Category: Neurology
Keywords: CVA, blood pressure management, aggressive, edema (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 8/30/2025)
Click here to contact Robert Flint, MD
While this study is imperfect and may not be measuring patient important outcomes, it does fit with other literature on the topic of intensive blood pressure control in patients with acute ischemic stroke. These patients were randomized to aggressive blood pressure control (SBP 130-140 within 1 hour of TPA administration continued for 72 hours) or the standard SBP <180. Repeat imaging was performed to assess the degree of cerebral swelling that each group developed. There was no difference in swelling between the two groups.
Take away is aggressive blood pressure management in this group of ischemic stroke patients does not seem to be beneficial.
Zhang G, Chen C, Ren X, Zhao Y, Ouyang M, Billot L, Li Q, Wang X, Zhang L, Ong S, Liu L, You S, Lindley RI, Robinson TG, Li G, Chen X, Sui Y, Anderson CS, Song L; ENCHANTED Investigators. Effects of Intensive Blood Pressure Lowering on Brain Swelling in Thrombolyzed Acute Ischemic Stroke: The ENCHANTED Results. Stroke. 2025 Jun;56(6):1388-1395. doi: 10.1161/STROKEAHA.124.049938. Epub 2025 Apr 3. PMID: 40177745.
Category: Neurology
Keywords: stroke, positioning, LVO, thrombectomy (PubMed Search)
Posted: 8/12/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
The concept of positioning the head of bed flat in a patient with a neurologic catastrophe seems like a recipe for badness. For most neurologic emergencies, elevating the head of the bed (HOB) to 30° is standard to help control intracranial pressure and reduce aspiration risk. However, emerging evidence indicates that acute large vessel occlusion (LVO) stroke patients—particularly before thrombectomy—may be an important exception.
The ZODIAC trial, published in June of this year, was a prospective, randomized, multicenter study comparing 0° (flat) versus 30° HOB positioning in patients with confirmed LVO stroke awaiting endovascular thrombectomy. The rationale stems from physiologic studies, including transcranial Doppler ultrasonography, showing that flat positioning can improve cerebral perfusion to ischemic tissue.
The primary outcome was early neurologic deterioration (>2-point worsening in NIHSS prior to thrombectomy). Safety endpoints included hospital-acquired pneumonia and all-cause mortality at 3 months.
In the trial’s 92 enrolled patients, flat positioning markedly reduced early neurologic deterioration, which occurred in 2.2% in the 0° group versus 55.3% in the 30° group. There were no significant differences in pneumonia or 3-month all-cause mortality. The authors also found a statistically insignificant improvement in 90-day functional outcomes in the 0° group. Due to the magnitude of benefit, the study was stopped early at interim analysis.
This technique represents a simple, cost-free, and practical method of preventing neurologic decline ahead of definitive management for LVO. This may be especially beneficial for LVO patients who require interhospital transfer to a thrombectomy-capable center.
Bottom Line: For patients with LVO stroke awaiting thrombectomy, flat (0°) head positioning is safe and significantly reduces early neurologic decline by improving blood flow to ischemic brain tissue.
Category: Neurology
Keywords: ischemic stroke, thrombolysis, tpa, intracranial hemorrhage (PubMed Search)
Posted: 6/6/2025 by Nicholas Contillo, MD
(Updated: 2/1/2026)
Click here to contact Nicholas Contillo, MD
Acute ischemic strokes involving the posterior circulation have significantly lower rates of hemorrhagic transformation after thrombolysis compared to anterior circulation strokes, a difference attributed to smaller infarct sizes and greater “ischemic tolerance” in the posterior circulation.
Given this lower hemorrhage risk, the EXPECTS trial evaluated the safety and efficacy of extending the thrombolysis window to 4.5–24 hours in patients with acute posterior circulation ischemic stroke who were not candidates for endovascular thrombectomy. This randomized controlled trial, conducted across 30 sites in China, enrolled 234 adults with mainly mild posterior circulation stroke (median NIHSS 3) and no evidence of extensive infarction on CT. Participants were randomized to receive either intravenous alteplase or standard medical care within the 4.5–24 hour window after symptom onset.
The primary outcome of functional independence at 90 days (modified Rankin Scale 0–2) was achieved in 89.6% of the alteplase group versus 72.6% of the standard care group. Rates of symptomatic intracranial hemorrhage were low and similar between groups (1.7% alteplase vs. 0.9% standard care), and 90-day mortality was lower in the alteplase group (5.2% vs. 8.5%).
These findings support extending the therapeutic window for intravenous thrombolysis in posterior circulation stroke beyond 4.5 hours when thrombectomy is not an option. However, the trial’s limitations, including a study population predominantly with mild strokes, exclusion of patients with extensive infarction, and enrollment limited to Chinese centers, warrant further investigation in larger and more diverse populations.
Bottom Line: Within limitations, emerging evidence supports an extended thrombolytic window beyond 4.5 hours for patients with posterior circulation strokes who are ineligible for thrombectomy.
Yan S, Zhou Y, Lansberg MG, Liebeskind DS, Yuan C, Yu H, Chen F, Chen H, Zhang B, Mao L, Zhang X, Wang X, Zhang X, Chen Y, Zhou H, Zhong W, He Y, Chen K, Wang J, Chen H, Huang Y, Campbell BCV, Lou M; EXPECTS Group. Alteplase for Posterior Circulation Ischemic Stroke at 4.5 to 24 Hours. N Engl J Med. 2025 Apr 3;392(13):1288-1296. doi: 10.1056/NEJMoa2413344. PMID: 40174223.
Category: Neurology
Keywords: Seizure, pediatrics, ketamine (PubMed Search)
Posted: 5/31/2025 by Visiting Speaker
(Updated: 2/1/2026)
Click here to contact Visiting Speaker
Author: Matthew Jackson, MD
The Ket-Mid Study (1) is a recent RCT out of a tertiary center in a largely rural region of Egypt that evaluated combined ketamine (2 mg/kg) and midazolam (0.2 mg/kg) (ket-mid) to midazolam plus placebo (pla-mid) as the first line seizure abortive therapy. Children in the ket-mid group achieved 76% termination at 5 minutes compared to 21% of those in the pla-mid group (p<0.001). Adverse outcomes were rare, though the pla-mid group did have more hypotension.
Notably, the population included differed from that typically seen in the US. These kids were seizing for a long time, with a median seizure duration before IV meds of 34 minutes, and the benefit of ketamine on subgroup analysis seemed to shrink for those that were treated in less than 30 minutes. CNS infections were also much more common, accounting for the underlying pathology in 11% of cases. Important exclusion criteria also included trauma, inborn errors of metabolism, underlying CNS malignancy, and others not always known to EMS or ED clinicians at the time therapy begins.
1. Othman AA, Sadek AA, Ahmed EA, Abdelkreem E. Combined Ketamine and Midazolam Versus Midazolam Alone for Initial Treatment of Pediatric Generalized Convulsive Status Epilepticus (Ket-Mid Study): A Randomized Controlled Trial. Pediatr Neurol. 2025 Jun;167:24-32. doi: 10.1016/j.pediatrneurol.2025.03.011. Epub 2025 Mar 22. PMID: 40186980.
Category: Neurology
Keywords: CVA, TIA, prediction, one year (PubMed Search)
Posted: 5/21/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
How likely is your TIA pt to go on to have a stroke? This study in JAMA gives us some answers. While EM providers aren’t as interested in 5 and 10 year prediction, it provides more evidence TIAs need to be evaluated and are risk factors for future events.
“In this systematic review and meta-analysis of 171?068 patients with TIA or minor stroke from 38 studies, the risk of subsequent stroke was 5.9% within 1 year, 12.8% within 5 years, and 19.8% within 10 years.”
Category: Neurology
Keywords: Cerebral Venous Sinus Thrombosis, CVST, Low-Molecular-Weight Heparin, Unfractionated Heparin (PubMed Search)
Posted: 3/27/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
Anticoagulation is the mainstay of treatment of cerebral venous sinus thrombosis, irrespective of whether associated venous hemorrhage is present. Anticoagulant selection is variable, with physicians opting for unfractionated heparin (UFH) about 72% of the time in one international study. However, recent evidence favors the use of low-molecular-weight heparin (LMWH), with meta-analytic data showing trends towards lower mortality rates and improved functional outcomes in LMWH cohorts. UFH is often viewed more favorably due to the ability to rapidly discontinue the infusion in the event of major bleeding; however, risk of major bleeding complications were actually found to be lower in patients treated with LMWH compared to UFH. Further, LMWH has many pharmacological and practical benefits compared to UFH, including more predictable pharmacokinetics, reduced risk of heparin-induced thrombocytopenia (HIT), lack of need for frequent aPTT monitoring, ease of administration (daily subcutaneous injection), and ease of transition to outpatient therapy.
Takeaway: Consider LMWH (1.5mg/kg subcutaneously once daily) as first-line treatment for CVST in patients with acceptable renal function.
Category: Neurology
Keywords: Stroke, ICH, Hypertension (PubMed Search)
Posted: 2/20/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
Multiple trials have aimed to assess the effect of blood pressure control in the prehospital setting for patients with suspected acute stroke. The INTERACT-4 trial was a multicenter, prospective, randomized, open-label, blind endpoint trial conducted in China, in which 2404 hypertensive patients with suspected acute stroke (based on FAST score >2, symptom onset <2h, SBP >150mmHg) were randomized to receive urapidil versus usual care in the prehospital setting. The primary outcome was modified Rankin score (mRs) distribution at 90 days. Overall, no significant difference in functional outcomes at 90 days were observed in the urapidil versus usual care groups (OR 1.00, 95% CI 0.87-1.15). However, when analyzed by stroke type, improved functional outcomes and lower rates of rebleeding were seen in patients with hemorrhagic stroke (46.5% of all enrolled patients), while worsened functional outcomes and mortality were seen in patients with ischemic stroke. These observations are consistent with standard practices of intensive blood pressure reduction in patients found to have ICH, versus the “permissive hypertension” approach to patients found to have cerebrovascular occlusion. The results of this trial are not practice-changing, but do highlight the importance of prompt stroke recognition, streamlined hospital workflows for expedited diagnostics (CT), and timely initiation of antihypertensive therapy in ICH patients.
Bottom line: Prehospital blood pressure reduction was not shown to improve clinical outcomes in hypertensive patients suspected to have acute undifferentiated stroke.
Li, G., Lin, Y., Yang, J., Anderson, C. S., Chen, C., Liu, F., Billot, L., Li, Q., Chen, X., Liu, X., Ren, X., Zhang, C., Xu, P., Wu, L., Wang, F., Qiu, D., Jiang, M., Peng, Y., Li, C., Huang, Y., … INTERACT4 Investigators (2024). Intensive Ambulance-Delivered Blood-Pressure Reduction in Hyperacute Stroke. The New England Journal of Medicine, 390(20), 1862–1872. https://doi.org/10.1056/NEJMoa2314741
Category: Neurology
Keywords: Baclofen withdrawal, baclofen pump, dysautonomia (PubMed Search)
Posted: 1/16/2025 by Nicholas Contillo, MD
Click here to contact Nicholas Contillo, MD
Intrathecal baclofen pumps are increasingly used to manage spasticity in patients with conditions such as cerebral palsy, spinal cord injury, multiple sclerosis, traumatic brain injury, and other dystonias. The most common causes of baclofen pump dysfunction include pump-related issues (e.g., programming errors, battery failure), catheter problems (e.g., extra-thecal dislodgement, kinking, leaks), and medication depletion (e.g., overdue or insufficient refills). Symptoms of dysfunction can be nonspecific, ranging from mild (spasticity, dysphoria, dysesthesias) to severe (e.g., rigidity, rhabdomyolysis, seizures, fever, autonomic dysfunction, cardiomyopathy).
Once dysfunction is recognized, management involves stabilizing vital functions (ABCs, temperature management, fluids), administering multimodal antispasmodics (enteral or parenteral baclofen, benzodiazepines, dexmedetomidine, tizanidine), and performing pump interrogation, often in collaboration with neurology or PM&R specialists. Restoration of intrathecal flow is the preferred and definitive therapy; however, patients with severe withdrawal may require aggressive temporizing measures including intubation. Some authors describe intrathecal baclofen administration via lumbar puncture as a rescue measure for severe cases with limited access to definitive care. Imaging with plain radiographs, fluoroscopy, or CT may be indicated in select cases where there is concern for catheter displacement or kinking, and some patients may require surgical revision.
Takeaway: Consider baclofen withdrawal in patients on chronic baclofen therapy who present with nonspecific symptoms that may mimic conditions such as alcohol withdrawal, delirium, sympathomimetic toxicity, neuroleptic malignant syndrome, serotonin syndrome, thyrotoxicosis, rhabdomyolysis, sepsis, or status epilepticus. In cases of intrathecal pump dysfunction, the definitive treatment is restoration of baclofen flow, so involve consultants early for pump interrogation while temporizing with supportive measures.
Category: Neurology
Keywords: drug reaction, toxicity, neurotoxicity, antibiotics (PubMed Search)
Posted: 11/10/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Recognition of antibiotic associated neurotoxicity reduces unnecessary workup and serious adverse effects.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: ventriculoperitoneal shunt, neurosurgery (PubMed Search)
Posted: 10/27/2021 by David Gatz, MD
(Updated: 2/1/2026)
Click here to contact David Gatz, MD
Ventriculoperitoneal (VP) shunts are common. Unfortunately shunt complications are also common!
There are 3 major categories of shunt complications:
Shunt series are helpful, but are NOT 100% sensitive. If you have a clinical concern for a shunt complication, make sure to involve neurosurgery.
For more reading:
Category: Neurology
Keywords: burr hole, trephination, subdural hematoma, epidural hematoma, herniation (PubMed Search)
Posted: 10/13/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Your patient presents with a large traumatic subdural hematoma with midline shift and clinical evidence of herniation. Your nearest neurosurgeon is several hours away, what do you do?
Initial resuscitation should follow ATLS. Treatment of intracranial hypertension and herniation includes elevating the head of bed, administering osmotic therapies, optimizing analgesia/sedation, and hyperventilation. If all measures have been exhausted and there is a delay to definitive neurosurgical intervention, an emergency department burr hole may be considered.
Indications:
Contraindications:
Equipment:
Transtemporal Approach:
Additional Points:
Follow us on Twitter @christinap0well @EM_NCC
Category: Neurology
Keywords: Sport concussion, brain injury (PubMed Search)
Posted: 8/28/2021 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Athletes with a history of concussion had an average cerebral blood flow of 40 mL per minute, per 100 grams of brain tissue.
Athletes without a history of concussion had an average cerebral blood flow of 53 mL per minute, per 100g of brain tissue.
In the weeks following concussion, those athletes with a prior history of concussion had microstructural changes in the corpus callosum.
Effects were seen in the absence of differences in SCAT domains or time to return to sport.
Acute and Chronic Effects of Multiple Concussions on Midline Brain Structures. Churchill et al. Neurology Aug 2021.
Category: Neurology
Keywords: stroke, large vessel occlusion, basilar artery, posterior circulation, thrombectomy (PubMed Search)
Posted: 6/9/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: There is no significant difference between endovascular thrombectomy and medical management for basilar artery occlusion strokes within 6 hours of symptom onset.
Category: Neurology
Keywords: Lumbar puncture, LP, post-dural, headache, intracranial hypotension (PubMed Search)
Posted: 5/12/2021 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The use of atraumatic needles is most effective in reducing the risk of post-LP headaches. These needles are easy to use and have similar rate of success as cutting needles.
Cognat E, Koehl B, Lilamand M, et al. Preventing post-lumbar puncture headache. Ann Emerg Med. 2021 May 6;S0196-0644(21)00151-7. Online ahead of print.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: functional neurological disorder, FND, stroke mimic, non-epileptic seizure (PubMed Search)
Posted: 4/28/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Functional neurological disorders (FND) are commonly encountered in the ED. A thorough neurological exam may reveal positive signs suggestive of FND. Early diagnosis and referral to specialists may improve outcomes.
Finkelstein SA, Cortel-LeBlanc MA, Cortel-LeBlanc A, Stone J. Functional neurological disorder in the emergency department. Acad Emerg Med. 2021 Apr 18 [Online ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: acute ischemic stroke, alteplase, tPA, thrombolysis, error (PubMed Search)
Posted: 4/15/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Alteplase administration in acute ischemic stroke is associated with errors, most commonly with over-dosage of the medication.
Dancsecs KA, Nestor M, Bailey A, Hess E, Metts E, Cook AM. Identifying errors and safety considerations in patients undergoing thrombolysis for acute ischemic stroke. Am J Emerg Med. 2021;47:90-94.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Idiopathic intracranial hypertension, IIH, pseudotumor cerebri, obesity, healthcare utilization (PubMed Search)
Posted: 3/10/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence and prevalence of IIH is increasing, likely related to rising rate of obesity. This has also been associated with more healthcare utilization compared to the general population.
Category: Neurology
Keywords: Bell's palsy, facial palsy, Lyme disease, Borrelia burgdorferi (PubMed Search)
Posted: 2/24/2021 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: In a Lyme-endemic area, the incidence of positive Lyme tests and Bell’s palsy are highest in the Lyme months. This seasonal variation may help guide the management of patients with Bell’s palsy.
Pacheco A, Rutler O, Valenzuela I, Feldman D, Eskin B, Allegra JR. Positive tests for Lyme disease and emergency department visits for Bell’s Palsy patients. J Emerg Med. 2020;59(6):820-827.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: seizure, status epilepticus, nonconvulsive, electrographic, EEG (PubMed Search)
Posted: 1/27/2021 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Persistent or recurrent seizures are not uncommon in the first 24 hours after status epilepticus even in patients with resolved clinical seizure activity. Early use of EEG can help identify patients who need further escalation of treatment.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: stroke, thrombolysis, tissue plasminogen activator, tPA, monitoring (PubMed Search)
Posted: 1/13/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
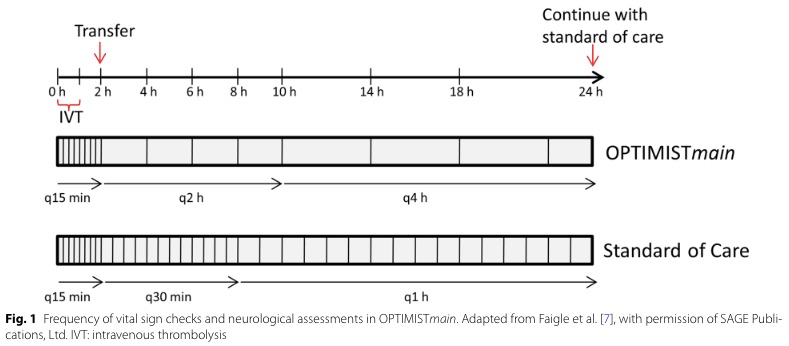
Bottom Line: Patients with NIHSS <10 may be safe for low-intensity post-tPA monitoring if they do not require critical care after an initial period of q15 min standard monitoring for the first 2 hours.
Follow me on Twitter @EM_NCC
