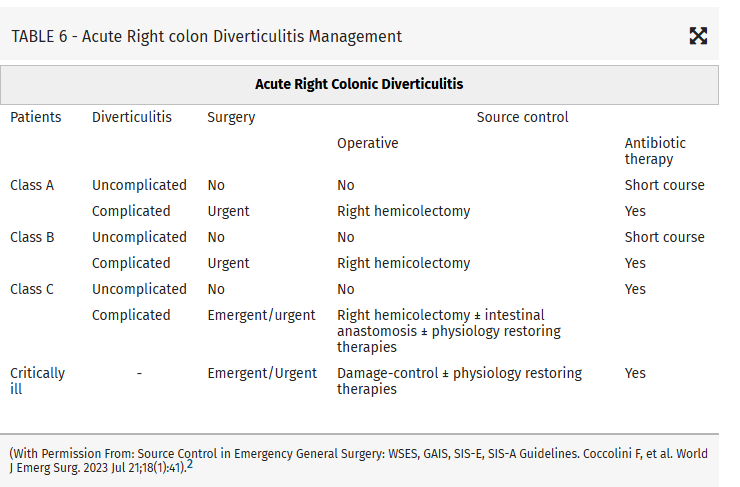
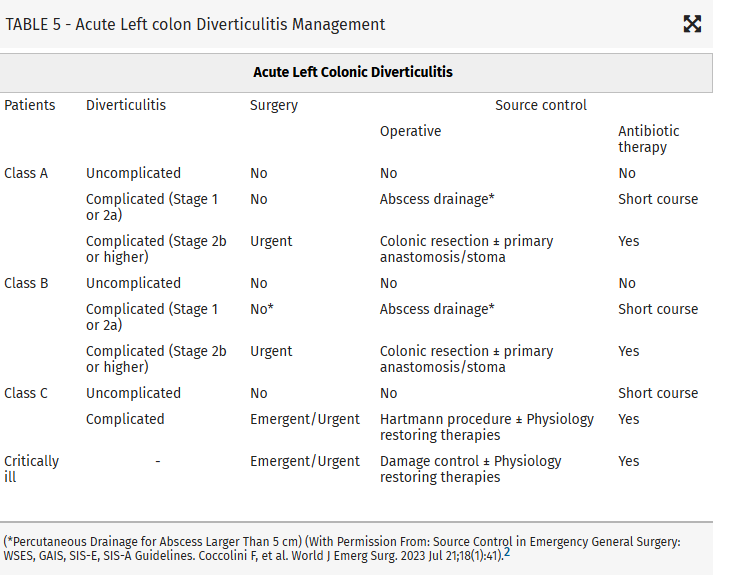
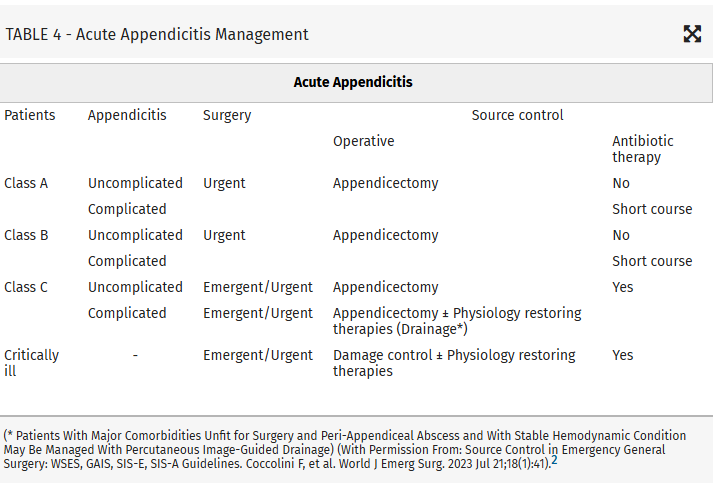
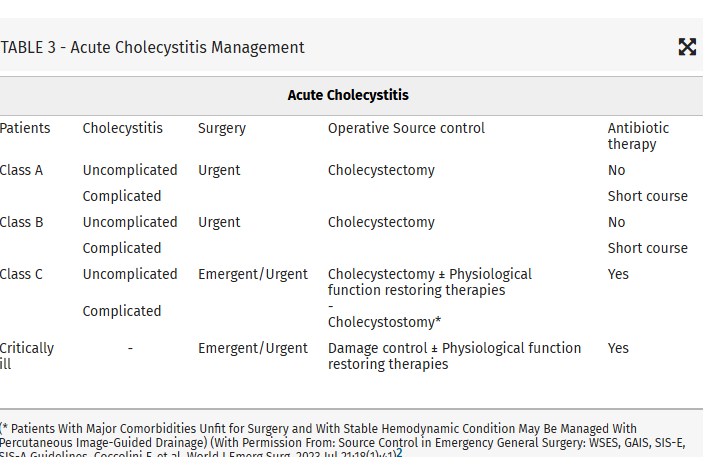
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Infectious Disease
Keywords: sepsis, intrabdominal source, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/29/2025)
Click here to contact Robert Flint, MD
This article looks at source control as it relates to intrabdominal sources for sepsis. Key take aways are:
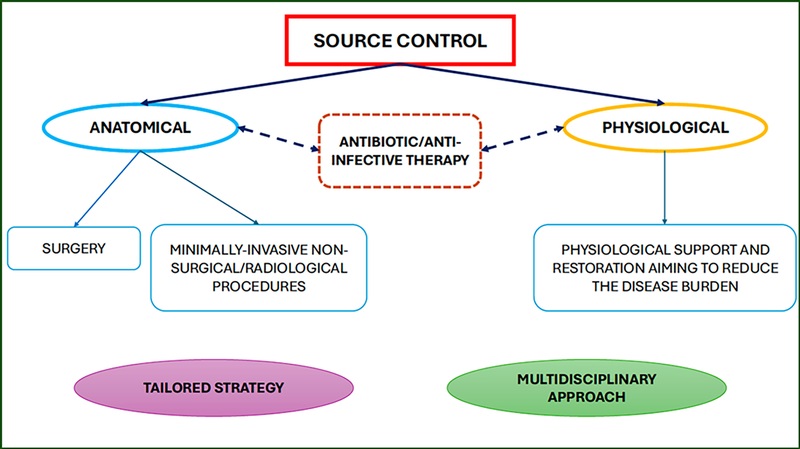
Those at high risk of morbidity and mortality from intraabdominal infection associated sepsis include:
Mild–moderate immune deficiency: Elderly (according to the age and general status of the patient), Malnourished, Diabetic, Burns, Trauma, Uremic, Active malignancy, not on chemotherapy, HIV with CD4+ count >200/mm3, Splenectomized, Severe immune deficiencyAIDS HIV with CD4+ count <200/mm3, Transplant (solid organ, bone marrow), High-dose steroids (more than 20 mg/day prednisone), Malignancy on chemotherapy, Neutrophil count <1,000/mm3
High-risk population (medical or surgical causes)Low serum albumin concentration Older age Obesity Smoking Diabetes mellitus Ischemia secondary to vascular disease or irradiation Prolonged or delayed/late procedures
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Misc
Keywords: prescribing, racial, disparity (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/28/2025)
Click here to contact Robert Flint, MD
Comparing prescribing patterns from early 2000s to late 2010s in the National Hospital Ambulatory Medical Care Survey, these authors found we continue to under prescribe pain medications to non-white patients for traumatic injuries.
Day, Jessica et al.
Journal of Emergency Medicine, Volume 78, 184 - 191
Category: Geriatrics
Keywords: frail, frailty scale, geriatrics, critical care (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/27/2025)
Click here to contact Robert Flint, MD
A prospective cohort of South Korean patients over 65 years admitted from the ED with critical illness had Clinical Frailty Scale (CFS) performed on them. Those with a high CFS had increased 3 month mortality. CFS helps us prognosticate morbidity and mortality in our older critically ill patients.
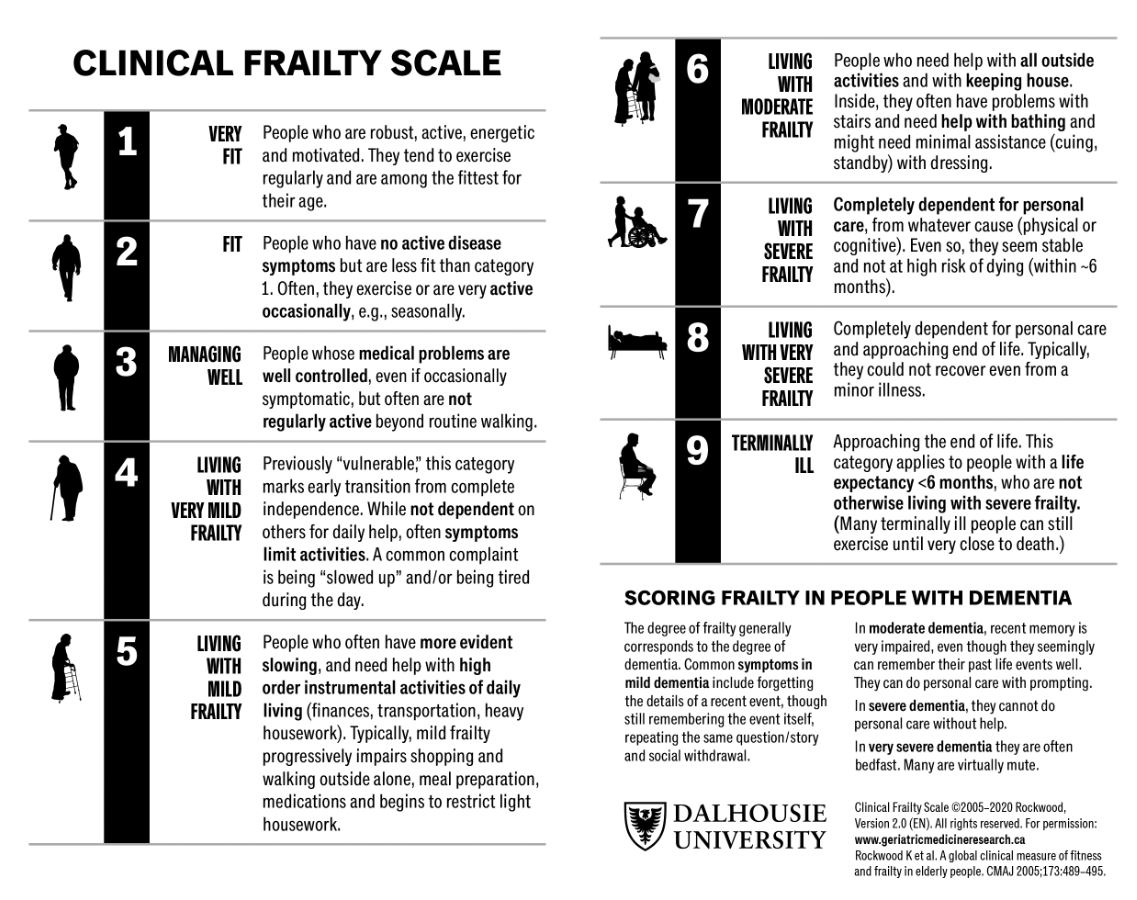
Um, Young Woo et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/26/2025 by Mercedes Torres, MD
(Updated: 2/2/2026)
Click here to contact Mercedes Torres, MD
Food for thought on this Thanksgiving eve…
AI is rapidly being integrated into the practice of emergency medicine, as well as many other medical specialties. Similar to the adage, "you are what you eat," AI is what we feed it. See below for an introduction to the various levels of bias contributing to the machine learning process:
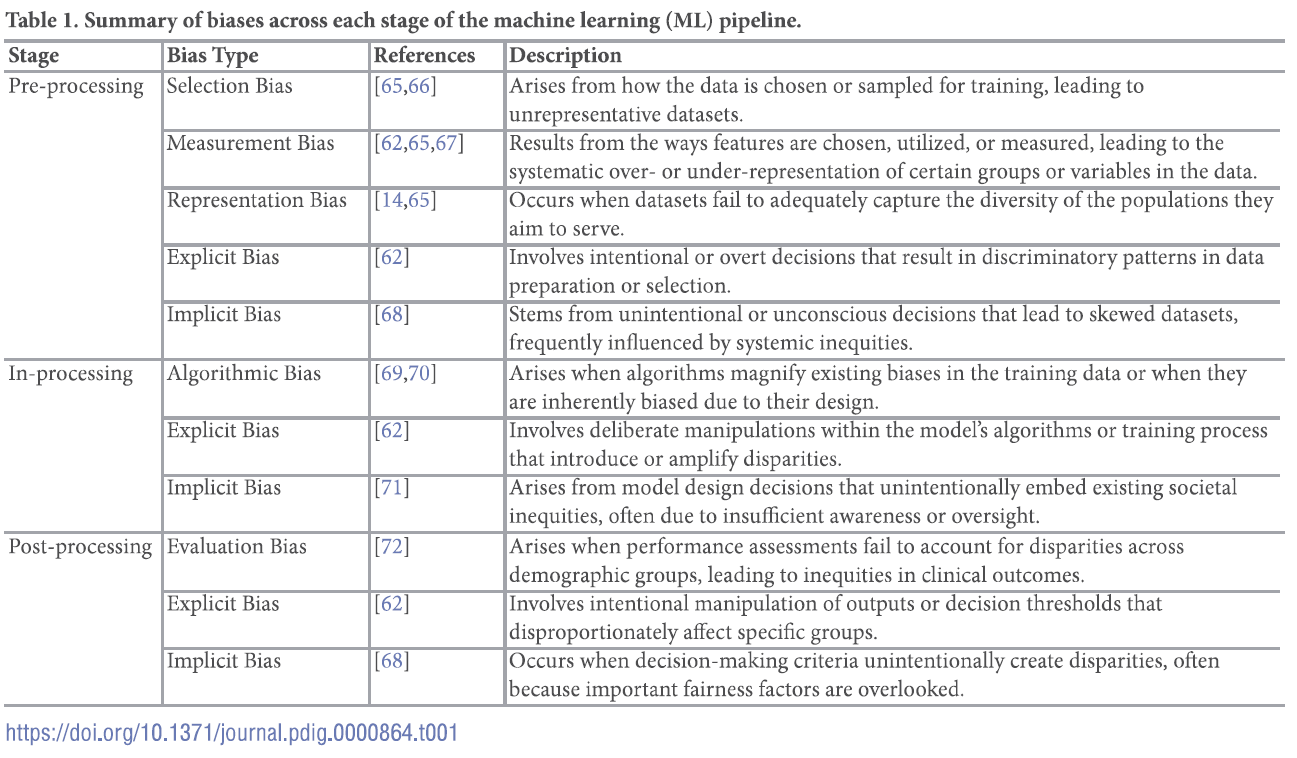
For a deep dive into the world of bias in AI, see referenced article.
Chinta SV, Wang Z, Palikhe A, Zhang X Kashif A, Smith MA, et al. (2025) AI-driven healthcare: A review on ensuring fairness and mitigating bias. PLOS Digit Health 4(5): e0000864. https://doi.org/10.1371/journal.pdig.0000864
