Category: Trauma
Keywords: Frail, trauma, mortality, outcome (PubMed Search)
Posted: 1/12/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
The Trauma Frailty Index has been validated to predict inpatient mortality, major complications and discharge to rehab facility. “In addition, frailty was significantly associated with higher adjusted odds of mortality, major complications, readmissions, and fall recurrence at 3 months postdischarge ( p < 0.05).”
It is a simple 15 variable index.

Joseph B, Saljuqi AT, Amos JD, Teichman A, Whitmill ML, Anand T, Hosseinpour H, Burruss SK, Dunn JA, Najafi K, Godat LN, Enniss TM, Shoultz TH, Egodage T, Bongiovanni T, Hazelton JP, Colling KP, Costantini TW, Stein DM, Schroeppel TJ, Nahmias J; AAST Frailty MIT Study Group. Prospective validation and application of the Trauma-Specific Frailty Index: Results of an American Association for the Surgery of Trauma multi-institutional observational trial. J Trauma Acute Care Surg. 2023 Jan 1;94(1):36-44. doi: 10.1097/TA.0000000000003817. Epub 2022 Oct 17. PMID: 36279368.
Category: Orthopedics
Posted: 1/11/2025 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Calcium pyrophosphate deposition disease (CPPD), AKA pseudogout.
Calcium crystal deposits form on articular surfaces.
This MAY trigger an inflammatory synovitis. Also can be asymptomatic.
Degenerative changes occur to the affected joint over time
CC: Moderate to severe pain, tenderness to palpation, stiffness, redness, warmth and decreased ROM.
May appear as punctate linear densities within the articular cartilage.
Joint fluid analysis: Weakly positive birefringent rhomboid shaped crystals.
Differential diagnosis: Calcified meniscus and Septic knee
Category: Pharmacology & Therapeutics
Keywords: olanzapine, benzodiazepine, drug interaction (PubMed Search)
Posted: 1/10/2025 by Alicia Pycraft
Click here to contact Alicia Pycraft
Background
Treatment of acute agitation often involves combining antipsychotics and benzodiazepines. Injectable olanzapine, a second-generation antipsychotic, uniquely carries a warning against concomitant use with parenteral benzodiazepines. The olanzapine prescribing information states that “concomitant administration of intramuscular (IM) olanzapine and parenteral benzodiazepines is not recommended due to the potential for excessive sedation and cardiorespiratory compromise”. The European Medicines Agency (similar to the United States FDA) cautions against use of the two within 60 minutes of each other using similar language.
The above warnings were based on a 2010 publication of 160 adverse event reports from a post-marketing database maintained by the drug manufacturer, and have resulted in many institutions prohibiting co-administration of IM olanzapine and parenteral benzodiazepines. The publication cited 29 fatal adverse events involving injectable olanzapine, concluding that caution should be exercised when using IM olanzapine and parenteral benzodiazepines simultaneously. However, 25 of the 29 patients received other sedating medications in addition to olanzapine and benzodiazepines, and the majority of fatalities were >12 hours after the last dose of olanzapine. Following this publication, a 2013 randomized controlled trial by Chan et al. found no difference in adverse event rates between patients receiving IV midazolam alone and patients receiving IV midazolam plus IV olanzapine for acute agitation.
This December 2024 study by Cole et al. aimed to re-evaluate the risks of cardiorespiratory compromise with concomitant injectable olanzapine and injectable benzodiazepine administration.
Study design
This was a single-center retrospective cohort study of 693 patients who received 2 parenteral doses of eligible sedating medications within 60 minutes of each other. A total of 549 patients received 2 doses of olanzapine, and 144 received olanzapine and a benzodiazepine (midazolam, lorazepam, or diazepam). To avoid cohorts with a higher baseline risk of sedation, patients who received other sedating medications and patients who received more than 2 doses of olanzapine or 1 dose of a benzodiazepine were excluded.
Patient Population
Results

*One death during hospitalization was due to missed occlusion myocardial infarction
Study Critique:
Key Takeaways
Category: Critical Care
Posted: 1/8/2025 by William Teeter, MD
Click here to contact William Teeter, MD
Extracorporeal cardiopulmonary resuscitation (ECPR) is a type of extracorporeal support following cardiac arrest available at a small, but growing number of ECMO centers around the world. After some initial promising results, more recent data have been mixed. There is a nice narrative review in JACEP Open recently which summarizes the most recent evidence. Implementation considerations and patient selection seemingly drive the variance seen in the studies reviewed.
To this point, a new article from Critical Care Medicine was just published looking at the outcomes of eCPR with respect to age using 5 years of ELSO patient data. Unsurprisingly, advancing age is associated with worse outcomes, with significantly reduced odds of survival above the age of 65.
Category: Critical Care
Keywords: Frailty, morbidity, mortality, geriatric (PubMed Search)
Posted: 1/5/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
The level of fitness/health a patient has entering the marathon of recovery from critical illness or trauma has a major impact on morbidity and mortality. Frailty is a measure of this fitness level. The clinical frailty scale can be used to assess your patients ability to survive critical illness. Age is a number. Frailty is more useful.


Category: Cardiology
Keywords: Hypertension, MACE, end organ (PubMed Search)
Posted: 1/4/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study followed patients presenting to the ED with elevated (SBP>180, DBP>120) blood pressure without evidence of end organ dysfunction for one year. The patients were followed for major adverse cardiac events. They found:
“A total of 12,044 patients were enrolled. The prevalence of MACE within one year was 1,865 (15.5%). Older age, male gender, history of cardiovascular disease, cerebrovascular disease, diabetes, smoking, presentation with chest pain, altered mental status, dyspnea, treatment with intravenous and oral hydralazine, and oral metoprolol were independent predictors for one-year MACE. Additionally, discharge with an SBP ?160 mm Hg was not associated with 30-day MACE-free survival after propensity matching (hazard ratio 0.99, 95% confidence interval 0.78–1.25, P?=?0.92).”
Treating to reach a magic number did not help. Most likely, long term control of blood pressure is a more important factor than attempts to lower in the ED. While this is a high risk group, there is no evidence that acute lowering of blood pressure impacts long term survival.
Category: Critical Care
Keywords: post-intensive care syndrome, PICS, PICS-F (PubMed Search)
Posted: 12/31/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Post-Intensive Care Syndrome (PICS) is an increasingly recognized phenomenon of impairment of physical, cognitive, and/or mental health after intensive care admission. Even more recently, similar deficits in caregivers of patients admitted to the ICU, often called Post-Intensive Care Syndrome Family (PICS-F) is increasingly recognized. A study recently published by Watland et al in Critical Care Medicine looking at reducing PICS-F through a “caregiver pathway” got me wondering if there's any literature out there about reducing PICS-F via interventions in the emergency department. Patients' treatment course in the ED is a highly stressful and uncertain time for both the patient and family members, so it stands to reason this is an impactful period where intervention may help, and even in patients where their condition is too advanced for us to make a medical difference, our actions could have a positive impact on long term outcomes for the family members.
The short answer is no, to this author's knowledge and based on my review of the literature, there is no good evidence for reducing PICS-F by ED interventions (hint, hint: if anyone's looking for a good area to study…) Based on evidence from the critical care realm, the following are probably reasonable approaches that would translate well to the ED:
Watland, Solbjørg RN, MS1,,2,3; Solberg Nes, Lise LP, PhD1,,3,,4; Ekeberg, Øivind MD, PhD5; Rostrup, Morten MD, PhD2,,6; Hanson, Elizabeth RN; PhD7,,8; Ekstedt, Mirjam RN, PhD7,,9; Stenberg, Una PhD10,,11; Hagen, Milada PhD12; Børøsund, Elin RN, PhD1,,13. The Caregiver Pathway Intervention Can Contribute to Reduced Post-Intensive Care Syndrome Among Family Caregivers of ICU Survivors: A Randomized Controlled Trial. Critical Care Medicine ():10.1097/CCM.0000000000006546, December 24, 2024. | DOI: 10.1097/CCM.0000000000006546
Shirasaki K, Hifumi T, Nakanishi N, Nosaka N, Miyamoto K, Komachi MH, Haruna J, Inoue S, Otani N. Postintensive care syndrome family: A comprehensive review. Acute Med Surg. 2024 Mar 11;11(1):e939. doi: 10.1002/ams2.939. PMID: 38476451; PMCID: PMC10928249.
Category: Trauma
Keywords: chest injury, exercise, chronic pain, (PubMed Search)
Posted: 12/30/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study suggests no. The control arm was given standard physical therapy and the intervention arm was instructed in four basic exercises to do on their own daily for a week. Patents were then surveyed to assess for long term pain. There was no difference in pain between the two groups. Meaning, at least in this study reliant on patient journaling and follow up, that these four simple exercises did not impact long term pain in chest wall injured patients. More work needs to be done in this important area.
Cheri Battle, Timothy Driscoll, Deborah Fitzsimmons, Shaun Harris, Fiona Lecky, Claire O'Neill, Alan Watkins, Jane Barnett, Susan Davies, Hayley Anne Hutchings, Kate Jones, Andrew Eglington, Sophie Place, Hannah Toghill, Katie Foster, Bethan Uzzell, Elizabeth Ford, Mark Baker, Sophie Lewis, Sara Davies, Sarah Nicholls, Amy Charnock, Claire Watkins, Sarah-Jane Garside, Jeannie Bishop, Thomas Dawson, Jessica Pendlebury, Reece Doonan,
EarLy Exercise in blunt Chest wall Trauma: A multi-centre, parallel randomised controlled trial (ELECT2 Trial),
Injury,
2024,
112075,
ISSN 0020-1383,
https://doi.org/10.1016/j.injury.2024.112075.C
Category: Critical Care
Keywords: agitation, choking, hypoxia, acidosis, breathing (PubMed Search)
Posted: 12/29/2024 by Steve Schenkel, MPP, MD
(Updated: 2/2/2026)
Click here to contact Steve Schenkel, MPP, MD
In a fascinating perspective piece, Matt Bivens and colleagues explain that the combination of struggle and restraint leads to death not because of hypoxia, but because of acidosis.
The sequence is something like this: exertion or struggle results in an acidotic state -> restraint reduces respiratory ability, especially when held prone or weight is applied to back or chest -> acidosis worsens with the potential for cardiac arrhythmia and arrest.
In this setting, “I can’t breathe” does not mean that there is no air movement over the vocal cords but that respiration is impaired, much as it is in asthma or obstructive lung disease.
Use of sedation in this setting reduces respiration even further, worsening acidosis and risking death. It’s not hypoxia that kills; it’s acidosis.
See the complete perspective here: https://www.nejm.org/doi/full/10.1056/NEJMp2407162.
Bivens M, Jaeger E, Weedn V. Handcuffs and Unexpected Deaths — “I Can’t Breathe” as a Medical Emergency. NEJM 2024; 391:2068-9. DOI: 10.1056/NEJMp2407162
Category: Orthopedics
Posted: 12/28/2024 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
A stinger is a short lived neuropraxia to the upper brachial plexus
Named for the temporary sensation that radiates from the shoulder to the hand
Can occur though 3 common mechanisms
Most commonly from direct traumatic or tractional injury
https://www.physio-network.com/wp-content/uploads/2021/11/unnamed-1.png
Common in American Football
Occurs in almost 50% of players over a 4-year college career
Most commonly to running backs and linebackers in one NFL study
Symptoms: Unilateral burning pain and tingling in the arm with transient weakness
Symptoms NOT confined to a single dermatome.
Usually in C5, C6 innervated muscles (deltoid and biceps).
Symptoms are transient usually resolving in approximately 2 minutes
If asked to examine someone for this at a sporting event
Evaluate patient for:
C spine tenderness
Full cervical range of motion
UNILATERAL weakness in shoulder Abductors and external rotators
UNILATERAL weakness in biceps
UNILATERAL weakness in forearm pronation
UNILATERAL weakness in triceps extension
Consider evaluation for concussion symptoms if appropriate
Majority of patients in college and profession sports return to play in game when exam returns to normal
Category: Administration
Keywords: push notification, EMR, ED flow, results, radiology (PubMed Search)
Posted: 12/26/2024 by Steve Schenkel, MPP, MD
(Updated: 2/2/2026)
Click here to contact Steve Schenkel, MPP, MD
Clinical practice in the world of the Electronic Medical Record has made many a clinician question the value of electronic reminders.
Banners warn of sepsis, the need for repeat evaluation, vital signs outside expected limits, wait times, and risks for readmission.
Can they instead help ED flow?
Sayan Dutta and colleagues suggest that they can. When clinicians chose to receive notice of a lab or imaging result, push notification reduced time between final result and ED disposition by 18 minutes (95% CI: 15-21 minutes).
The likely key here? Clinicians actively chose when and about what to be notified.
See: Result Push Notifications Improve Time to Emergency Department Disposition: A Pragmatic Observational Study, Annals of Emergency Medicine, 85(1), 53-62. https://www.annemergmed.com/article/S0196-0644(24)00404-9/abstract.
Result Push Notifications Improve Time to Emergency Department Disposition: A Pragmatic Observational Study
Dutta, Sayon et al.
Annals of Emergency Medicine, Volume 85, Issue 1, 53 - 62
Category: Misc
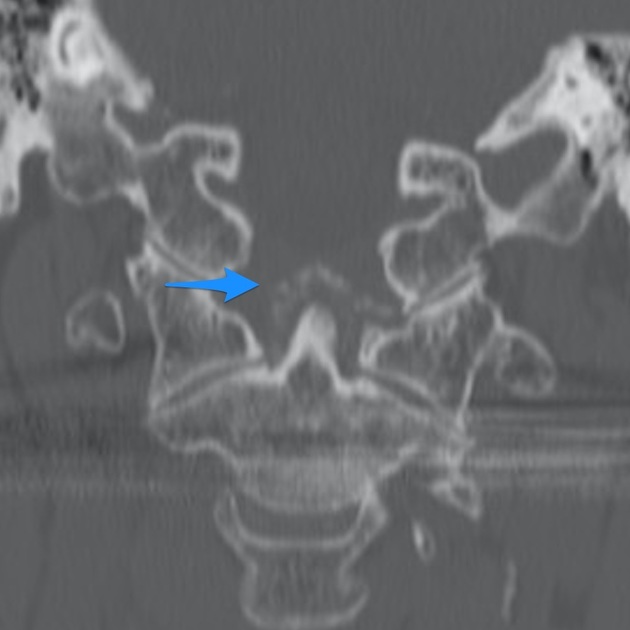
Keywords: Neck pain, crowned dens syndrome (PubMed Search)
Posted: 12/22/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Crowned dens syndrome is an acute inflammatory disease caused by deposition of calcium pyrophosphate dihydrate crystals or hydroxyapatite crystals in the soft tissue and ligaments surrounding the dense. Patient presentation is severe pain in the neck and base of the skull, low grade fever, and elevated inflammatory markers. It is most commonly seen in elderly females. Ct scan is the gold standard for diagnosis. Once meningitis and other significant infectious process has been excluded, treatment is anti inflammatory medications including steroids.
Category: Pediatrics
Keywords: nasal suctioning, rsv, bronchiolitis (PubMed Search)
Posted: 12/18/2024 by Jenny Guyther, MD
(Updated: 12/20/2024)
Click here to contact Jenny Guyther, MD
Infants are typically obligate nasal breathers and the increased mucus production associated with bronchiolitis can impair both breathing and feeding. AAP bronchiolitis guidelines state that the routine use of deep suctioning may not be beneficial.
This was an observational study of 121 infants aged 2-23 months with bronchiolitis who received either nasal suction (31), deep suction (68) or a combination (52). Groups were based on clinician discretion. Respiratory scores and pulse ox were obtained pre-suction and at 30 and 60 minutes post suction.
There was no difference between suction type and respiratory score. However, there was an improvement in respiratory score between the 0-30 and 0-60 time point with any suctioning. Suction type had no effect on pulse ox, airway adjunct escalation, length of stay or outpatient outcomes.
The study also showed no association between albuterol use and respiratory scores (albuterol is not recommended by the AAP in the management of bronchiolitis).
Bottom line: In this small study, nasal aspiration and deep suction appear to be equal in improving respiratory scores up to 1 hour post suction suggesting that deep suctioning may not be needed.
Hedland JL, Chang TP, Schmidt AR, Festekjian A. Suctioning in the management of bronchiolitis: A prospective observational study. Am J Emerg Med. 2024;82:57-62. doi:10.1016/j.ajem.2024.05.013
Category: Airway Management
Keywords: Ketamine, etomidate, RSI, induction (PubMed Search)
Posted: 12/19/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Another large database evaluation of the use of etomidate vs. ketamine as an induction agent for intubation found a trend toward higher mortality in the etomidate group. Even when trying to control for steroid use (to control for etomidate’s possible adrenal suppression), etomidate had a higher mortality rate.
A well done study that adds to the chorus advocating for choosing ketamine when looking for a hemodynamically neutral induction agent.
Wunsch H, Bosch NA, Law AC, Vail EA, Hua M, Shen BH, Lindenauer PK, Juurlink DN, Walkey AJ, Gershengorn HB. Evaluation of Etomidate Use and Association with Mortality Compared with Ketamine among Critically Ill Patients. Am J Respir Crit Care Med. 2024 Nov 15;210(10):1243-1251. doi: 10.1164/rccm.202404-0813OC. PMID: 39173173.
Category: EMS
Keywords: cardiac arrest, hypoxia, CPR bystander (PubMed Search)
Posted: 12/18/2024 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
This was a review of the cardiac arrest registry of Norway between 2016-2021. The incidence of pediatric out of hospital cardiac arrests was 4.6 per 100,000 child years and significantly higher in children < 1 year (20.9 per 100,000 child years). There was an overall 18% one year survival rate in the 308 patients included.
Leading causes of arrests were choking, respiratory disease, drowning and SIDS, making up 67% of cases.
73% of the arrests were initially asystolic and 14% were PEA on EMS arrival. The presence of shockable rhythms increased with age and VT/VF were the initial rhythm in up to 15% of the 13-17 year age group.
88% of patients received bystander CPR ( with 68% receiving both chest compressions and ventilations). A minority of these patients were in a shockable rhythm, but 7 total patients were in refractory VF. Mechanical CPR devices were used in 35 patients aged 11-17. ECMO was started in 19 cases.
Bottom line: The rate of bystander CPR in this study was very high and other jurisdictions can attempt to learn from the system in place in Norway to increase their local prehospital interventions.
Kelpanides IK, Katzenschlager S, Skogvoll E, et al. Out-of-hospital cardiac arrest in children in Norway: A national cohort study, 2016-2021. Resusc Plus. 2024;18:100662. Published 2024 May 18. doi:10.1016/j.resplu.2024.100662
Category: Critical Care
Posted: 12/17/2024 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
High-Intensity NIPPV for Acute COPD Exacerbations?
Luo Z, et al. Effect of high-intensity vs low-intensity noninvasive positive pressure ventilation on the need for endotracheal intubation in patients with an acute exacerbation of chronic obstructive pulmonary disease. JAMA. Published online September 2024.
Category: Ultrasound
Keywords: POCUS, vascular access, pediatrics (PubMed Search)
Posted: 12/16/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
In adult patients, ultrasound-guided long catheter IVs for difficult venous access have been shown to provide increased duration of use, reduced complication rates, and greater cost-effectiveness.
However, there are relatively few studies examining the use of ultrasound for IV access in pediatric patients.
A recent study, the DIAPEDUS study, investigated the success rate of peripheral IV access with and without ultrasound assistance in pediatric patients with difficult venous access.
The study included 110 pediatric patients. IVs were placed by 25 nurses and 6 pediatricians, each of whom had completed departmental training involving at least 20 ultrasound-guided IV placements prior to the study.
The results showed a significantly higher success rate on the first attempt with ultrasound-guided techniques (90% vs. 18%), along with reduced procedural time and fewer attempts overall.
Bottom Line: For patients with known difficult venous access, ultrasound-guided IV placement should be the first-line approach.
D'Alessandro M, Ricci M, Bellini T, Chianucci B, Calevo MG, Piccotti E, Moscatelli A. Difficult Intravascular Access in Pediatric Emergency Department: The Ultrasound-Assisted Strategy (DIAPEDUS Study). J Intensive Care Med. 2024 Mar;39(3):217-221. doi: 10.1177/08850666231199050
Bahl A, Johnson S, Hijazi M, Mielke N, Chen NW. Cost effectiveness of ultrasound-guided long peripheral catheters in difficult vascular access patients. J Vasc Access. 2024 Jul;25(4):1204-1211. doi: 10.1177/11297298231154297.
Category: Trauma
Keywords: Trauma, oxygen, mortality (PubMed Search)
Posted: 12/14/2024 by Robert Flint, MD
(Updated: 12/15/2024)
Click here to contact Robert Flint, MD
In this randomized trial of restrictive oxygen (arterial oxygen sat of 94% ) vs. liberal oxygen (12-15 L of O2 per minute) for 8 hours after traumatic injury there was no difference in mortality or major respiratory complications at 30 days between the two groups.
Further evidence that managing hypoxia is important but over oxygenation at best offers no benefit and may add harm.
Arleth T, Baekgaard J, Siersma V, et al. Early Restrictive vs Liberal Oxygen for Trauma Patients: The TRAUMOX2 Randomized Clinical Trial. JAMA. Published online December 10, 2024. doi:10.1001/jama.2024.25786
Category: Cardiology
Posted: 12/14/2024 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Cardiovascular disease (CVD) is the leading cause of death both in the United States and globally for both men and women.
Major adverse cardiovascular events (MACE) is a commonly used composite outcome.
MACE is defined as non-fatal stroke/acute myocardial infarction/heart failure or cardiovascular death.
Physical inactivity is a leading risk factor for noncommunicable diseases and death worldwide
Up to 5 million deaths/yr could be averted with increased physical activity
Regular physical activity reduces the risk of many types of cancer by 8-28%, diabetes by 17%, heart disease and CVA by 19%, and dementia by 20%.
Many adults and children find meeting the recommended physical activity goals very challenging.
A recent observational study found that just 1.5-to-4-minute small bursts of high intensity exercise throughout the day may help lower an individual’s risk of MACE.
To clarify, this does not mean going to the gym to do a 45-minute HIIT class
Vigorous intermittent lifestyle physical activity (VILPA) involves such simple things as carrying the groceries a short distance or taking the work stairs instead of the elevator.
Such activities are more feasible for all of us vs structured exercise for obvious reasons.
Study group was >100,000 middle-aged men and women. Average age 61.
All participants wore an activity tracker continuously for a full week.
This data was used to calculate VILPA bouts throughout the day.
Female participants with no formal exercise regimen who recorded just 3.4 minutes of VILPA a day were 50% less likely to have a MI, had a 67% decreased risk for heart failure and 45% less likely to develop any type of MACE vs those who did not clock any VILPA during their day.
Female participants who recorded just 1.2-1.6 minutes of VILPA a day had a 33% lower risk of MI, 40% decreased risk of heart failure and 30% lower risk of MACE.
In male participants, those with 5.6 minutes of VILPA each day had a 16% reduced risk of having MACE than those who did not have any VILPA.
Differences may be due to women’s VILPA intensity was roughly 20% greater than men
Conclusion: Take the stairs
Stamatakis E, et al. Device-measured vigorous intermittent lifestyle physical activity (VILPA) and major adverse cardiovascular events: evidence of sex differences. Br J Sports Med. 2024 Oct 28
Category: Pediatrics
Keywords: pediatrics, seizure, infant, epilepsy, spams, infantile spasms (PubMed Search)
Posted: 12/13/2024 by Kathleen Stephanos, MD
(Updated: 2/2/2026)
Click here to contact Kathleen Stephanos, MD
Infantile Spasms (now known as Infantile Epileptic Spasms Syndrome- IESS) is a subtle, can't miss diagnosis occurring in children under the age of 2, with 90% presenting before 1 year of age.
History:
Presentation for these patients can be sporadic, recurrent, flexion or extension of the limbs or head. The patient typically remains alert during an episode, but they can be startled or appear uncomfortable from the sudden movement.
With smart phone use, parents often have videos of the events that a provider can see as they are often no events in the ED.
Prognosis is very poor with up to 50% having long-term neuro-cognitive complications or regression.
Examination:
A complete physical exam should be performed with particular attention to focal neurologic deficits which would require emergent imaging, signs of electrolyte abnormalities (eg. Chvostek's sign in hypocalcemia), and evidence of neurocutenous syndromes (eg. Neurofibromatosis, tuberous sclerosis).
Testing:
Diagnosis is made with EEG showing hypsarrhythmia. This should be done as soon as possible, most often requiring an inpatient admission.
Lab work can be done to exclude other possible causes of abnormal movements including assessing for electrolyte abnormalities.
Imaging in the ED is not typically indicated unless there is concern based on exam. MRI is the imaging modality of choice, and is often completed after EEG confirmed diagnosis.
Treatment:
Management is initiated in conjunction with a pediatric neurologist with most common therapies being corticotropin (ACTH) and vigabatrin.
Smith MS, Matthews R, Rajnik M, Mukherji P. Infantile Epileptic Spasms Syndrome (West Syndrome). 2024 Feb 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30725936.
