Category: EMS
Keywords: GCS, pediatric trauma, motor (PubMed Search)
Posted: 6/18/2025 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
GCS was first introduced in 1974 and now includes a preverbal version for patients < 2 years.
This study looked for non inferiority between motor Glascow Coma Scale (mGCS) and the total GCS in pediatric patients. The study also examined if a mGCS<6 was non inferior to a GCS < 14 in children. 582 patients < 18 years were reviewed in this retrospective review.
The mGCS was noninferior to total GCS as a triage tool in pediatric trauma. It also validated the use of mGCS <6 in place of GCS <14 in the field with identification of children at risk of death or requiring ICU care.
Yap SE, Wong HC, Chong SL, Ganapathy S, Ong GY. Validation of motor component of Glasgow coma scale in lieu of total Glasgow coma scale as a pediatric trauma field triage tool. Am J Emerg Med. 2024;81:105-110. doi:10.1016/j.ajem.2024.04.031
Category: Critical Care
Keywords: ARDS (PubMed Search)
Posted: 6/16/2025 by Jordan Parker, MD
(Updated: 6/17/2025)
Click here to contact Jordan Parker, MD
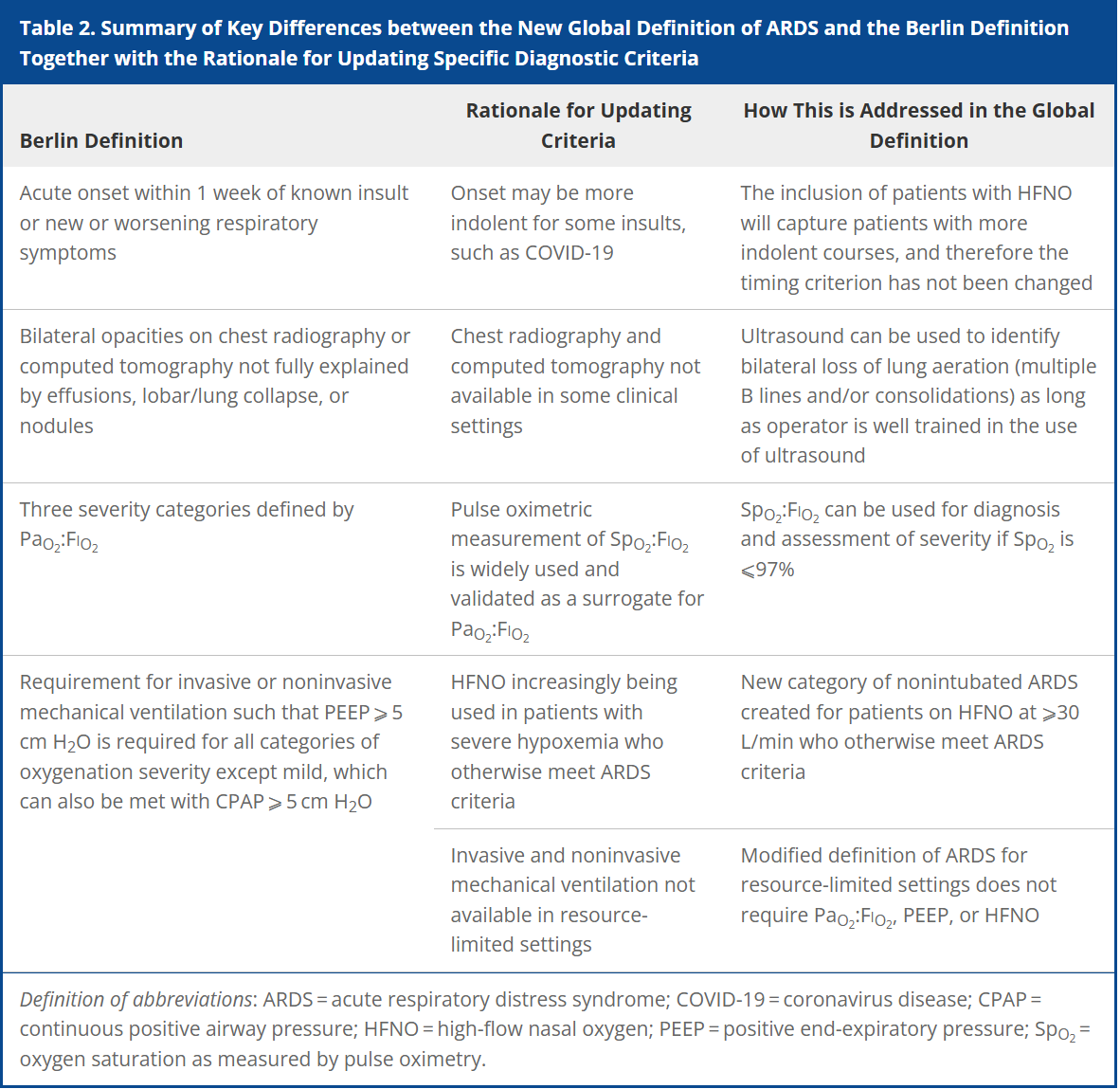
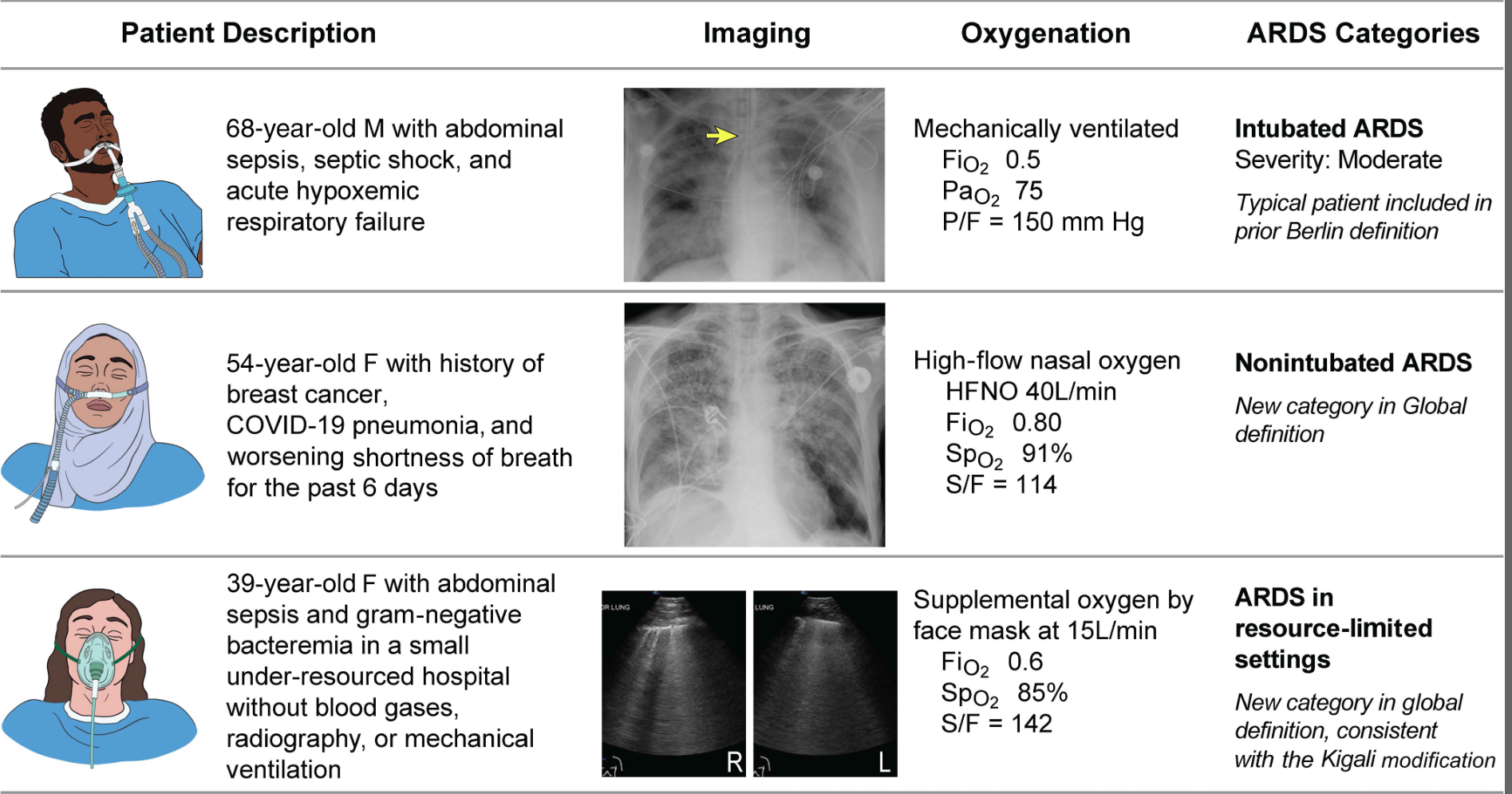
Acute respiratory distress syndrome (ARDS) is an acute, inflammatory lung injury that effects the lung diffusely and can be triggered by various insults. Aside from the Kigali modification, the most recent updated definition of ARDS was the Berlin definition in 2012. There have been many advances and changes in the understanding and clinical practice for managing patients with ARDS since then. In 2024, Matthay, et al. proposed the new global definition to build upon the Berlin criteria [1]. They addressed several important issues with the Berlin definition to improve the diagnostic criteria and improve ability for diagnosis in resource-limited settings.
ARDS Berlin Definition
Important updates for the Global definition of ARDS
Diagnostic Criteria for the New Global Definition of ARDS from Matthay et al.
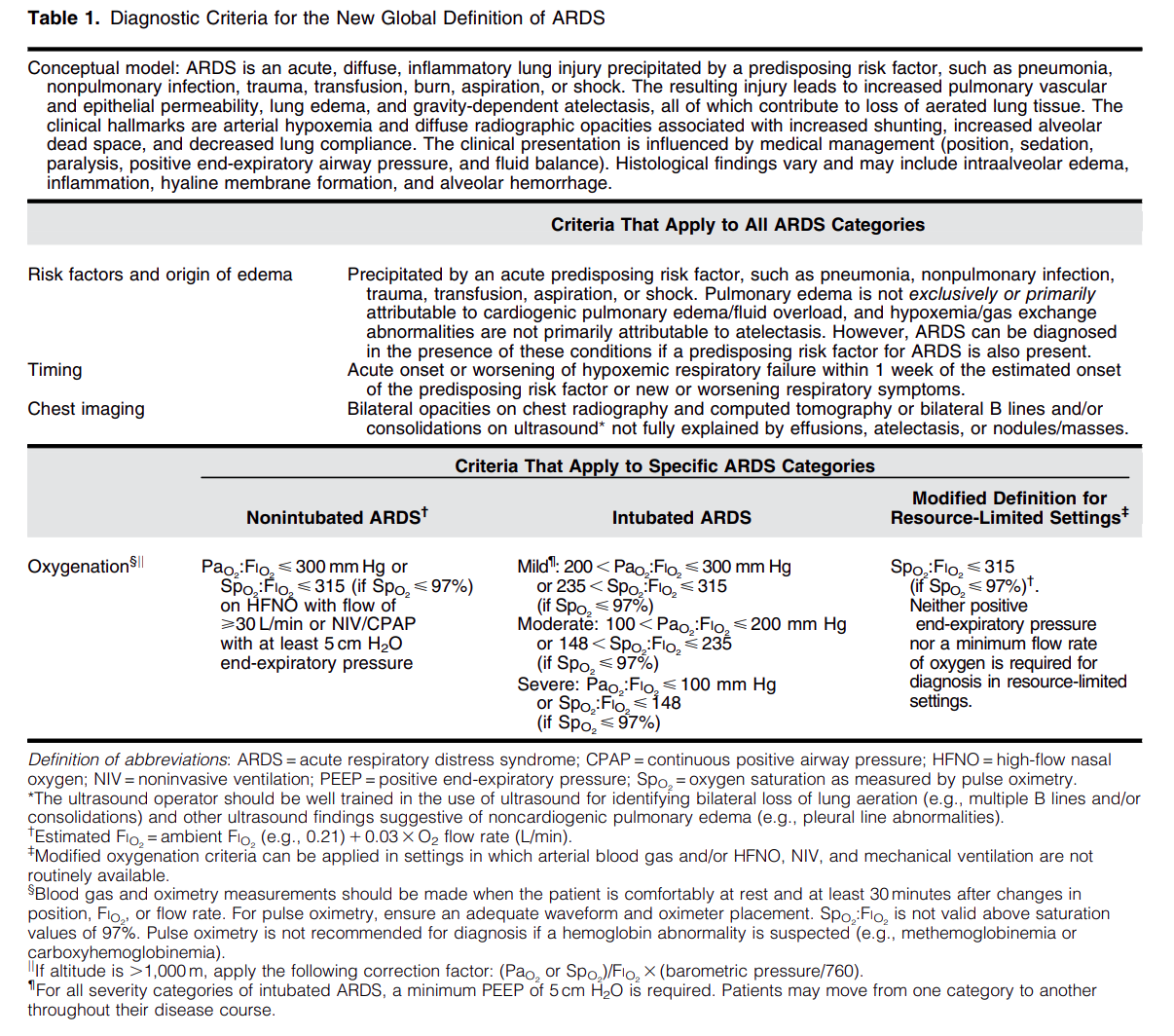
The Global Definition of ARDS expands upon the Berlin definition. It was shown that this new definition improves diagnosis in resource-limited settings, allows for earlier detection, and better classification [2]. A retrospective study evaluating this new global definition found that there was a significant number of patients identified using this new definition who would have been missed using the Berlin definition [3]. These patients may benefit from ARDS directed therapies and further prospective studies will be needed to assess how this new definition effects clinical management of these patients using the new definition.
Helpful table/figure from the paper.
Category: Ultrasound
Keywords: POCUS, Hip Effusion, MSK (PubMed Search)
Posted: 6/16/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
A hip effusion can cause pain with leg movement in both pediatric and adult patients.
A recent multicenter, prospective study assessed the diagnostic accuracy of POCUS performed by pediatric emergency physicians in detecting hip effusion.
They found that POCUS had a sensitivity of 89.3% (95% CI 80.6 to 95.0%) and specificity of 99.2% (95% CI 97.0 to 99.9%).
To scan the hip:
-Position the patient supine with the patient’s hip externally rotated.
-Place the probe transversely across the patient’s leg with the marker towards the patient’s right and scan proximally.
-Upon reaching the proximal femur, rotate the probe marker so it points towards the patient’s umbilicus.
-Look for an anechoic stripe at the femoral neck, preceding the femoral head.
An anechoic stripe measuring at least 5 mm in the anterior synovial space or an asymmetry exceeding 2 mm compared to the opposite, asymptomatic hip is diagnostic for hip effusion in BOTH pediatric and adult populations.
Jones RM, Malia L, Snelling PJ, Riera A, Mak W, Moote D, Brimacombe M, Chicaiza H. Diagnostic Accuracy of Point-of-Care Ultrasound for Hip Effusion: A Multicenter Diagnostic Study. Ann Emerg Med. 2025 Jun 7:S0196-0644(25)00279-3. doi: 10.1016/j.annemergmed.2025.04.033. Epub ahead of print. PMID: 40481828.
Category: Trauma
Keywords: Intubation, trauma, mortality, operating room, Ed (PubMed Search)
Posted: 6/15/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
In this Israeli study comparing mortality for trauma patients intubated in the emergency department vs the operating room, in hospital mortality was higher for the ED group before controlling for injury severity score and shock. After controlling for injury severity and shock, there was no difference in In hospital mortality. Coupled with previous research, if intubation can wait until after resuscitation and in the OR, that is ideal. And sometimes it just has to happen in the ED and we should be prepared for rapid resuscitation.
Talmy T, Radomislensky I, Brzezinski Sinai I, Shaylor R, Katorza E, Gendler S; Israel Trauma Group Collaborators. Intubation Setting and Mortality in Trauma Patients Undergoing Hemorrhage Control Surgery: A Propensity Score-Matched Analysis. Anesth Analg. 2025 May 16. doi: 10.1213/ANE.0000000000007542. Epub ahead of print. PMID: 40378073.
Category: Orthopedics
Posted: 6/14/2025 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
NSAIDs are first line analgesic medications for many pain related ED presentations
All NSAIDs are not created equal in their side effect profile
Ibuprofen and ketorolac are both commonly used NSAIDs in the ED
A 2010 review looked at relative risk estimates of individual NSAIDs and associated upper GI bleeding/perforation.
Definitions: Most of included studies included patients with NSAID use within prior week and daignosed upper GI bleed admitted to the hospital.
Daily use predicted increased risk.
In comparison between these two common medications Ibuprofen and Ketorolac: RR as follows
Ibuprofen (2.69 [95% CI 2.17-3.33]) vs ketorolac (14.54 [95% CI 5.87-36.04])
Ketorolac has approximately double the half life of ibuprofen
Other commonly used ED medications were also included:
RRs:
Naproxen 5.63 (95% CI 3.83-8.28)
Indomethacin 5.40 (95% CI 4.16-7.00)
Meloxicam 4.15 (95% CI 2.59-6.64)
Diclofenac 3.98 (95% CI 3.36-4.72)
Conclusion: The risk of upper GI bleeding varies between individual NSAIDs at the doses commonly used in the general population. When possible, consider the relative risk of a particular NSAID when making a selection.
Massó González EL, Patrignani P, Tacconelli S, García Rodríguez LA. Variability among nonsteroidal antiinflammatory drugs in risk of upper gastrointestinal bleeding. Arthritis Rheum. 2010 Jun;62(6):1592-601.
Category: Pediatrics
Keywords: environmental, climate change, heat, pediatrics (PubMed Search)
Posted: 6/13/2025 by Kathleen Stephanos, MD
(Updated: 2/2/2026)
Click here to contact Kathleen Stephanos, MD
As the weather warms up, remember that pediatric patients have some physiologic factors that increase their risk of heat related complications. Approximately 37 infants die in cars annually, with risk of vehicular related heat illness starting with outdoor temperatures as low 72°F (32°C). Approximately 9,000 high school athletes require treatment for heat related illness annually with approximately 2 deaths per year.
Physiology:
Infants and young children have physiologically limited thermoregulation. They also may lack developmental abilities to impact their environment (they cannot ask for water, remove clothing or a seat belt, or move themselves to a cooler environment).
Older children take longer to acclimate to environments than their adult counterparts- requiring 10-14 days to adjust to work outs in higher temperatures (a gradual approach of increasing gear over time has been recommended for outdoor sports requiring padding or heavy equipment)
Management:
Heat exhaustion/stroke- focus on cooling the patient with temperatures being monitored with a core measurement. In teens and older children this can be done in a similar manner to adults- with removal of clothes, emersion therapy for heat stroke. In infants and young children, some experts favor evaporative management over emersion due to reflex bradycardia as well as patient compliance.
There are no recommended medications for use during heat stroke. Benzodiazepines may be utilized to present shivering or to treat seizures only if needed.
Prevention:
For athletes steps should include encouraging hydration (flavored drinks have been shown to increase consumption and improve hydration), developing strategies for acclimatization for athletes, and have materials present (ice baths) to intervene quickly for players with symptoms. For infants and young children car alarms or reminders, and practicing placing a needed item in the back seat can prevent parents from inadvertently leaving a child in a car.
Mangus CW, Canares TL. Heat-Related Illness in Children in an Era of Extreme Temperatures. Pediatr Rev. 2019 Mar;40(3):97-107. doi: 10.1542/pir.2017-0322. Epub 2019 Mar 1. PMID: 30824495.
Category: Pharmacology & Therapeutics
Keywords: sepsis, beta-lactam, vancomycin, antibiotic (PubMed Search)
Posted: 6/13/2025 by Alicia Pycraft
Click here to contact Alicia Pycraft
Background:
Early antibiotic administration is consistently linked to improved mortality outcomes in patients with sepsis. As a result, time-to-antibiotic delivery is a critical metric in hospital sepsis quality improvement initiatives. Empiric treatment often consists of a broad-spectrum beta-lactam to cover both gram-positive and gram-negative organisms, alongside vancomycin to ensure coverage of methicillin-resistant Staphylococcus aureus (MRSA). When multiple agents are indicated, they may be given simultaneously; however, factors such as limited intravenous (IV) access or drug incompatibilities can necessitate sequential administration. Administration of vancomycin first may delay the administration of a beta-lactam agent by at least 60-120 minutes due to its prolonged infusion time. This raises an important clinical question: Does the order in which antibiotics are administered influence outcomes in sepsis?
A 2022 retrospective study by Amoah et al. found that, among patients with confirmed bloodstream infections, a beta-lactam-first regimen was associated with a 52% reduction in the odds of short-term mortality compared to a vancomycin-first regimen. However, the generalizability of these findings to the broader population of patients with suspected sepsis, of whom only 15-20% ultimately have positive blood cultures, remains uncertain.
What's new?
A recent retrospective, multi-center, cohort study by Kondo et al. evaluated the impact of a beta-lactam-first antibiotic strategy compared to a vancomycin-first strategy on in-hospital mortality in patients with suspected sepsis. Of the 25,391 patients with sepsis who were screened, 21,449 (84.4%) received a beta-lactam first and 3,942 (15.6%) received vancomycin first. Patients who received vancomycin first had lower comorbidity burden, lower illness severity, more skin/musculoskeletal infections, and received beta lactams a median of 3.5 hours later relative to ED arrival compared to those who received a beta-lactam first. Although the overall rate of documented bloodstream infections was similar between groups, MRSA-positive cultures were more common in the vancomycin-first group, both in clinical cultures (4.5% vs. 3.2%) and in blood cultures (1.8 vs. 1.2%).
Beta-lactam administration prior to vancomycin was associated with an 11% reduction in the odds of in-hospital mortality (aOR: 0.89; 95% CI: 0.8-0.99; p=0.046). When the time-to-first antibiotic covariate was replaced with time-to-first beta-lactam, this association was no longer significant (aOR 0.93, 95% CI: 0.82-1.05, p=0.25), suggesting a possible link between time-to-first beta-lactam antibiotic and mortality. There was a trend toward lower in-hospital morality for the beta-lactam first regimen in several subgroups examined, including patients with positive blood cultures or positive MRSA cultures, and patients who received anti-pseudomonal beta-lactams; however, none reached statistical significance.
Bottom line:
Given the observed mortality benefit and absence of harm associated with a beta-lactam-first approach, even among patients with positive MRSA cultures, the findings of this study support the prioritization of beta-lactam therapy in patients with sepsis.
Category: Critical Care
Keywords: Cardiac Arrest, PEA, ROSC (PubMed Search)
Posted: 6/9/2025 by Harry Flaster, MD
Click here to contact Harry Flaster, MD
Pulse Checks in Cardiac Arrest: Your Fingers Are Not Reliable.
Summary: Whenever possible, use an ultrasound or an arterial line for pulse checks. Our fingers are not reliable.
Key points:
Multiple studies have demonstrated that manual pulse checks are not a reliable method to determine ROSC. Arterial lines and ultrasound are far more reliable methods. However, using more accurate measures of circulation lead to an additional dilemma: at what MAP, SBP, or ultrasound measured flow should we stop chest compressions? There is no agreed upon number, and as with most dilemmas in clinical medicine, the best answer is, “it depends”. However, a MAP > 50 or SBP > 60 for most patients is a reasonable choice to stop chest compressions. MAP < 50 or SBP < 60 are unlikely to provide adequate perfusion to the brain, and chest compressions should be resumed.
References:
Category: Obstetrics & Gynecology
Keywords: breech delivery (PubMed Search)
Posted: 6/9/2025 by Jennifer Wang, MD
(Updated: 2/2/2026)
Click here to contact Jennifer Wang, MD
Everyone clenches up when an imminent delivery shows up at the ED bay doors, even though most of these deliveries will not need intervention. Still, there are catastrophic ways delivery can go wrong, so today, let's talk about a new study on breech delivery.
The Study: Bogner et. al conducted a prospective single-center observational cohort study from 2006-2021 looking at breech deliveries in ~230 patients, with 92 of them being delivered in the traditional, supine way, while 140 of them delivered on all-fours. The only difference found between the two groups was that the all-fours group had heavier babies with bigger heads.
The Results: Over half (51.4%) of the patients in the all-fours position required no additional interventions from the provider compared to 11.9% of the supine group, and there were fewer perineal injuries. There was no increase in neonatal outcomes or NICU referrals in the all-fours group as compared to the supine group.
Limitations: Single center, no randomization, 11 patients started in all-fours and then had to switch to supine due to difficulty with delivery and prolonged second stage of labor, excluded footling breech
Takeaways: All-fours may be a position to consider for your patient with a breech delivery - especially if you haven't brushed up on your breech maneuvers recently.
Bogner G, Schuller J, Gargitter C, Dölzlmüller E, Fischer T, Fazelnia C. Vaginal breech delivery in all-fours position-Hands off instead of intervention: A prospective observational study. Acta Obstet Gynecol Scand. 2025;104(6):1153-1161. doi:10.1111/aogs.15078
Category: Trauma
Keywords: Hysterotomy (PubMed Search)
Posted: 6/8/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Another case series of 3 resuscitative hysterotomies, all performed by obstetricians, reported 33% maternal and 67% neonate survival.(1).
The mechanics of the procedure are:
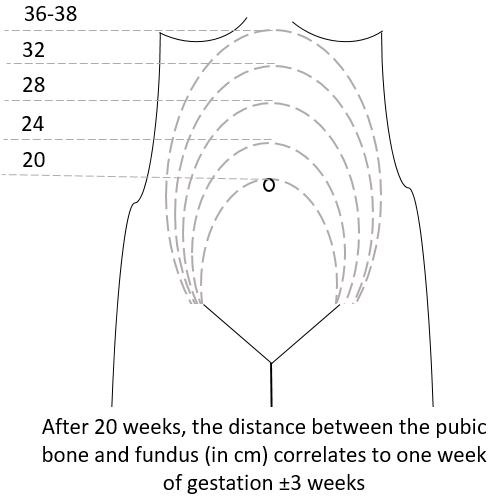
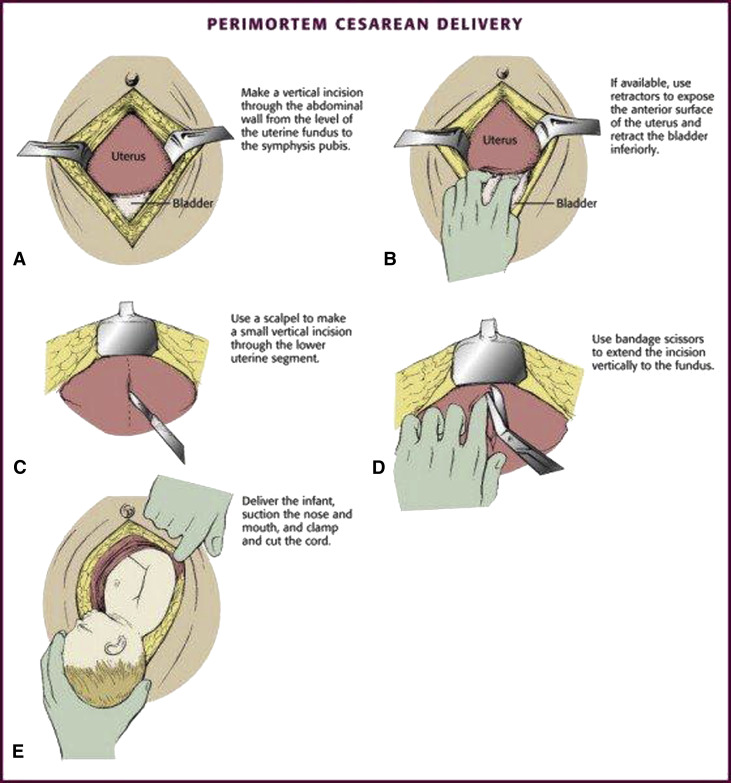
(3)
Category: Trauma
Posted: 6/7/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
A literature search revealed very little evidence, however in 66 women and 68 neonates who underwent resuscitative hysterotomy for out of hospital cardiac arrest 4.5% of women and 45% of neonates survived to discharge. The longest down time was 29 minutes and 47 minutes for women and neonates respectively. While more evidence is needed, it appears this procedure should be performed as early as possible and may lead to some survival benefit.
Leech C, Nutbeam T, Chu J, Knight M, Hinshaw K, Appleyard TL, Cowan S, Couper K, Yeung J. Maternal and neonatal outcomes following resuscitative hysterotomy for out of hospital cardiac arrest: A systematic review. Resuscitation. 2025 Feb;207:110479. doi: 10.1016/j.resuscitation.2024.110479. Epub 2024 Dec 29. PMID: 39736393.
Category: Neurology
Keywords: ischemic stroke, thrombolysis, tpa, intracranial hemorrhage (PubMed Search)
Posted: 6/6/2025 by Nicholas Contillo, MD
(Updated: 2/2/2026)
Click here to contact Nicholas Contillo, MD
Acute ischemic strokes involving the posterior circulation have significantly lower rates of hemorrhagic transformation after thrombolysis compared to anterior circulation strokes, a difference attributed to smaller infarct sizes and greater “ischemic tolerance” in the posterior circulation.
Given this lower hemorrhage risk, the EXPECTS trial evaluated the safety and efficacy of extending the thrombolysis window to 4.5–24 hours in patients with acute posterior circulation ischemic stroke who were not candidates for endovascular thrombectomy. This randomized controlled trial, conducted across 30 sites in China, enrolled 234 adults with mainly mild posterior circulation stroke (median NIHSS 3) and no evidence of extensive infarction on CT. Participants were randomized to receive either intravenous alteplase or standard medical care within the 4.5–24 hour window after symptom onset.
The primary outcome of functional independence at 90 days (modified Rankin Scale 0–2) was achieved in 89.6% of the alteplase group versus 72.6% of the standard care group. Rates of symptomatic intracranial hemorrhage were low and similar between groups (1.7% alteplase vs. 0.9% standard care), and 90-day mortality was lower in the alteplase group (5.2% vs. 8.5%).
These findings support extending the therapeutic window for intravenous thrombolysis in posterior circulation stroke beyond 4.5 hours when thrombectomy is not an option. However, the trial’s limitations, including a study population predominantly with mild strokes, exclusion of patients with extensive infarction, and enrollment limited to Chinese centers, warrant further investigation in larger and more diverse populations.
Bottom Line: Within limitations, emerging evidence supports an extended thrombolytic window beyond 4.5 hours for patients with posterior circulation strokes who are ineligible for thrombectomy.
Yan S, Zhou Y, Lansberg MG, Liebeskind DS, Yuan C, Yu H, Chen F, Chen H, Zhang B, Mao L, Zhang X, Wang X, Zhang X, Chen Y, Zhou H, Zhong W, He Y, Chen K, Wang J, Chen H, Huang Y, Campbell BCV, Lou M; EXPECTS Group. Alteplase for Posterior Circulation Ischemic Stroke at 4.5 to 24 Hours. N Engl J Med. 2025 Apr 3;392(13):1288-1296. doi: 10.1056/NEJMoa2413344. PMID: 40174223.
Category: Trauma
Keywords: Femur fracture, splint (PubMed Search)
Posted: 6/6/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
The National Association of Emergency Medical Service Physicians reminds us that femur fractures rarely cause enough blood loss to cause hemodynamic instability (look for other sources), often have concomitant injuries in the pelvis or distal extremity, and can be effectively splinted either static or with traction (which has contraindications, complications, and technical hurdles).
John W. Lyng, Joshua G. Corsa, Philip S. Nawrocki, Brad D. Raetzke, Josh
Nackenson & Nichole Bosson (07 May 2025): Prehospital Trauma Compendium: Management
of Suspected Femoral Shaft Fractures – A position statement and resource document of
NAEMSP, Prehospital Emergency Care, DOI: 10.1080/10903127.2025.2493846
To link to this article: https://doi.org/10.1080/10903127.2025.2493846
Category: Critical Care
Keywords: OHCA, shockable rhythms, VF, ventricular fibrillation, defibrillation, AED, energy (PubMed Search)
Posted: 6/4/2025 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
A recent retrospective cohort study out of China investigated an escalating energy (200 > 300 > 360J) versus fixed energy (200 > 200 > 200 J) defibrillation strategy in OHCA with ventricular fibrillation requiring repeated defibrillations.
Notes:
Results:
Caveats:
Category: Trauma
Keywords: Nail gun injury, surgery, antibiotics (PubMed Search)
Posted: 5/31/2025 by Robert Flint, MD
(Updated: 6/1/2025)
Click here to contact Robert Flint, MD
An Australian retrospective study of 158 patients treated for nail gun injuries found those treated with operative debridement or with prophylactic antibiotics had no different 30 day infection rates compared to patients receiving no antibiotics.
Slater S, Vasudeva M, Mitra B, Sreedharan S. Penetrating nail gun injuries: Role of antibiotics and surgical management. Trauma. 2025;0(0). doi:10.1177/14604086251320524
Category: Neurology
Keywords: Seizure, pediatrics, ketamine (PubMed Search)
Posted: 5/31/2025 by Visiting Speaker
(Updated: 2/2/2026)
Click here to contact Visiting Speaker
Author: Matthew Jackson, MD
The Ket-Mid Study (1) is a recent RCT out of a tertiary center in a largely rural region of Egypt that evaluated combined ketamine (2 mg/kg) and midazolam (0.2 mg/kg) (ket-mid) to midazolam plus placebo (pla-mid) as the first line seizure abortive therapy. Children in the ket-mid group achieved 76% termination at 5 minutes compared to 21% of those in the pla-mid group (p<0.001). Adverse outcomes were rare, though the pla-mid group did have more hypotension.
Notably, the population included differed from that typically seen in the US. These kids were seizing for a long time, with a median seizure duration before IV meds of 34 minutes, and the benefit of ketamine on subgroup analysis seemed to shrink for those that were treated in less than 30 minutes. CNS infections were also much more common, accounting for the underlying pathology in 11% of cases. Important exclusion criteria also included trauma, inborn errors of metabolism, underlying CNS malignancy, and others not always known to EMS or ED clinicians at the time therapy begins.
1. Othman AA, Sadek AA, Ahmed EA, Abdelkreem E. Combined Ketamine and Midazolam Versus Midazolam Alone for Initial Treatment of Pediatric Generalized Convulsive Status Epilepticus (Ket-Mid Study): A Randomized Controlled Trial. Pediatr Neurol. 2025 Jun;167:24-32. doi: 10.1016/j.pediatrneurol.2025.03.011. Epub 2025 Mar 22. PMID: 40186980.
Category: Trauma
Keywords: geriatric, trauma, CT scan (PubMed Search)
Posted: 5/29/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This literature search from 1946-2023 looking at comparing selective use of CT scans vs whole body scans in geriatric trauma found no benefit of whole body CT in mortality, hospital length of stay or ED discharge. This study only included 15,000 pts over that very long time line. More robust, current work needs to be done on this important topic.
Tang P, Elkington O, Stevens S. Whole body CT-scan vs. selective CT-scan in geriatric trauma: Systematic review and meta-analysis. Trauma. 2025;0(0). doi:10.1177/14604086241304629
Category: Administration
Keywords: Artificial intelligence, Emergency department, emergency practice (PubMed Search)
Posted: 5/27/2025 by Mercedes Torres, MD
(Updated: 5/28/2025)
Click here to contact Mercedes Torres, MD
AI is probably already being used in your ED, like it or not…
This article is an excellent review of the ways that AI can be used in emergency medicine. (See blue boxes in the figure below for a visual representation of opportunities for AI to augment emergency care from start to finish.) The authors note that there will always be a role for human physicians in EDs; AI can serve as an adjunct rather than a replacement for physician care. Physicians should strive to be informed leaders in AI development to ensure it is performed in a cautious, thoughtful, patient-centered manner.
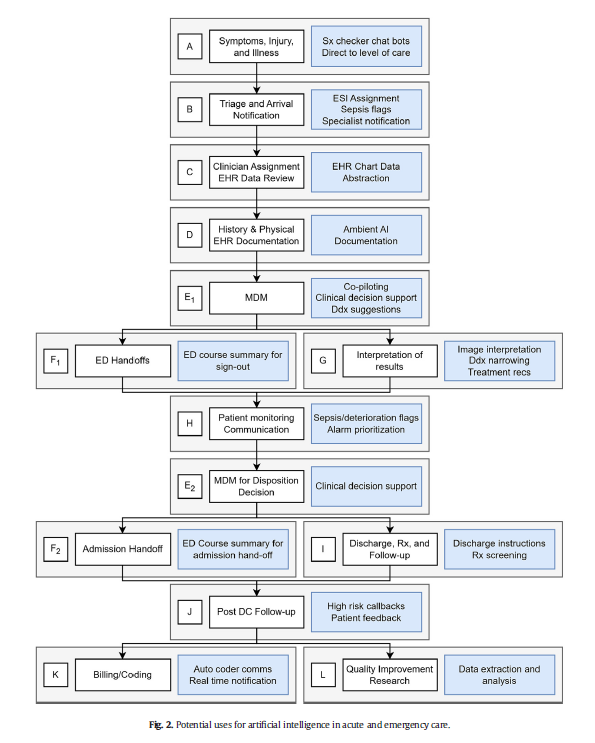
Marika M. Kachman, Irina Brennan, Jonathan J. Oskvarek, Tayab Waseem, Jesse M. Pines. How artificial intelligence could transform emergency care. The American Journal of Emergency Medicine, Volume 81, 2024, Pages 40-46, https://doi.org/10.1016/j.ajem.2024.04.024.
Category: Critical Care
Posted: 5/27/2025 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
We have known that resuscitation with balanced crystalloids was associated with better outcomes, than normal saline. However, I have believed that in the early phase of resuscitation, volume of any crystalloids is still better than little volume. Thus, a couple of liters of normal saline (0.9% saline) would not hurt. However, the recent secondary analysis from the Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis (CLOVERS) trial might have changed my practice.
-----
Settings:
60 ICU in the United States between 2018 to 2022. This is the secondary analysis of the Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis (CLOVERS) trial population
Participants: Patients with sepsis-induced hypotension after receiving fluid resuscitation (from 1-3 litters). Participants who received lactate ringers (622 patients) were compared with patients who received normal saline (690 patients).
Outcome measurement:
Death before discharge home by day 90.
Hospital-free days at 28 days
Study Results:
Dead occurred in 12.2% of LR group (76/622) vs. 15.9% (110/690) patients of the NS group, Adjusted Hazard Ratio 0.71 (95% CI 0.51-0.99, p=0.043)
Patients receiving LR had more hospital-free days at 28 days than those receiving 0.9% saline (16.6 ± 10.8 vs. 15.4 ± 11.4 d, respectively). The mean difference was 1.6 days (95% CI, 0.4–2.8; p = 0.009).
Discussion:
This study confirms that not only early resuscitation is important, but the fluid choice during the early resuscitation phase is also important, especially in patients with signs and symptoms of sepsis.
Thus, even during pre-hospital phase and in the ED, clinicians should consider to use LR or other balanced solutions if available.
Conclusion:
Among patients with sepsis-induced hypotension, resuscitation with Lactate Ringer was associated with better outcomes than normal saline.
Gelbenegger G, Shapiro NI, Zeitlinger M, Jilma B, Douglas IS, Jorda A. Lactated Ringer's or Normal Saline for Initial Fluid Resuscitation in Sepsis-Induced Hypotension. Crit Care Med. 2025 May 1;53(5):e1140-e1144. doi: 10.1097/CCM.0000000000006601. Epub 2025 Feb 19. PMID: 39969246; PMCID: PMC12047640.
Category: Infectious Disease
Keywords: Coccidioidomycosis, climate change (PubMed Search)
Posted: 5/26/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Typically Coccidioidomycosis is seen in the Southwestern US. The authors of this study, using climate modeling predict endemic areas will spread across the US to include Idaho, the Dakotas, Nebraska and Wyoming.
Clinically, “Patients with pulmonary Coccidioides infection frequently experience fever, cough, and shortness of breath. Chest radiographic imaging may demonstrate lobar, segmental, or multifocal consolidations; cavitary lesions; and lung nodules. Given these nonspecific findings, patients with coccidioidomycosis are often treated for community-acquired pneumonia. Coccidioidomycosis should be considered in patients not improving with antibiotic treatment or in those who have exposure to or reside in endemic areas. Up to 50% of patients with pulmonary coccidioidomycosis have erythema nodosum, approximately 25% to 30% have peripheral eosinophilia, and approximately 25% have arthralgias (particularly symmetric knee and ankle arthralgia). Up to 10% of patients diagnosed with coccidioidomycosis develop disseminated disease, including skin, central nervous system, and bone and joint infection.”
Lee PS, Swain DL, Johnson R. Climate Change and Coccidioidomycosis. JAMA. 2025;333(11):997–998. doi:10.1001/jama.2024.27274
