Category: Critical Care
Keywords: Sepsis, Shock, Hypotension, Fluids, Ultrasound, Vasopressors (PubMed Search)
Posted: 11/4/2025 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Another month, another study of hemodynamic targets in sepsis… The age-old questions: is a MAP > 65 a good target for everybody, or should we individualize? Should we just give a bolus of fluids to everyone and then move to pressors, or should this strategy change patient to patient?
Huet et al have a preprint that'll appear in Intensive Care Medicine looking at this question in 517 patients. I can't reprint it here due to copyright (follow link below, go to full PDF and scroll to figures at bottom if curious), but basically their algorithm was 1) check if patient is fluid responsive via either echo or swan, 2) give fluid if yes, 3) do something else (pressors) if no.
Importantly the differences were not statistically significant, but they found a strong, nearly significant, trend towards benefit on SOFA score, ICU and hospital LOS in the “personalized therapy” group (also of note, these are dubious as patient oriented outcomes). The sickest patients (by SOFA) showed the most benefit.
Bottom Line: The “personalized hemodynamic therapy” literature continues to show a modest benefit of using tools like echo (e.g. LVOT VTI) to determine if the patient is fluid responsive (or fluid tolerant) and NOT give fluid (instead using pressors) if that is not the case, but for now there's relatively limited support for hyper-personalized approaches like varying MAP goals or otherwise mixing up your strategy. Some day we'll likely find a more nuanced approach, but for now I think a reasonable strategy in critically ill septic patients is to use ultrasound to determine if the patient needs fluid, if yes give fluid and reassess, and if not move to pressors, to maintain a MAP > 65.
Category: Ultrasound
Keywords: POCUS; Pediatrics; Cardiology; left ventricular function (PubMed Search)
Posted: 11/3/2025 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
E-point septal separation (EPSS)—the distance between the anterior mitral valve leaflet and the interventricular septum during early diastole—is a well-established marker of left ventricular (LV) systolic function in adults. A threshold of 7.0 mm is commonly used to screen for severely depressed LV function. But how well does this cutoff translate to pediatric populations?
A recent retrospective study set out to explore this very question. Researchers reviewed 770 pediatric echocardiograms, including 148 with abnormal LV function and a 4:1 random sample of normal studies. Using post-exam ultrasound software, blinded operators measured EPSS across three age groups: 0-3 years, 4-12 years and 13-18 years.
Results:
Among children with LV systolic dysfunction, EPSS values increased progressively with severity:
When applying the adult 7.0 mm threshold: Sensitivity: 76.4% (95% CI: 68.5–82.8%) Specificity: 95.8% (95% CI: 93.8–97.2%)
However, the study-derived optimal threshold of 6.0 mm improved sensitivity to 81.8% (95% CI: 74.4–87.4%) while maintaining high specificity at 91.4% (95% CI: 88.9–93.5%).
Special Consideration for the Youngest Patients
In children aged 0–3 years, a lower threshold of 4.9 mm outperformed the adult cutoff: Sensitivity at 4.9 mm: 77.8% (95% CI: 51.9–92.6%) vs sensitivity at 7.0 mm: 55.6% (95% CI: 31.3–77.6%)
While these findings are promising, further research is needed to validate EPSS thresholds in emergency department (ED) settings using point-of-care ultrasound (POCUS), and to assess their feasibility in real-time clinical workflows.
Bottom Line: For older children an EPSS threshold of 7.0 mm appears to be accurate in identifying children with LV systolic dysfunction, but a lower threshold may be needed for children ages 0-3. Further studies are needed.
Chen E, Ramgopal S, Lorenz D, Jone PN, Horowitz R. Use of e-point septal separation to screen for left ventricular function in children. Am J Emerg Med. 2025 Sep 6;99:39-45. doi: 10.1016/j.ajem.2025.09.013
Category: Trauma
Keywords: Analgesia, trauma, prehospital, multimodal (PubMed Search)
Posted: 11/1/2025 by Robert Flint, MD
(Updated: 11/2/2025)
Click here to contact Robert Flint, MD
In a German study comparing one EMS jurisdiction which used IV paracetamol (acetaminophen) in combination with nalbuphine (Nubian, opiate agonist/antagonist) to another jurisdiction which used piritramide (synthetic opioid similar to fentanyl) for prehospital traumatic pain, the combination worked better to decrease pain on a numerical scale. There were no differences in typical safety measures.
The use of an antagonist/agonist theoretically could precipitate withdrawal in non-opiate naive patients and could influence in hospital analgesic choices. The literature on this is mixed.
This study offers further evidence of the efficacy of multi-modal pain control, the feasibility of paramedics using IV paracetamol and the possibility of using rapid onset opioid agonist/antagonist in the prehospital setting.
Lohmann, J., Deicke, M., Deslandes, M. et al. Prehospital analgesia for trauma-related pain by paramedics: a comparative retrospective observational study of paracetamol, nalbuphine plus paracetamol, and piritramide. Scand J Trauma Resusc Emerg Med 33, 152 (2025). https://doi.org/10.1186/s13049-025-01470-8
Category: Critical Care
Keywords: Cardiac arrest, norepinephrine, re-arrest, advantage, epinephrine (PubMed Search)
Posted: 11/1/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
A scoping review of literature involving norepinephrine use during cardiac arrest associated with a shockable rhythm found:
-evidence in animal and signal in human trials of improved myocardial and cerebral blood flow
-a suggestion of less re-arrest
There is not enough evidence comparing epinephrine to norepinephrine however this would be an excellent area of research with a theoretical advantage to norepinephrine.
Bouman, S.J., Baldussu, E., Franssen, G.H. et al. The effects of norepinephrine in shockable cardiac arrest, a scoping review. Scand J Trauma Resusc Emerg Med 33, 155 (2025). https://doi.org/10.1186/s13049-025-01480-6
Category: EMS
Keywords: cardiac arrest, mechanical devices, AHA (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/30/2025)
Click here to contact Robert Flint, MD
In the newly released American Heart Association guidelines on CPR and cardiovascular care, they state there is no evidence that mechanical compression devices show improvement in survival when compared to manual CPR. They do not recommend routine use of mechanical devices except when high quality CPR can not be maintained or when healthcare personnel safety is impacted such as during transport to the hospital.
Surely there will be more to follow on this topic.
Part 1: Executive Summary: 2025 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Author:
Marina Del Rios, Jason A. Bartos, Ashish R. Panchal, Dianne L. Atkins, et al.
Publication:
Circulation
Publisher:
Wolters Kluwer Health, Inc.
Date:
Oct 22, 2025
Category: Geriatrics
Keywords: cardiac arrest, older, epinephrine (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/29/2025)
Click here to contact Robert Flint, MD
These authors looked at survival to discharge pre and post-implementation of a single dose epinephrine protocol for out of hospital cardiac arrest as it relates to age ranges. They found that older patients had a survival rate of 12% in the single dose protocol compared to 6% in the multidose protocol. Younger and middle aged patients had no difference in survival pre and post-implementation. At least in older adults, epinephrine does not seem to offer much benefit when given more than one time during cardiac arrest.
Single Dose Epinephrine Protocol Is Associated With Improved Survival of Older Adults With Out-Of-Hospital Cardiac Arrest
Ethan J. Lilien, Nicklaus P. Ashburn, Tyler S. George, Anna C. Snavely, Bryan P. Beaver, Casey G. Costa, Michael A. Chado, Harris A. Cannon, James E. Winslow, R. Darrell Nelson … See all authors
First published: 25 September 2025 Academic Emergency Medicine
Category: Critical Care
Keywords: Ventilator, autoPEEP, asthma, COPD, obstructive lung disease (PubMed Search)
Posted: 10/28/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
Bottom line:
If a ventilated patient exhibits at least one of: persistent end expiratory flow, unequal inspiratory and expiratory flow-time areas, or ineffective breath triggers; autoPEEP must be evaluated by performing an end-expiratory hold.
If present, ventilator settings should be changed to maximize exhalation time.
In critically ill patients with obstructive lung disease, intubation and mechanical ventilation is often a last resort as it does not fix the underlying pathology of small airway disease. While many complications can arise, the most feared complication is autoPEEP.
What is autoPEEP?
AutoPEEP is excess air trapping in the lungs because the patient has insufficient time to fully exhale. Patients at highest risk include those with obstructive lung pathology due to their increased resistance (from bronchospasm) and sometimes increased compliance (such as in emphysema).
However, it is possible for any patient to develop autoPEEP depending on the amount of time they have to exhale. As respiratory rate increases, the expiratory time decreases proportionally if inspiratory time is kept constant. Ultimately, autoPEEP can lead to rapidly increasing intrathoracic pressures causing decreased preload leading to hemodynamic instability and potentially cardiac arrest. These elevated pressures also place the patient at significant risk of barotrauma/volutrauma.
How do I find it?
There are several signs on the ventilator waveforms for autoPEEP. Some patients may only exhibit one of the following signs of autoPEEP. They are demonstrated in the attached pictures in various ventilator modes.
Image A. Persistent end expiratory flow on the flow-time curve (middle curve) - demonstrated by the expiratory limb of the flow curve not returning to zero (remains negative)
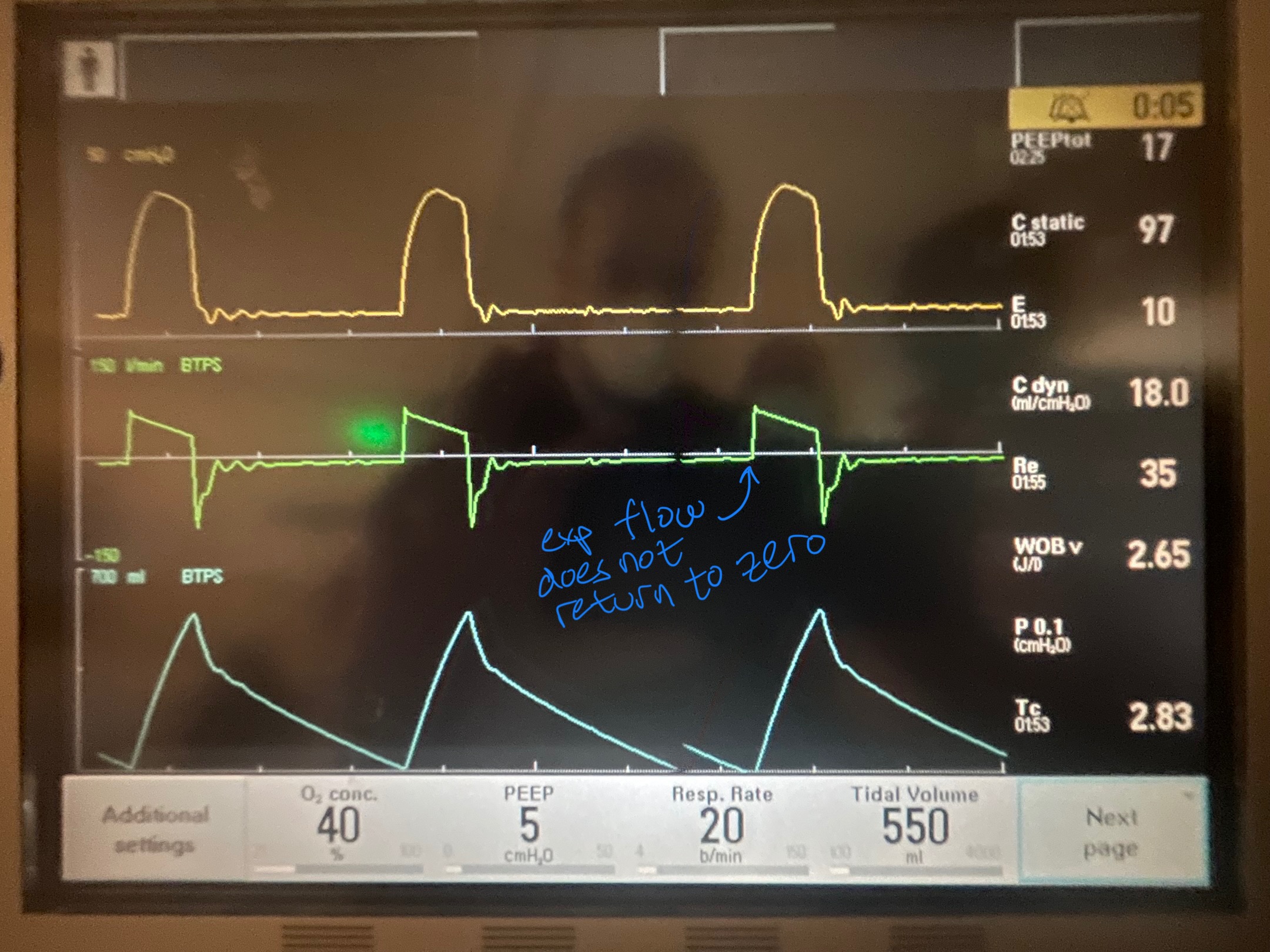
Image B. Unequal inspiratory and expiratory volumes on the flow-time curve (area of flow curve inspiratory limb does not equal area of flow curve expiratory limb)
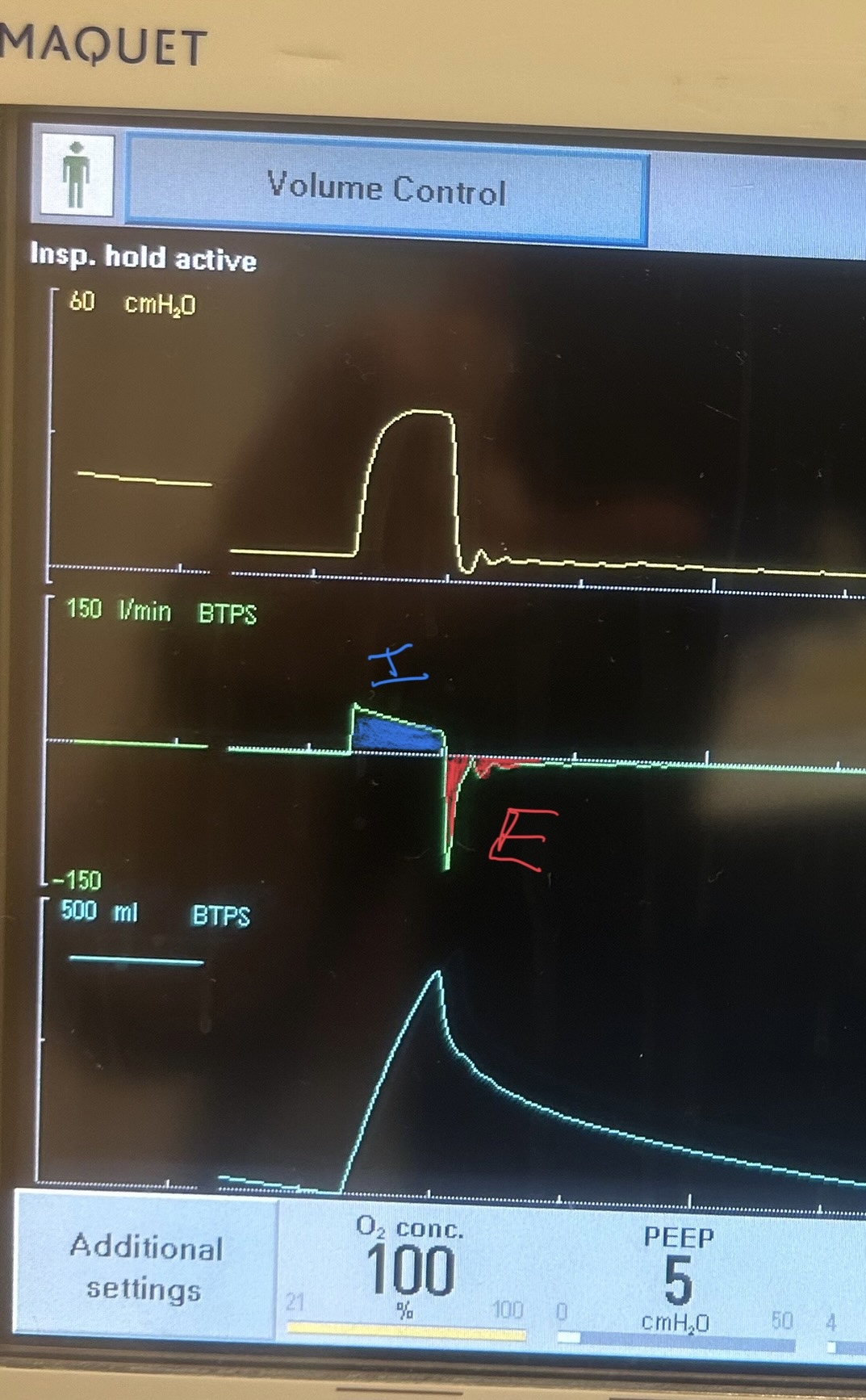
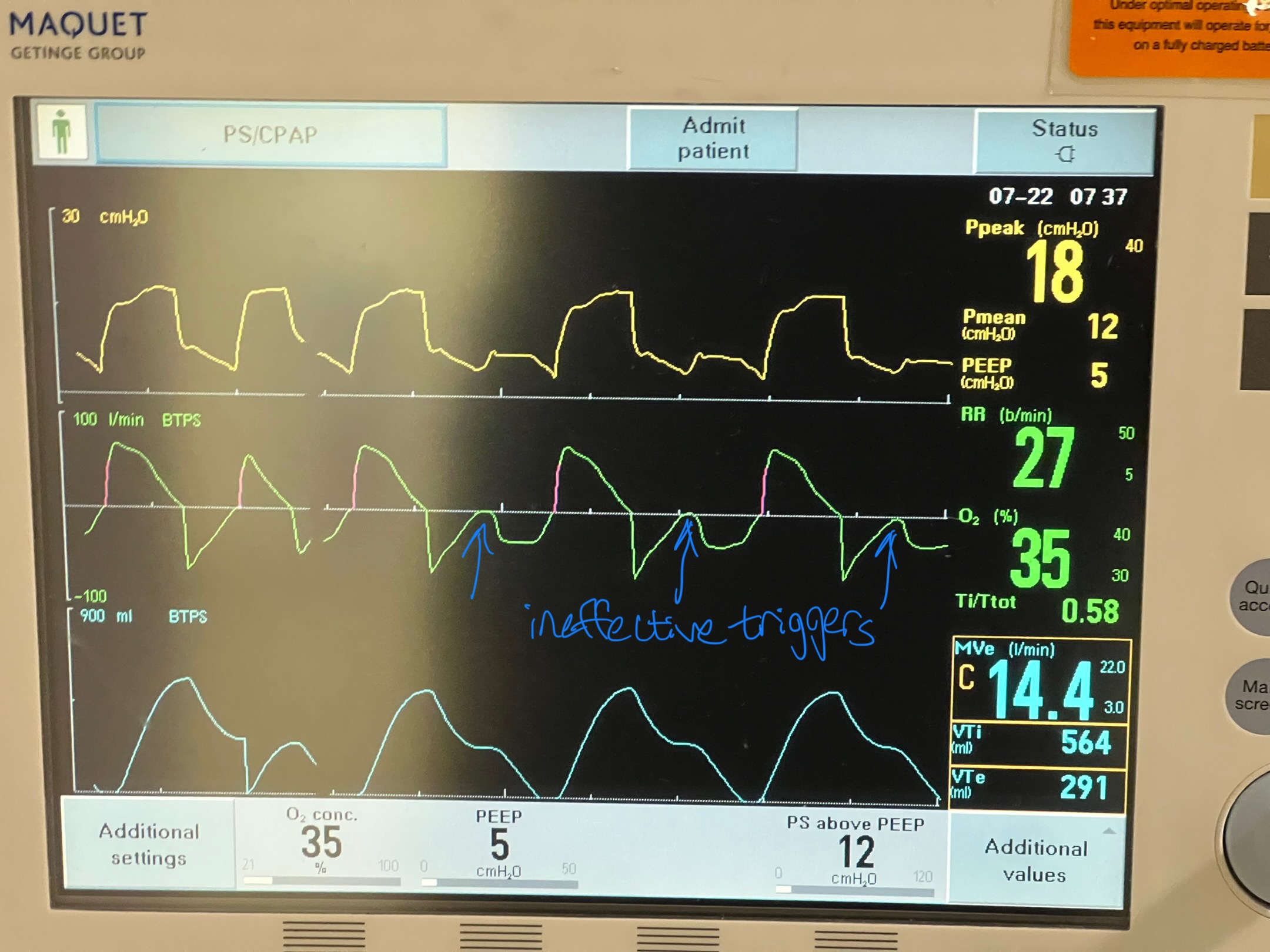
Image C. Ineffective triggering (seen on flow-time curve; patient has to perform more work to reach trigger threshold when autoPEEP is present; they are sometimes unable to trigger a breath)
If any of these are present, an end-expiratory hold maneuver should be performed.
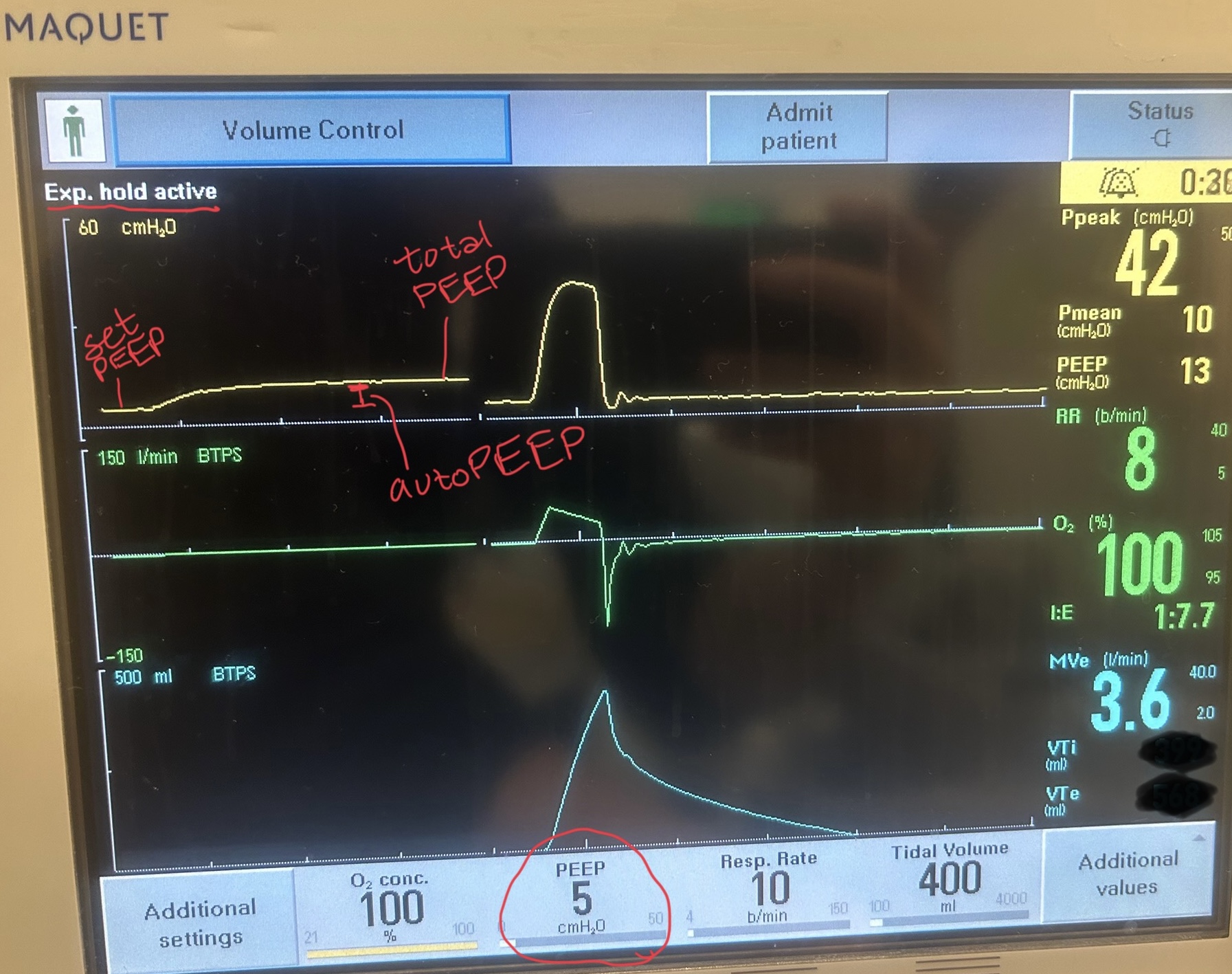
Image D - End-expiratory hold maneuver (done if patient is passive on the ventilator) - the pressure-time curve will begin at ventilator set PEEP and reach total PEEP at the end of the maneuver. The difference between total PEEP and set PEEP is autoPEEP.
If autoPEEP is present, ventilator changes to allow for more exhalation time should be made. The most effective change is by decreasing the respiratory rate though small improvements can be made by changing the inspiratory time and tidal volume. Appropriate bronchodilator therapy, sedation, and treatment of underlying pathology is also critical in these patients.
For more information on autoPEEP, check out this post by Dr. John Greenwood discussing autoPEEP on MarylandCCProject with video demonstrations!
Category: EMS
Keywords: single dose, epinephrine, cardiac arrest, survival (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/27/2025)
Click here to contact Robert Flint, MD
The authors conducted a pre- and post-implementation study after five North Carolina county EMS agencies switched to single dose epinephrine during out of hospital cardiac arrest treatment from the traditional multidose (every 3-5 minutes) protocol. They looked at 1 year before and 1 year after implementation. They found no difference in survival to discharge from the hospital in the two groups but there was less return to spontaneous circulation in the single dose group.
Ashburn, N. P., Beaver, B. P., Snavely, A. C., Nazir, N., Winslow, J. T., Nelson, R. D., … Stopyra, J. P. (2022). One and Done Epinephrine in Out-of-Hospital Cardiac Arrest? Outcomes in a Multiagency United States Study. Prehospital Emergency Care, 27(6), 751–757. https://doi.org/10.1080/10903127.2022.2120135
Category: Trauma
Keywords: brain injury, evidence, eucapnia, normotensive, care (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/26/2025)
Click here to contact Robert Flint, MD
Another paper emphasizing care for brain injured patients should include:
-pre-intubation preoxygenation to avoid hypoxia
-pre-intubation avoid extremes in blood pressure (hypotension kills)
-use hemodynamically neutral induction agents such as ketamine or etomidate
-post intubation target eucapnia on the ventilator. (do not aim for low CO2)
-post intubation maintain adequate sedation to avoid increased intercranial pressure
Hoyne J, Edlow J. Airway Management in Patients With Acute Brain Injury or Ischemia. J Emerg Med. 2025 Jul;74:125-133. doi: 10.1016/j.jemermed.2024.12.015. Epub 2025 Jan 6. PMID: 40348691.
Category: Orthopedics
Posted: 10/25/2025 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Low-Dose Radiation Therapy for Osteoarthritis
Current options for osteoarthritis include NSAIDs, physical therapy, intraarticular steroid injections, and lifestyle modifications, such as weight loss and exercise. After these options have been exhausted, there is joint replacement.
Problems with these options in older patients are that about 25% of all patients will not respond to these therapies or lose their responsiveness over time. NSAIDs also may not be great options in those with renal impairment and increased risk of GI bleeding.
Conventional radiation therapy (RT) in the treatment of malignant disorders relies on its antiproliferative effects. Alternatively, at doses of less than 1 Gray, RT has been shown to have strong anti-inflammatory effects.
RT may be an appropriate option for those with OA who have failed other conservative measures but are not ready for joint replacement…ideally before the onset of bone-on-bone changes at which point RT is less likely to be effective.
Appropriate candidates are older than 50 years. Patients do not typically experience acute side effects. There may be slight redness, milder than a sunburn, on the skin of the area radiated. Malignancy induced by RT treatment remains a small theoretical risk and is mitigated by selection of non central joints (i.e. not for spine OA).
The most commonly treated joints include hands, feet, knees, and elbows.
Pain relief can last from several months to years, with studies reporting that 30%-60% of patients maintain significant pain reduction 1-2 years after treatment. In one study, patients reported 85% decreased use of analgesic medications.
Typical treatment regimens involve 6 sessions of 0.5 Gy each conducted 2-3 times per week.
RT may be an effective modality for patients who have failed conventional treatment and are either not ready for surgery or are poor surgical candidates.
The Use of Low-Dose Radiation Therapy in Osteoarthritis: A Review
Dove, Austin P.H. et al. International Journal of Radiation Oncology, Biology, Physics, Volume 114, Issue 2, 203 - 220
Category: Administration
Keywords: complaint, service recovery, administration (PubMed Search)
Posted: 10/20/2025 by Steve Schenkel, MPP, MD
(Updated: 10/22/2025)
Click here to contact Steve Schenkel, MPP, MD
Do you ever have to manage a complaint? Perhaps a patient complaint?
It can be tough to hear a complaint. Emotions can run high. And then the ability to listen and respond can fade.
It helps to have a shorthand to guide the response.
Customer service literature provides one that often works well: LAST, for Listen, Apologize, Solve, and Thank.
This article gets at the basic idea (while adding one or two additional items): Steinman, HK. A Method for Working with Displeased Patients—Blast. J Clin Aesthet Dermatol. 2013 Mar;6(3):25–28. https://pmc.ncbi.nlm.nih.gov/articles/PMC3613270/.
Category: Critical Care
Posted: 10/21/2025 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Check for Elevated ICP in the Post-ROSC Patient
Long B, Gottlieb M. Emergency medicine updates: Managing the patient with return of spontaneous circulation. Am J Emerg Med. 2025; 26-36.
Category: Geriatrics
Keywords: RSV, geriatric, heart failure, morbidity (PubMed Search)
Posted: 10/19/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study looked at older patients admitted to the hospital with a diagnosis of one of the following: RSV infection, UTI, influenza, fracture. Those patients with RSV had longer stays, higher mortality, higher ICU length of stay and interestingly more cardiovascular complications up to one year after hospitalization. Further evidence we should be testing for RSV in our ill older patients and encouraging vaccination.
Category: Pediatrics
Keywords: caffeine, bronchiolitis, respiratory distress (PubMed Search)
Posted: 10/17/2025 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Premature infants in the NICU are often given caffeine to help to prevent apneic episodes and this has been proven safe. This study aims to determine if caffeine will help infants < 8 weeks with bronchiolitis, even if there is no concern for apnea. The current recommended treatment for bronchiolitis is supportive care.
2 French Hospitals with the same protocols and resources for bronchiolitis participated. All infants admitted to each hospital with a diagnosis of bronchiolitis were included. Infants who presented to Hospital A received caffeine and infants who presented to hospital B did not. The remainder of their care was similar. The caffeine was given as a bolus dose followed by a daily maintenance dose until there was clinical improvement. The dose was the standard dose used in premature infants with apnea as recommended by the French National Authority for Health. There were 26 patients at the study hospital that did not receive caffeine for an unknown reason. 65 patients received caffeine.
The study had several areas showing statistical significance:
In the subgroup of RSV + patients, those who did NOT receive caffeine had a higher incidence of requiring ventilatory support.
The use of high flow nasal cannula was HIGHER in the group with NO caffeine.
The use of CPAP was HIGHER in the caffeine group BUT the duration of CPAP use was shorter compared to the NO caffeine group.
The need for nutritional support was higher in the NO caffeine group.
There were a few cases of temporary tachycardia and irritability in the caffeine group which resolved several hours after the medication was given.
A larger study is needed, but in this small group, there may be an indication for caffeine outside of the NICU for infants < 8 weeks.
Casabianca M, Akouka D, Maman L, Lopes AA. Caffeine Was Associated With Shorter Continuous Positive Airway Pressure Treatment for Infants up to Eight Weeks Old Hospitalised for Bronchiolitis. Acta Paediatr. 2025 Aug 27. doi: 10.1111/apa.70279. Epub ahead of print. PMID: 40862534.
Category: Critical Care
Keywords: delirium, ICU, acetylcholinesterase inhibitor (PubMed Search)
Posted: 10/14/2025 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
Delirium is common among critically ill patients. Some of the common Acetylcholinesterase inhibitors (AChEI), rivastigmine, donepezil, have been used to prevent delirium in ICU patients. However, their efficacy was just recently re-examined in a meta-analysis of only Randomized Control Trials.
Ten studies and 731 patients were included- 365 in the treatment (AChEI) group and 366 in the control group.
AChEI was associated with lower occurrence of delirium (RR 0.68, 95% CI 0.47-0.98, p=0.039. However, there was no significant difference in the delirium duration (mean difference -0.16 day, 95% CI -0.95 to 0.62 day, p=0.23). There was no difference in delirium severity nor length of hospital stay.
Among the medication, interestingly, rivastigmine 4.5 mg/day significantly reduced delirium occurrence (RR = 0.61 [0.39– 0.97]) and severity (SMD = –0.33 [–0.58 to –0.08]), as well as length of hospital stay (MD = –1.29 [–1.87 to –0.72]).
Discussion:
This meta-analysis was well-conducted.
The cholinergic dysregulation—especially elevated acetylcholinesterase activity—can lead to the imbalance between attention and cognition, contributing to delirium in ICU patients. Thus, the use of AChEI and reduction of occurrence of delirium proves that acetylcholine deficiency may be associated with delirium among ICU patients.
Subgroup analysis showed that prophylactic use of AChEI was associated with significant reduction of delirium duration. Thus, further studies are needed to define which populations will benefit from AChEI.
Conclusion:
AChEIs are effective in reducing occurrence of delirium, but they did not affect delirium duration, severity or hospital LOS.
Pipek LZ, Pascual GS, Nascimento RFV, Silva GD, Castro LH. Acetylcholinesterase Inhibitors for Delirium Prevention: A Systematic Review and Meta-Analysis. Crit Care Med. 2025 Oct 1;53(10):e2054-e2061. doi: 10.1097/CCM.0000000000006786. Epub 2025 Aug 5. PMID: 40758382.
Category: Obstetrics & Gynecology
Posted: 10/9/2025 by Jennifer Wang, MD
(Updated: 2/2/2026)
Click here to contact Jennifer Wang, MD
At this point, we've likely all encountered a patient who is on aspirin as a preventative for a history of pre-eclampsia or high risk pregnancy, but what about for low risk patients who have not yet had any children?
This meta-analysis came out in August of this year looking at RCTs that examined giving low dose aspirin to low-risk (no pre-eclampsia, gestational DM/HTN, autoimmune or renal disease), nulliparous individuals during pregnancy and found that while not all doses of aspirin at all ages were helpful, a planned subgroup analysis showed that giving 100mg of aspirin daily starting before 16 weeks cut the odds of preterm birth before 37 weeks in about half (RR 0.45).
That's not to say that we should all be starting aspirin for our patients in the emergency department just yet - but this might be why you're seeing aspirin pop up on more of our pregnant patients' medication list (or why your OB might be recommending it to you or your family/friends).
Wodoslawsky S, Khanuja K, Saccone G, Hoffman MK, Berghella V. Low-dose aspirin use in low-risk nulliparous pregnancies: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol MFM. 2025;7(2):101595. doi:10.1016/j.ajogmf.2024.101595
Category: Geriatrics
Keywords: fall, score, geriatric, prediction (PubMed Search)
Posted: 10/11/2025 by Robert Flint, MD
(Updated: 10/12/2025)
Click here to contact Robert Flint, MD
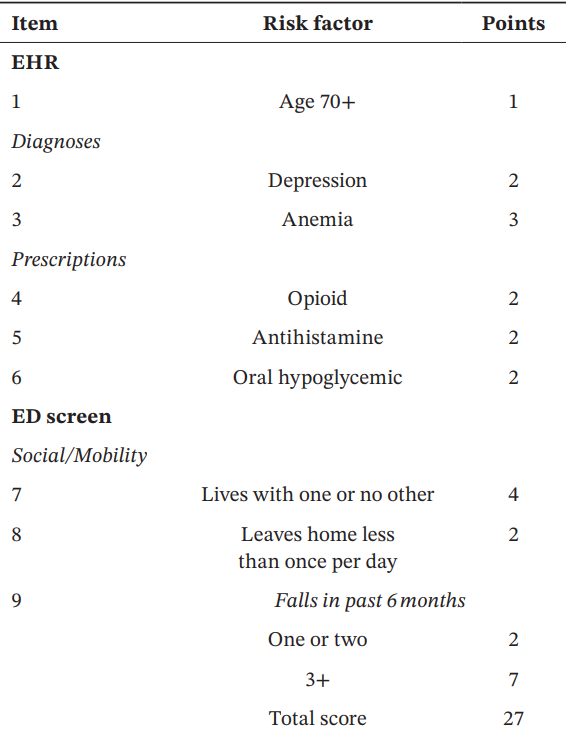
These authors used information available from both the medical record as well as from a survey instrument given in the emergency department to created this fall risk score. A score over 6 had a 63% sensitivity and 75% specificity of predicting future falls.

Acaemic Emergency Medicine 2025 0:1-12
Category: Orthopedics
Posted: 10/11/2025 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Use of Muscle Relaxants in the Elderly
A recent pearl discussed the risks of skeletal muscle relaxants (SMR) in the elderly population.
Risks included sedation, confusion, disorientation, orthostatic hypotension and increased risk for falls and fractures.
The Beers Criteria is a list of medications that older adults should generally avoid due to potential adverse effects.
Two commonly used muscle relaxants, Baclofen and Tizanidine (Zanaflex) are not included in the Beers criterion.
A study published last month investigated the safety profile of these medicines as compared to cyclobenzaprine (Flexeril).
Retrospective cohort study of Kaiser Permanente Southern California patients aged 65 to 99 years between 2008 and 2018.
From a population of approximately 88,000 participants (mean age 71.4 years; 59.8% women), approximately 118,000 study medication episodes were identified: 54.8% participants were dispensed baclofen, 6.3% tizanidine, and 38.9% cyclobenzaprine
Outcomes included injury-related hospitalizations, emergency department visits, and urgent care visits documented in EMR and identified through diagnostic codes for fractures, falls leading to fractures, brain injuries, and dislocation injuries
Compared with cyclobenzaprine, Baclofen demonstrated a 69% greater risk (adjusted Hazard Ratio 1.69, [95% CI 1.51-1.88]) and tizanidine carried a 34% greater risk (adjusted Hazard Ratio 1.34, [95% CI 1.11-1.62]) for composite injury outcomes.
Conclusion: Older adult patients prescribed baclofen or tizanidine have an increased risk of injury when compared with Flexeril (currently included on the Beers Criteria)
George MM, et al. Safety of Baclofen and Tizanidine in Older Adults: A Retrospective Cohort Study in a Large Integrated Health Care System. J Am Geriatr Soc. 2025 Sep 13
Category: Pediatrics
Keywords: pediatrics, sinusitis, infectious diseases (PubMed Search)
Posted: 10/10/2025 by Kathleen Stephanos, MD
(Updated: 2/2/2026)
Click here to contact Kathleen Stephanos, MD
As we enter cold and flu season, sinus issues become commonplace in the ED. What do we need to know about pediatric sinusitis?
First, it is important to know when pneumatization of the sinuses occur (so we don't look for symptoms where they can't be present). Completion of their development does not occur until around age 21 years.
Sinusitis should be a clinical diagnosis and does not require imaging unless there is concern for abscess development, cellulitis or other complications, or in cases where symptoms are not improving despite treatment.
In most otherwise healthy children, acute sinusitis is typically viral in nature, regardless of the color of nasal discharge, and can be managed with symptomatic care, including saline sprays, humidifiers, warm compresses and monitoring.
There are strict criteria for otherwise healthy children regarding when to initiate antibiotics including:
The antibiotic of choice is high-dose amoxicillin with or without clavulanic acid (cefpodoxime or cefdinir can be considered in penicillin allergic patients)
Antibiotic stewardship is critical in these patients, as unnecessary antibiotics can result in resistance or undesired side effects. There should be a clear conversation about return precautions with parents including education about the importance of symptomatic management over antibiotics in the first 10 days.
Ramadan HH, Chaiban R, Makary C. Pediatric Rhinosinusitis. Pediatr Clin North Am. 2022 Apr;69(2):275-286. doi: 10.1016/j.pcl.2022.01.002. PMID: 35337539.
Leung AK, Hon KL, Chu WC. Acute bacterial sinusitis in children: an updated review. Drugs Context. 2020 Nov 23;9:2020-9-3. doi: 10.7573/dic.2020-9-3. PMID: 33281908; PMCID: PMC7685231.
Category: Pharmacology & Therapeutics
Keywords: rapid sequence intubation, rocuronium, paralytic, awareness (PubMed Search)
Posted: 10/9/2025 by Alicia Pycraft
Click here to contact Alicia Pycraft
It is estimated that between 2.6% and 3.4% of patients undergoing rapid sequence intubation (RSI) experience awareness with paralysis, with the highest risk observed in patients receiving rocuronium. Several studies have now demonstrated prolonged time to sedation following RSI with long-acting paralytics, including a 2024 single-centered retrospective chart review by Dukes et al., which found that fewer than half of patients in the ICU receiving rocuronium for RSI were administered sedation within 15 minutes of intubation. The following study by Cappuccilli et al. sought to compare differences in sedation practices between the ED and ICUs at the same institution, hypothesizing that patients undergoing RSI in the ED would experience similar delays in sedation to those in the ICU.
