Category: Infectious Disease
Keywords: sepsis, intrabdominal, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/30/2025)
Click here to contact Robert Flint, MD
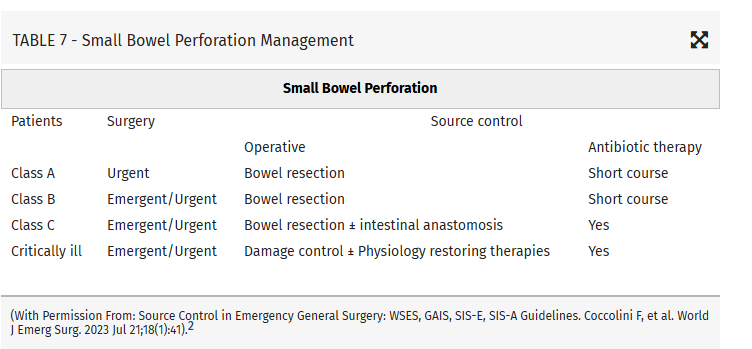
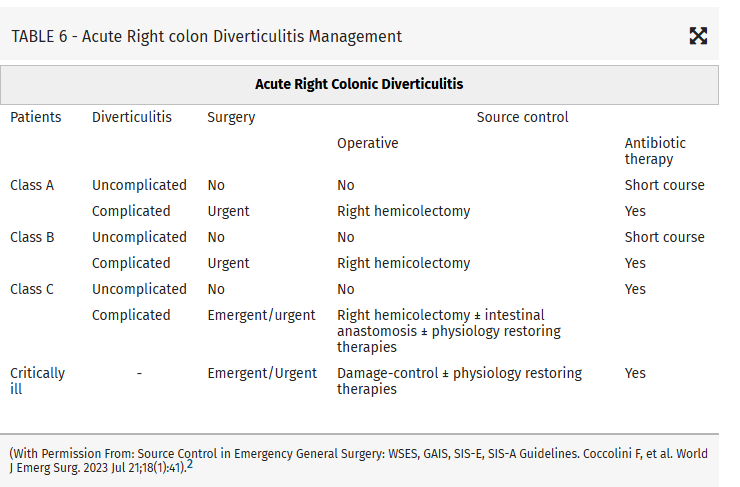
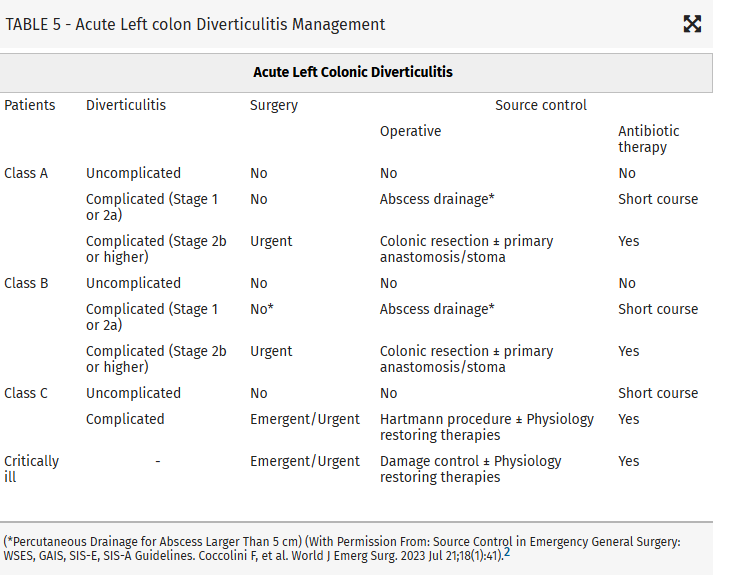
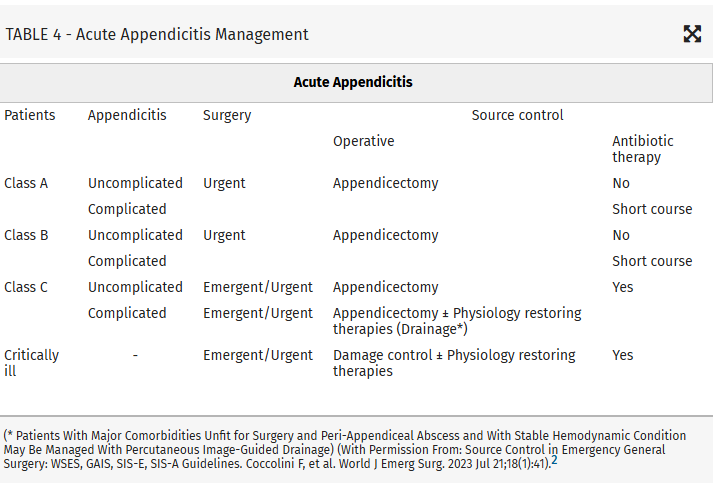
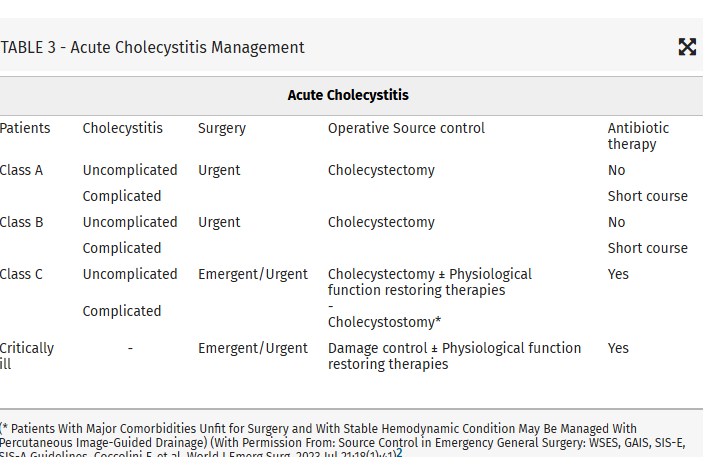
Intraabdominal infections leading to sepsis can come from cholecystitis, small bowel perforation, gastric perforation, left sided colonic diverticulitis, right sided diverticulitis and appendicitis. When to initiate source control and antibiotics is controversial. These authors propose breaking patient populations into three groups:
From this they propose algorithms to treat these intraabdominal infections such as (note the different approach to right and left diverticulitis):
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Infectious Disease
Keywords: sepsis, intrabdominal source, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/29/2025)
Click here to contact Robert Flint, MD
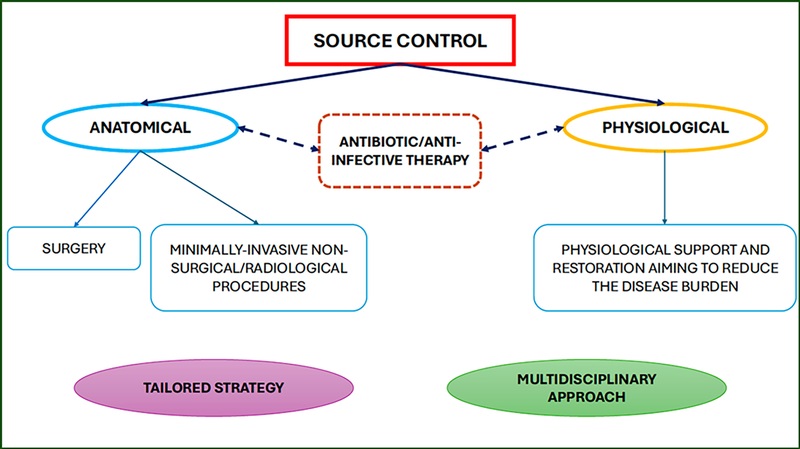
This article looks at source control as it relates to intrabdominal sources for sepsis. Key take aways are:
Those at high risk of morbidity and mortality from intraabdominal infection associated sepsis include:
Mild–moderate immune deficiency: Elderly (according to the age and general status of the patient), Malnourished, Diabetic, Burns, Trauma, Uremic, Active malignancy, not on chemotherapy, HIV with CD4+ count >200/mm3, Splenectomized, Severe immune deficiencyAIDS HIV with CD4+ count <200/mm3, Transplant (solid organ, bone marrow), High-dose steroids (more than 20 mg/day prednisone), Malignancy on chemotherapy, Neutrophil count <1,000/mm3
High-risk population (medical or surgical causes)Low serum albumin concentration Older age Obesity Smoking Diabetes mellitus Ischemia secondary to vascular disease or irradiation Prolonged or delayed/late procedures
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Infectious Disease
Keywords: Dalbavancin, bacteremia, antibiotics, transitions of care (PubMed Search)
Posted: 11/17/2025 by Lena Carleton, MD
(Updated: 11/24/2025)
Click here to contact Lena Carleton, MD
Treatment of Staphylococcus aureus bacteremia has traditionally required several weeks of intravenous antibiotics. This approach carries medical risks, such as catheter-associated infection or thrombosis, as well as significant social and financial burdens for patients. Dalbavancin, a long-acting intravenous lipoglycopeptide with activity against S. aureus (including MRSA), has been proposed as a more convenient alternative. This study evaluated the efficacy and safety of dalbavancin compared with standard therapy for S. aureus bacteremia.
Two hundred adults were enrolled in this open-label, randomized clinical trial, which was conducted in the United States and Canada. After blood cultures cleared, participants were randomized to complete therapy with dalbavancin (administered on Days 1 and 8) or with standard treatment (cefazolin for MSSA and vancomycin or daptomycin for MRSA).
The primary outcome was the Desirability of Outcome Ranking (DOOR) at Day 70, incorporating five domains: clinical success, infectious complications, safety events, mortality, and health-related quality of life.
Dalbavancin was not superior to standard therapy for treating S. aureus bacteremia, and adverse events were similar between groups. A key strength of this study was the inclusion of people who inject drugs, a population at high risk for S. aureus bacteremia and often underrepresented in trials. A major limitation was that the DOOR metric did not account for important social and economic factors, such as disposition (home versus skilled nursing facility), caregiver burden, or treatment cost.
Key Takeaway: Dalbavancin may be a suitable alternative to traditional therapy for Staphylococcus aureus bacteremia, offering less frequent dosing and a shorter treatment course. Further research is needed to identify which patients benefit most and to evaluate its impact on social and economic factors such as discharge disposition, caregiver burden, and treatment costs.
Turner NA, Hamasaki T, Doernberg SB, et al. Dalbavancin for Treatment of Staphylococcus aureus Bacteremia: The DOTS Randomized Clinical Trial. JAMA. 2025;334(10):866–877. doi:10.1001/jama.2025.12543
McCreary EK, Malani PN. New Pathways to Treat Staphylococcus aureus Bacteremia: Connecting the DOTS. JAMA. 2025;334(10):861–863. doi:10.1001/jama.2025.13717
Category: Infectious Disease
Keywords: Abscess, brain, drainage, neurosurgery (PubMed Search)
Posted: 6/22/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In a Danish study of 558 patients with a brain abscess, those that had early surgical drainage did better than those treated conservatively with antibiotics only. Prompt neurosurgical consultation is warranted for these patients.
Category: Infectious Disease
Keywords: Coccidioidomycosis, climate change (PubMed Search)
Posted: 5/26/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Typically Coccidioidomycosis is seen in the Southwestern US. The authors of this study, using climate modeling predict endemic areas will spread across the US to include Idaho, the Dakotas, Nebraska and Wyoming.
Clinically, “Patients with pulmonary Coccidioides infection frequently experience fever, cough, and shortness of breath. Chest radiographic imaging may demonstrate lobar, segmental, or multifocal consolidations; cavitary lesions; and lung nodules. Given these nonspecific findings, patients with coccidioidomycosis are often treated for community-acquired pneumonia. Coccidioidomycosis should be considered in patients not improving with antibiotic treatment or in those who have exposure to or reside in endemic areas. Up to 50% of patients with pulmonary coccidioidomycosis have erythema nodosum, approximately 25% to 30% have peripheral eosinophilia, and approximately 25% have arthralgias (particularly symmetric knee and ankle arthralgia). Up to 10% of patients diagnosed with coccidioidomycosis develop disseminated disease, including skin, central nervous system, and bone and joint infection.”
Lee PS, Swain DL, Johnson R. Climate Change and Coccidioidomycosis. JAMA. 2025;333(11):997–998. doi:10.1001/jama.2024.27274
Category: Infectious Disease
Keywords: Necrotizing infection, antibiotic selection (PubMed Search)
Posted: 4/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
In the April edition of Annals of EM, there are opposing view points on the optimal antibiotic regiment for necrotizing soft tissue infection. One group proposes linezolid alone will cover all the worrisome pathogens namely group A Strep and Staph. There are less side effects including C. Diff infection with this medication. Another group suggests sticking to vancomycin plus/minus BLactam along with clindamycin. Their arguement centers around clindamycin is useful as an antitoxin more so than its antibacterial property.
Both offer reasonable evidence and neither is compelling enough to say one is superior to the other.
Optimal antibiotic Selevtion for Necrotizing soft tissue infections. Annals of Emergency Medicine. April 2025. Vol 8, No. 4 358-360
Category: Infectious Disease
Keywords: JHR, syphillis, penicillin (PubMed Search)
Posted: 3/31/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
The Jarisch-Herxheimer reaction (JHR) is a non-specific set of symptoms (fever, malaise, worsened rash, hemodynamic instability, leukocytosis) seen after treating syphillis and other spirochete induced infections. In this study 1 in 4 patients treated with 2.4 million units of benzathine penicillin G developed a short lived JHR. Those who developed the reaction were more likely HIV negative, had secondary syphillis and had successful treatment at 6 months.
Dionne JA, Zhu C, Mejia-Galvis J, et al. Jarisch-Herxheimer Reaction After Benzathine Penicillin G Treatment in Adults With Early Syphilis: Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open. 2025;8(2):e2459490. doi:10.1001/jamanetworkopen.2024.59490
Category: Infectious Disease
Keywords: Risk, soft tissue, infection (PubMed Search)
Posted: 1/30/2025 by Robert Flint, MD
(Updated: 2/2/2025)
Click here to contact Robert Flint, MD
Risk factors for necrotizing soft tissue infections include: obesity, diabetes mellitus, peripheral vascular disease, immunosuppression, injection drug use, and deep traumatic wounds.
“Any anatomical site can be involved, but the most common sites are perineal, anorectal, foot, or lower extremities.”
Category: Infectious Disease
Keywords: Soft tissue infection (PubMed Search)
Posted: 1/30/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
These infections remain difficult to diagnose early and early diagnosis is key to limiting morbidity and mortality.
“The classic clinical signs and symptoms are rarely all present especially in early disease. Crepitus or gas in the soft tissues, while specific, is only present in approximately 10% of patients. More often, the presenting symptoms are nonspecific: fever, pain, induration, and edema. Pain out of proportion to examination is a more specific finding that may assist in differentiation of NSTI from cellulitis.”
Bisgaard, Erika K. MD; Bulger, Eileen M. MD
Journal of Trauma and Acute Care Surgery 97(5):p 678-686, November 2024. | DOI: 10.1097/TA.0000000000004351
Category: Infectious Disease
Keywords: avian, influenza, infectious (PubMed Search)
Posted: 10/31/2024 by Visiting Speaker
(Updated: 2/1/2026)
Click here to contact Visiting Speaker
By Bobbi-Jo Lowie, MD
Assistant Professor
Emergency Medicine
University of Maryland School of Medicine
Since April of 2024 there have been 36 confirmed cases of avian influenza A across the United States. Avian influenza, primarily caused by influenza viruses that infect birds, can pose significant health risks to both animals and humans. The most notable strains include H5N1 and H7N9, with H5N1 being particularly alarming due to its high mortality rate among infected humans. The virus primarily spreads from birds to humans through direct contact with infected birds, their droppings, or contaminated environments. Although there have been recorded cases of human-to-human transmission, this usually occurs only in close-contact situations.
In humans, avian influenza can present with symptoms ranging from mild respiratory illness to severe pneumonia. Patients may experience fever, cough, sore throat, muscle aches, and in severe cases, gastrointestinal symptoms. Those that have more moderate or severe illness may develop shortness of breath, altered mental status, or seizures. Complications include acute respiratory failure, pulmonary hemorrhage among others, with respiratory failure being the most common cause of death in this patient population.
Diagnosing avian influenza involves a combination of clinical presentation, travel history, and exposure to birds and confirmation through PCR testing of upper respiratory tract samples like a nasopharyngeal swab.
Treatment for avian influenza focuses on antiviral medications such as oseltamivir which is most effective when administered early in the course of the illness but still administered after 48 hours of illness. Supportive care is essential for managing severe cases, especially those that progress to acute respiratory distress syndrome.
Category: Infectious Disease
Keywords: Mpox, monkeypox, outbreak, democratic republic of congo (PubMed Search)
Posted: 8/25/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Background:
What’s new?
Who is at risk?
Patients with epidemiologic characteristics and lesions or other signs and symptoms consistent with mpox. This includes anyone with travel to DRC or any of its neighboring countries (ROC, CAR, Rwanda, Burundi, Uganda, Zambia, Angola, Tanzania, and South Sudan) in the previous 21 days.
What to look for?
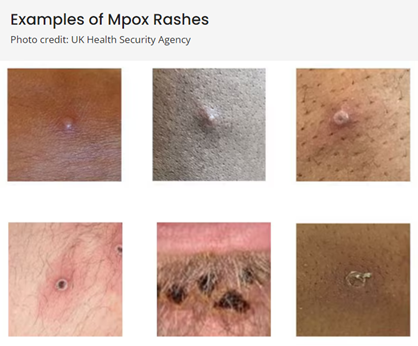
(Above photos from https://www.cdc.gov/poxvirus/mpox/clinicians/clinical-recognition.html)
What to do?
If mpox is suspected in a patient:
Duwell M. Mpox Clinician Letter. Maryland Department of Health. August 19, 2024.
Mpox Caused by Human-to-Human Transmission of Monkeypox Virus in the Democratic Republic of the Congo with Spread to Neighboring Countries. US Centers for Disease Control and Prevention. CDC Health Alert Network, August 7, 2024, 3:15 PM ET, Accessed at https://emergency.cdc.gov/han/2024/han00513.asp# on August 25, 2024.
Mpox. US Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/mpox/index.html, Accessed on August 25, 2024.
Category: Infectious Disease
Keywords: Idea, cystitis, aminoglycosides, single dose (PubMed Search)
Posted: 7/27/2024 by Robert Flint, MD
(Updated: 7/28/2024)
Click here to contact Robert Flint, MD
The Infectious Disease Society of America in 2023 recommended a single dose of an aminoglycoside for uncomplicated cystitis treatment in those with resistance or other contraindications to first line oral agents who were otherwise well enough to be discharged. This very small study (13 participants) suggest this strategy works for complicated (“male sex, urinary flow obstruction, renal failure or transplantation, urinary retention, or indwelling catheters”) cystitis patients who could otherwise be discharged home.
Academic Emergency MedicineVolume 31, Issue 7 p. 649-655
Jordan E. Jenrette PharmD, Kyle Coronato PharmD, Matthew A. Miller PharmD, Kyle C. Molina PharmD, Alexander Quinones MD, Gabrielle Jacknin PharmD
First published: 07 March 2024
Category: Infectious Disease
Keywords: HIV, Medications (PubMed Search)
Posted: 6/20/2020 by Michael Bond, MD
(Updated: 6/21/2020)
Click here to contact Michael Bond, MD
Category: Infectious Disease
Keywords: clostridium difficile, antibiotics, vancomycin (PubMed Search)
Posted: 8/4/2018 by Ashley Martinelli
(Updated: 2/1/2026)
Click here to contact Ashley Martinelli
| Clinical Definition | Treatment | |
| Initial episode, non-severe | WBC ≤ 15,000 AND SCr <1.5 |
If above agents unavailable, metronidazole PO 500mg 3x daily
|
| Initial episode, severe | WBC ≥ 15,000 OR SCr >1.5 |
|
| Initial episode, fulminant | Hypotension, shock, ileus, megacolon |
|
| First Recurrence |
|
|
McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clinical Infectious Diseases. 2018;66(7):e1-e48.
PMID: 29562266
Category: Infectious Disease
Keywords: sepsis, pseudomonas (PubMed Search)
Posted: 2/3/2018 by Ashley Martinelli
(Updated: 2/1/2026)
Click here to contact Ashley Martinelli
Debating between cefepime or piperacillin/tazobactam for your septic patient? Use this table to help you decide.
|
|
| Cefepime | Piperacillin/Tazobactam |
| Gram Negative Spectrum | Pseudomonas aeruginosa | Yes | Yes |
| Aerobic gram negative organisms | E. coli Klebsiella sp. Proteus mirabilis M catarrhalis H. influenza | E. coli Klebsiella sp. Proteus mirabilis M. catarrhalis H. influenza | |
| Anerobic gram negative organisms | No | B. fragilis
| |
| Gram Positive Spectrum | MRSA | No | No |
| Aerobic gram positive organisms | MSSA CoNS Group A Strep S. pneumoniae
| MSSA CoNS Group A Strep S. pneumoniae E. faecalis | |
| Anaerobic gram positive organisms | P. acnes Peptostreptococci | P. acnes Peptostreptococci Clostridium sp. | |
| Infection Site Concerns | CNS Penetration | Yes | No1 |
| Urine Penetration | Yes | Yes | |
| Lung Penetration | Yes | Low2 | |
| Dosing Frequency (Normal Renal Function) | Q8h | Q6h | |
1. Tazobactam CNS penetration is limited, thus limiting antipseudomonal activity in the CNS
2. Low pulmonary penetration, may not achieve therapeutic levels in patients with critical illness
Take home points:
-Piperacillin/tazobactam differs in spectrum with its ability to cover enterococcus and anaerobes. Consider for sepsis with gastrointestinal source
-Cefepime can be used for CNS infections and readily achieves therapeutic concentrations in the lungs. Metronidazole can be added to ensure anaerobic organism coverage.
-Piperacillin/tazobactam should be dosed every 6 hours in patients with normal renal function to achieve therapeutic concentration.
1. Gilbert, D. N., Chambers, H. F., Eliopoulos, G. M., Saag, M. S., & Pavia, A. T. (2016). Sanford guide to antimicrobial therapy 2016. 46th edition. Sperryville, VA, USA: Antimicrobial Therapy, Inc.
2. Nau R, Kinzig-Schippers M, Sörgel F, et al. Kinetics of piperacillin and tazobactam in ventricular cerebrospinal fluid of hydrocephalic patients.?Antimicrobial Agents and Chemotherapy. 1997;41(5):987-991.
3. Felton T, McCalman K, Malagon I, et al. Pulmonary penetration of piperacillin and tazobactam in critically ill patients. Clinical pharmacology and therapeutics. 2014;96(4):438-448. doi:10.1038/clpt.2014.131.
4. Boselli E, Breilh D, Duflo F, et al. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion critically ill patients with severe nosocomial pneumonia. Critical Care Medicine.2003;31:2102-2106.
Category: Infectious Disease
Keywords: c. difficile, antibiotic (PubMed Search)
Posted: 12/2/2017 by Ashley Martinelli
(Updated: 12/6/2017)
Click here to contact Ashley Martinelli
Community-associated Clostridium difficile infection (CA-CDI) represents 41% of all CDI cases annually. The association of specific outpatient exposures was assessed in a case control study by Guh, et al. They reviewed the CDC’s active surveillance reporting from 10 states through the Emerging Infections Program (Maryland participates).
Cases: ≥18, + C. difficile stool specimen collected as an outpatient or within 3 days of hospitalization, with no overnight stay in a health care facility in the prior 12 weeks, and no prior CDI diagnosis
Controls: matched 1:1 for age and sex within the same surveillance catchment area as the case patient on the date of the collection specimen. Exclusion criteria: prior diagnosis of CDI, diarrheal illness, overnight stay in health care facility in the prior 12 weeks
Data Collection: telephone interview, standardized questionnaire or comorbidities, medication use, outpatient health care visits, household and dietary exposures in the prior 12 weeks
Results: 452 participants (226 pairs), over 50% were ≥ 60 years of age, 70.4% female, and 29% were hospitalized within 7 days of diagnosis, no patients developed toxic megacolon or required colectomy.
Cases had more health care exposures, including the emergency department (11.2% vs 1.4% p <0.0001), urgent care (9.9% vs 1.8%, p=0.0003). In addition, cases also reported higher antibiotic exposures (62.2% vs 10.3%, p<0.0001) with statistically significant higher exposure to cephalosporins, clindamycin, fluoroquinolones, metronidazole, and beta-lactam and/or beta-lactamase inhibitor combination. The most common antibiotic indications were ear or sinus infections, URI, SSTI, dental procedure, and UTI. No differences were found in household or dietary exposures.
Take-home point: This study highlighted the risk for CA-CDI infection for patients presenting to an ED and reiterates that exposures to fluoroquinolones, cephalosporins, beta-lactam and/or beta-lactamase inhibitor combinations, and clindamycin significantly increases the risk of CA-CDI infection. Reducing unnecessary outpatient antibiotic prescribing may prevent further CA-CDI. 36% of case patients did not have any antibiotic or outpatient health care exposure; therefore, additional risk factors may exist.
Alice Y Guh, Susan Hocevar Adkins, Qunna Li, Sandra N Bulens, Monica M Farley, Zirka Smith, Stacy M Holzbauer, Tory Whitten, Erin C Phipps, Emily B Hancock, Ghinwa Dumyati, Cathleen Concannon, Marion A Kainer, Brenda Rue, Carol Lyons, Danyel M Olson, Lucy Wilson, Rebecca Perlmutter, Lisa G Winston, Erin Parker, Wendy Bamberg, Zintars G Beldavs, Valerie Ocampo, Maria Karlsson, Dale N Gerding, L Clifford McDonald; Risk Factors for Community-Associated Clostridium difficile Infection in Adults: A Case-Control Study, Open Forum Infectious Diseases, Volume 4, Issue 4, 1 October 2017, ofx171, https://doi.org/10.1093/ofid/ofx171
Category: Infectious Disease
Keywords: cellulitis (PubMed Search)
Posted: 12/15/2016 by Michael Bond, MD
(Updated: 12/17/2016)
Click here to contact Michael Bond, MD
Take home points:
Category: Infectious Disease
Keywords: Zika, arbovirus, infectious disease, mosquitos (PubMed Search)
Posted: 8/31/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Zika virus and its transmission is currently an important infectious disease topic in the United States and the Western Hemisphere. With domestic spread in the Continental United States, and the likely further spread to other parts of the southern United States, continued vigilance by healthcare providers remains important.
What are the signs and symptoms of Zika?
Most common signs and symptoms are:
Other symptoms can include
Symptoms can generally last 2 to 7 days. Most individuals will have minimal or no significant symptoms and may not seek medical care. These symptoms are similar to other arboviruses, such as dengue or chikungunya. Potential serious complications include Guillian Barre syndrome.
Of course, the main concern remains infection of pregnant women and the impact that Zika has on the developing fetus, especially for the brain.
https://www.cdc.gov/zika/symptoms/symptoms.html
Shastry S, Koenig KL, Hirshon JM. Zika Virus: Critical Information for Emergency Providers. Emerg Med Clin North Am. 2016 Aug;34(3):e25-37.
Category: Infectious Disease
Keywords: Rash, Cutaneous larva migrans, nematode, tropics (PubMed Search)
Posted: 3/16/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Cutaneous larva migrans (CLM) is an acquired dermatosis
Clinical manifestations:
Treatment:
Bottom Line:
http://emedicine.medscape.com/article/1108784-clinical
http://www.cdc.gov/parasites/zoonotichookworm/gen_info/faqs.html
https://cid.oxfordjournals.org/content/30/5/811.full
Category: Infectious Disease
Posted: 2/10/2016 by Michael Bond, MD
(Updated: 2/13/2016)
Click here to contact Michael Bond, MD
Borrella mayonii a new species
There is a new bacteria that is causing Lyme disease. Borrella burgdorferi is the typical bacteria associated with lyme disease, but now several cases of Borrelia mayonii have been isolated from patients and ticks that live in Minnesota, Wisconsin and North Dakota. What is unique about this new species is that it is associated with nausea, vomiting, diffuse macular rashes, and neuro symptoms [e.g.: confusion, visual disturbance, and somnolence) along with the typical lyme disease symptoms of arthralgias and headaches.
Current lyme tests should detect this new species and treatment is the same as Borrella burgdorferi. The take home pearl is that we may see patients with "atypical" lyme disease symptoms so this should be on our differential for patients presenting with rashes, nausea, vomiting and neurologic complaints.
