Category: EMS
Keywords: refusal, AMA, online medical direction (PubMed Search)
Posted: 10/16/2024 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
EMS may call the hospital to obtain online medical direction when a patient does not wish to come to the hospital. One difficult task faced by the physician at the hospital is determining the decision making capacity of the patient. There is currently no nationally recognized standard protocol for physicians providing EMS oversight in this situation.
The four components involved in the determination of capacity are: understanding, appreciation, reasoning and expression of choice. This study used a modified Delphi approach with 19 physician experts to develop standardized steps to guide best practices for physicians who are called in real time about a patient refusing EMS transport. Consensus was defined as 80% agreement.
The example worksheet with the compilation of recommendations is attached.
Carrillo, E. A., Ignell, S. P., Wulfovich, S., Vernon, M. J., & Sebok-Syer, S. S. (2024). Critical Steps for Determining Capacity to Refuse Emergency Medical Services Transport: A Modified Delphi Study. Prehospital Emergency Care, 1–6. https://doi.org/10.1080/10903127.2024.2403650
Category: Critical Care
Keywords: vascular access, micropuncture kits, procedures (PubMed Search)
Posted: 10/15/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Getting reliable venous and arterial access is crucial when resuscitating critically ill patients. These lines can be difficult due to patient and situation specific variables.
Micropuncture kits contain a 21-gauge echogenic needle, a stainless-steel hard shaft/soft-tip wire, and a 4 Fr or 5 Fr sheath and introducer. The micropuncture kit offers several advantages that can help overcome difficult situations:
To use a micropuncture kit, gain vessel access with the needle and wire, railroad the sheath and introducer into the vessel, remove the wire, then remove the introducer. Now you have a 4 Fr or 5 Fr sheath in the vessel. This is typically used to introduce a normal central line wire.
For arterial lines, you can place them directly over the wire without dilation. Keep in mind that the 4 Fr sheath (1.3 mm OD) and 5 Fr sheath (1.7 mm OD) are larger than a typical arterial line catheter (18g = 1.27 mm OD). If you dilate then you will cause hematoma.
Find out where your department stores micropuncture kits and get familiar with their components. While it adds an extra step to the procedure, it could make the difference between securing the line or not.
Montrief, T., Ramzy, M., & Long, B. (2021). Micropuncture kits for difficult vascular access. The American journal of emergency medicine.
Category: Trauma
Keywords: Rectal injury trauma (PubMed Search)
Posted: 10/13/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Rectal injuries are rare. The majority are secondary to penetrating injuries. Trauma care providers “should have a high clinical suspicion of rectal injury with any missile with a trajectory near the rectum; transpelvic gunshot wounds; stab injuries near the perineum, buttocks, groin, or proximal thighs; or open pelvic fractures. A digital rectal examination with a focus on sphincter tone, presence of blood, palpable defect, or bony protrusion should be carried out. Of note, a normal digital rectal examination does not exclude rectal injury.”
Ct scan with IV contrast (not PO or rectal) is used to identify rectal injuries but will be diagnostic in only 33% of injuries.
Rectal Injury Grading Scale
| Grade | Injury Type | Description of Injury |
|---|---|---|
| I | Hematoma laceration | Hematoma or hematoma without devascularization Partial-thickness laceration |
| II | Laceration | Laceration <50% of circumference |
| III | Laceration | Laceration ?50% of circumference |
| IV | Laceration | Full-thickness laceration with extension into perineum |
| V | Vascular | Devascularized segment |
Fields, Adam MD, MPH; Salim, Ali MD, FACS
Journal of Trauma and Acute Care Surgery 97(4):p 497-504, October 2024. | DOI: 10.1097/TA.0000000000004352
Category: Orthopedics
Posted: 10/12/2024 by Brian Corwell, MD
(Updated: 10/13/2024)
Click here to contact Brian Corwell, MD
Shoulder Abduction Test aka Bakody’s Sign
Used clinically in the evaluation of patients with suspected cervical radiculopathy
Unlike Spurling’s test, where we create discomfort, this test attempts to relieve it.
Specifically, evaluates for nerve root compression at C4-C6/7
To perform:
Arm Abduction can be active or passive
3. Instruct the patient to hold this position for 30 seconds.
4.Observe the patient for any relief of symptoms (A positive test)
Decrease in pain, numbness, weakness or tingling
5. Repeat on the unaffected side for comparison.
Sensitivity: 17–78% Specificity: 75–92%
Note: when asked about what alleviates their pain, patients will frequently describe and demonstrate the maneuver.
Consider adding this simple maneuver in your assessment of patients with suspected symptomatic cervical radiculopathy
Category: Pediatrics
Keywords: pediatrics, electrolyte, sodium (PubMed Search)
Posted: 7/5/2024 by Kathleen Stephanos, MD
(Updated: 10/11/2024)
Click here to contact Kathleen Stephanos, MD
Hypernatremia in Pediatric patients is less common than other electrolyte abnormalities occurring in <1% of hospitalized patients. The most common cause is water loss, either from poor absorption in the cases of vomiting, diarrhea, malabsorption or insensible losses, or via diabetes insipidus. Congenital disorders may cause decreased thirst receptors resulting in inadequate intake. Finally, excess sodium intake can occur via hypertonic fluids, ingestions or hyperaldosteronism or hypercortisolism.
Symptoms are often nonspecific- including fatigue, vomiting, hypertonia or hyperreflexia in lower states, but may result in lethargy, mental status changes or seizures as levels approach and exceed 160mmol/L
Treatment is similar to adults - free water deficit should be calculated:
Total body water (%) x weight (kg) x [(serum Na)/140 - 1]
Total Body Water (TBW) varies by age:
24-31 weeks- 90%
32-35 weeks - 80%
Term - 12 months - 70%
12 months and up - 60%
IV fluids should be started with a goal of decreasing the sodium level by 0.5 mmol/L/h with close monitoring of sodium levels.
Brown DH, Paloian NJ. Hypokalemia/Hyperkalemia and Hyponatremia/Hypernatremia. Pediatr Rev. 2023 Jul 1;44(7):349-362. doi: 10.1542/pir.2021-005119. PMID: 37391630.
Category: Obstetrics & Gynecology
Keywords: alloimmunization, pregnancy, RhoGAM (PubMed Search)
Posted: 10/10/2024 by Michele Callahan, MD
Click here to contact Michele Callahan, MD
Historically, there has been limited and inconclusive data regarding the utility of Rh (D) immunoglobulin (RhIg) in preventing alloimmunization for patients with early pregnancy loss or abortion at <12 weeks gestation. Although previous guidelines recommended routine administration of RhIg in Rh(-) patients after abortion of pregnancy loss at <12 weeks gestation, updated recommendations have been published as of September 2024.
The following are the updated recommendations from ACOG for patients who are less than 12 0/7 weeks gestation and undergoing abortion (managed with uterine aspiration or medication) or experiencing pregnancy loss (spontaneous or managed with aspiration or medication):
-ACOG recommends forgoing routine Rh testing and RhIg prophylaxis
-Rh testing and administration of RhIg can be considered on an individual basis with the help of shared-decision making regarding potential risks and benefits
These updated recommendations are based on recent studies that show a very low likelihood (although not entirely zero) of Rh alloimmunization associated with these populations. Many other Obstetric expert guidelines (such as those from the World Health Organization, Royal College of Obstetricians and Gynaecologists, and the Society of Family Planning) mirror these recommendations.
Summary: Consider shared decision-making regarding RhoGAM administration in patients who have an abortion or early pregnancy loss at <12 weeks gestation.
Rh D Immune Globulin Administration After Abortion or Pregnancy Loss at Less Than 12 Weeks of Gestation. Obstetrics & Gynecology ():10.1097/AOG.0000000000005733, September 10, 2024. | DOI: 10.1097/AOG.0000000000005733
Category: Pharmacology & Therapeutics
Keywords: Epinephrine, Allergic Reactions, Anaphylaxis (PubMed Search)
Posted: 10/10/2024 by Matthew Poremba
(Updated: 2/2/2026)
Click here to contact Matthew Poremba
Background:
Epinephrine administration is a critical component of treating severe allergic reactions, and delayed administration is associated with increased morbidity and mortality. Epinephrine auto-injectors are the current standard of care and allow for rapid administration in all care settings, but compliance issues can limit their use. The most common reason patient’s site for failure to administer or delayed administration of auto-injectors is needle phobia (particularly with pediatric patients). This has led to interest in developing needle-free epinephrine delivery devices that are easy to administer.
New Drug Approval:
This August, the FDA approved an epinephrine nasal spray (brand name: Neffy) for use as emergency treatment for Type 1 allergic reactions, including life-threatening anaphylaxis. The approval was based on four studies, including 175 total patients, comparing epinephrine 2 mg nasal spray with an epinephrine 0.3 mg intramuscular injection in healthy adults and children. These studies showed similar blood concentrations of epinephrine between treatment arms through 60 minutes after administration. In addition, both treatment arms showed similar elevations in heart rate and systolic blood pressure.
Bottom Line:
Epinephrine nasal spray is a newly approved option for the treatment of severe allergic reactions and anaphylaxis. While this approval was based on studies in healthy adults and children who did not currently have anaphylaxis, this medication may be worth considering for patients who have issues or concerns about using an injectable device to administer epinephrine.
Category: Critical Care
Keywords: Septic Shock, Vitamin B12, Hydroxocobalamin, sepsis (PubMed Search)
Posted: 10/8/2024 by Jordan Parker, MD
Click here to contact Jordan Parker, MD
Background:
Septic shock is a severe and common critical illness that is managed in the emergency department. Our current foundation of treatment includes IV fluids, empiric antibiotic coverage, vasopressor therapy, source control and corticosteroids for refractory shock. The levels of nitric oxide (NO) and hydrogen sulfide (H2S) are elevated in sepsis and associated with worse outcomes. Hydroxocobalamin is an inhibitor of NO activity and production and a scavenger of H2S [1,2]. Most of the current data is limited to observational studies looking at hydroxocobalamin in cardiac surgery related vasodilatory shock with few case series and reports for use in septic shock. The available data has shown an improvement in hemodynamics and reduction in vasopressor requirements in various vasodilatory shock states [2]. Chromaturia and self-limited red skin discoloration are common side effects but current data has not shown significant adverse events [3,4]. Patel et al, performed a phase 2 single-center trial to evaluate use of high dose IV hydroxocobalamin in patients with septic shock.
Study:
Results
Take home
There is a low risk of serious adverse events from high dose hydroxocobalamin use [3,4]. For now, it may be reasonable to consider in cases of septic shock refractory to standard care but there isn’t enough data to support its regular use yet.
Category: Trauma
Keywords: chest tube, hemothorax, pigtail (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/7/2024)
Click here to contact Robert Flint, MD
The authors reviewed the literature surrounding use of pigtail catheters for traumatic hemothorax and found:
“these data support using percutaneous thoracostomy as a safe and reliable treatment option for hemodynamically stable adult patients with traumatic hemothorax and are backed by major trauma society guidelines including the Eastern Society for the Surgery of Trauma and the Western Trauma Association.1,3 It has the added benefit of the insertion being less painful with the understanding that the percutaneous thoracostomy can always be upsized to a thoracostomy tube.”
Owodunni, Oluwafemi P.Moore, Sarah A.Hynes, Allyson M. et al.
Annals of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: Pigtail (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/6/2024)
Click here to contact Robert Flint, MD
Emergency Medicine Cases offers these excellent tips on pigtail catheters placement. Their video/website is worth a look.
PEARL # 1 – LOCATION/LANDMARK: Minimize skin to pleural distance.
PEARL # 2 – ADEQUATE LOCAL ANESTHESIA: This can obviate the need for sedation.
PEARL #3 – DILATING: Do it in a controlled manner.
PEARL #4 – USING THE OBTURATOR: Needless to say, it is there for a reason.
PEARL #5 – INTERPLEURAL BLOCK: Provide your patient with ongoing analgesia.
PEARL #6 – STOPCOCK AND ONE-WAY VALVE IN THE CORRECT POSITIONS
PEARL #7 – USE A GOOD SUTURE: Don’t let that chest tube come out.
Category: Trauma
Keywords: EMS, c-spine, clearance, (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/5/2024)
Click here to contact Robert Flint, MD
This Canadian study looked at the safety of paramedics using the modified Canadian C-Spine Rule to determine which pre-hospital blunt trauma patients required immobilization. These were MVC and fall patients predominately. Bottom line: appropriately trained paramedics can use the modified Canadian C-Spine rule to clinically clear cervical spines in the field.

| Result of Application | Paramedics’ Interpretation | Investigators’ Interpretation |
|---|---|---|
| Injury | No Injury | Injury |
| --- | --- | --- |
| Immobilization required (N) | 10 | 1,342 |
| Immobilization not required (N) | 1 | 2,668 |
| Sensitivity, % (95% CI) | 90.9 (58.7–99.8) | 90.9 (58.7 to 99.8) |
| Specificity, % (95% CI) | 66.5 (65.1–68.0) | 68.2 (66.7 to 69.7) |
| Positive likelihood ratio, (95% CI) | 2.7 (2.2–3.4) | 2.9 (2.4 to 3.5) |
| Negative likelihood ratio (95% CI) | 0.1 (0.0–0.9) | 0.1 (0.0–0.9) |
Vaillancourt, Christian et al.
Annals of Emergency Medicine, Volume 81, Issue 2, 187 - 196
Category: EMS
Keywords: Cardiac arrest, Sodium Bicarbonate, EMS, Tricyclic Antidepressant (PubMed Search)
Posted: 10/4/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
Background:
Despite a lack of reliable evidence, sodium bicarbonate (SB) still appears in various protocols as a potential therapy for patients in cardiac arrest. Local EMS protocols also endorse the use of (SB) in specific scenarios such as: tricyclic overdose and hyperkalemia. EMS systems struggle to articulate best practices with respect to indications for SB administration.
Patients/methods:
Study authors conducted a scoping review of existing literature. The review included in hospital and out of hospital patients with cardiac arrest. Despite multiple studies looking at this question, a total of 12 were included in the final analysis. Criteria for inclusion were as follows: RCT or observational studies looking at patients aged 18 or older who experienced a cardiac arrest. Important outcome metrics incorporated: neurological recovery and survival to discharge.
Results:
The retrospective review failed to demonstrate a reliable association between survival and administration of sodium bicarbonate. Despite significant limitations (different study populations, retrospective designs), there remains insufficient evidence to consider routine administration of bicarb in the setting of cardiac arrest.
Bottom line:
Empiric administration of SB is not linked to a reliable benefit. SB may be considered for specific indications (tricyclic overdose, hyperkalemia) but is unlikely to improve outcomes such as neurologic recovery or hospital discharge. EMS systems should avoid recommending routine SB administration for patients with out of hospital cardiac arrest.
Batarda Sena PM, Rodrigues J, Das Neves Coelho F, Soares Nunes B, Fernandes O, Fernandes N, Nóbrega JJ. Sodium Bicarbonate In In-Hospital and Out-of-Hospital Cardiac Arrest: A Systematic Literature Review. Cureus. 2024 Aug 30;16(8):e68192. doi: 10.7759/cureus.68192. PMID: 39347297; PMCID: PMC11439239.
Category: Critical Care
Keywords: albumin, crystalloid, septic shock, mortality (PubMed Search)
Posted: 10/1/2024 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Title: Albumin Versus Balanced Crystalloid for the Early Resuscitation of Sepsis: An Open Parallel-Group Randomized Feasibility Trial— The ABC-Sepsis Trial
Settings: 15 ED in the United Kingdom. This study is a feasibility study but it looked at mortality as a primary outcome.
Participants:
• Patients with Sepsis, with their National Early Warning Score (NEWS) ? 5 (These patients have estimated mortality of 20%). IV fluid resuscitation needs to be within 1 hour of assessment.
• 300 Patients were randomized to receive balanced crystalloids or 5% human albumin solution (HAS) only, within 6 hours of randomization.
Outcome measurement: 30-day mortality, Hospital length of stay (HLOS)
Study Results:
• The median time for receiving IV fluid from randomization was 41 minutes (HAS) vs. 36 minutes (crystalloids).
• Total volume of IV fluid per Kg in first 6 hours 14.5 ml/kg (HAS) vs. 18.8 ml/kg (crystalloids).
• Other interventions (vasopressor, Renal replacement therapy, invasive ventilation) were similar.
• Complications (AKI, pulmonary edema, allergy) were lower for Crystalloids group
• Median hospital LOS = 6 days for both groups.
• 90-day mortality: 31 (21.1%) (HAS) vs. 22 (14.8%) (Crystalloids), OR 1.54 (95% 0.8-2.8)
Discussion:
• Total volumes for resuscitation in the first 6 hours was 750 ml (HAS) and 1250 ml (crystalloids). This signified a trend toward lower total volume of resuscitation (remember that 30 ml/kg recommendation)
• The 2024 guidelines from Chest (REF 2) suggested that: “In Critically ill adult patients (excluding patients with thermal injuries and ARDS), intravenous albumin is not suggested for first line volume replacement or to increase serum albumin levels. Therefore, we should not give patients (except for cirrhosis or spontaneous bacterial peritonitis) albumin just to reduce the volume of fluid.
• The authors suggested that even a definitive trial in the future will not be able to demonstrate a significant benefit of using 5% albumin.
Conclusion:
There is lower mortality (numerical but not statistically) among the group with balanced crystalloids.
1. Gray AJ, Oatey K, Grahamslaw J, Irvine S, Cafferkey J, Kennel T, Norrie J, Walsh T, Lone N, Horner D, Appelboam A, Hall P, Skipworth RJE, Bell D, Rooney K, Shankar-Hari M, Corfield AR; Albumin, Balanced, and Crystalloid-Sepsis (ABC-Sepsis) Investigators. Albumin Versus Balanced Crystalloid for the Early Resuscitation of Sepsis: An Open Parallel-Group Randomized Feasibility Trial- The ABC-Sepsis Trial. Crit Care Med. 2024 Oct 1;52(10):1520-1532. doi: 10.1097/CCM.0000000000006348. Epub 2024 Jun 24. PMID: 38912884.
2. Callum J, Skubas NJ, Bathla A, Keshavarz H, Clark EG, Rochwerg B, Fergusson D, Arbous S, Bauer SR, China L, Fung M, Jug R, Neill M, Paine C, Pavenski K, Shah PS, Robinson S, Shan H, Szczepiorkowski ZM, Thevenot T, Wu B, Stanworth S, Shehata N; International Collaboration for Transfusion Medicine Guidelines Intravenous Albumin Guideline Group. Use of Intravenous Albumin: A Guideline From the International Collaboration for Transfusion Medicine Guidelines. Chest. 2024 Aug;166(2):321-338. doi: 10.1016/j.chest.2024.02.049. Epub 2024 Mar 4. PMID: 38447639; PMCID: PMC11317816.
Category: Ultrasound
Keywords: POCUS; FAST exam (PubMed Search)
Posted: 9/30/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
The Lipliner Sign is causing a lot of buzz within the ultrasound community, particularly concerning its implications for focused assessment with sonography for trauma (FAST) exams. This artifact arises from postprocessing techniques that enhance organ visualization but can inadvertently create a hypoechoic line that resembles free fluid leading to false positive exams.
Key points to note:
Nature of the Artifact: The Lipliner Sign manifests as a linear, hypoechoic outline around an organ, misleading clinicians into thinking there's free fluid present.
Differentiation: As mentioned in this case report, free fluid typically appears wedge-shaped and tapers as it moves into dependent areas, while the Lipliner Sign is more linear and closely follows the organ's contour.
Manufacturer Variability: This artifact can be observed across different ultrasound machine manufacturers.
Clinical Implications: Misinterpretation of the Lipliner Sign could lead to unnecessary interventions or misdiagnoses in trauma settings, underscoring the importance of thorough training and awareness of potential artifacts.
Category: Trauma
Keywords: Fall, EMS, injury prevention (PubMed Search)
Posted: 9/30/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This meta analysis looked for studies involving community EMS (CEMS) interventions trying to reduce falls. The authors found:
“CEMS fall prevention interventions reduced all-cause and fall-related emergency department encounters, subsequent falls and EMS calls for lift assist. These interventions also improved patient health-related quality of life, independence with activities of daily living, and secondary health outcomes.”
Further, prospective work needs to be done to look at this on a larger scale. We know falls in elderly patients lead to significant morbidity and mortality. This could be one way to improve fall mortality.
Friend TH, Thomas HM, Ordoobadi AJ_, et al_
Community emergency medical services approaches to fall prevention: a systematic review
Injury Prevention Published Online First:22 July 2024. doi: 10.1136/ip-2023-045110
Category: Orthopedics
Posted: 9/28/2024 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
A northeast university was recently in the news when several members of the lacrosse team were hospitalized with rhabdomyolysis. 9 of 50 players who participated in the workout required hospitalization. This occurred after a single intense 45-minute workout led by an alum and recent graduate of the Navy Seal training program.
It was surprising to many that young, fit, athletes would be so affected from a single workout.
Nontraumatic exertional rhabdomyolysis occurs following intense physical activity especially in untrained individuals or those unaccustomed to the particular activity (for example a group of runners performing an intense HIIT workout).
Prolonged strenuous activity can result in rhabdomyolysis even in trained individuals in the absence of known risk factors or prior history.
Increased risk when natural cooling mechanisms are affected such as when the individual is taking medications with anticholinergic properties, or the individual is wearing heavy military gear or football equipment.
Increased risk with sickle cell trait.
Increased risk when that activity is performed in environments of severe heat and humidity.
Exercise routines that have a heavy eccentric focus increases risk of rhabdomyolysis.
An Eccentric exercise involves slow lengthening of muscles under load
Examples: the lowering phase of a barbell while performing a bench press or the downward phase of a pull up
Helpful kinetics:
Following the exertional event, the serum CK will rise within 2-12 hours, reaching its maximum in 1-3 days.
CK has a serum half-life of approximately 36 hours.
CK levels decrease at approximately 40% per day.
Category: Administration
Keywords: design, workspace, handoff, interruptions, collaboration (PubMed Search)
Posted: 9/21/2024 by Mercedes Torres, MD
(Updated: 9/25/2024)
Click here to contact Mercedes Torres, MD
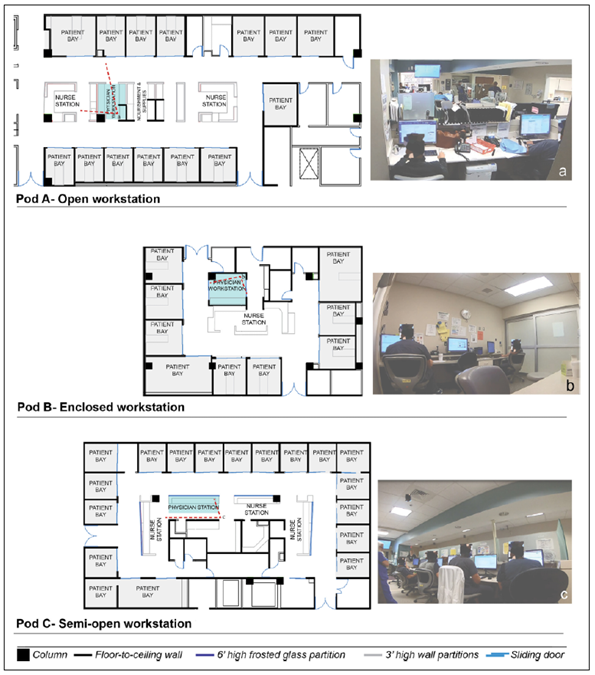
Joshi R, Joseph A, Ossmann M, et al. Emergency Physicians’ Workstation Design: An Observational Study of Interruptions and Perception of Collaboration During Shift-End Handoffs. HERD: Health Environments Research & Design Journal. 2021;14(4):174-193. doi:10.1177/19375867211001379
Category: Critical Care
Posted: 9/24/2024 by Caleb Chan, MD
(Updated: 2/2/2026)
Click here to contact Caleb Chan, MD
Some points from this narrative review:
Take home pearls:
van Eijk JA, Doeleman LC, Loer SA, Koster RW, van Schuppen H, Schober P. Ventilation during cardiopulmonary resuscitation: A narrative review. Resuscitation. 2024;203:110366.
Category: Hematology/Oncology
Posted: 9/24/2024 by Sarah Dubbs, MD
(Updated: 2/2/2026)
Click here to contact Sarah Dubbs, MD
The FDA approved two cell-based gene therapies for the treatment of Sickle Cell Disease in December, 2023. These therapies show potential to dramatically improve the outcomes and quality of life for patients with SCD. You may soon encounter patients who received one of these treatments in the ER, so here is an intro to what they are:
Casgevy is an FDA-approved gene therapy for sickle cell disease in patients 12 and older with recurrent vaso-occlusive crises. It uses CRISPR/Cas9 genome editing to modify blood stem cells, increasing fetal hemoglobin (HbF) production, which prevents red blood cell sickling.
Lyfgenia, also a gene therapy for sickle cell disease, uses a lentiviral vector to modify stem cells to produce HbAT87Q, a hemoglobin that reduces sickling. Both therapies involve modifying the patient's own stem cells, followed by myeloablative chemotherapy, and are given as a single infusion.
Long-term safety and effectiveness is still being studied. More to come in the future!
Frangoul H, Altshuler D, Cappellini MD, Chen YS, Domm J, Eustace BK, Foell J, de la Fuente J, Grupp S, Handgretinger R, Ho TW, Kattamis A, Kernytsky A, Lekstrom-Himes J, Li AM, Locatelli F, Mapara MY, de Montalembert M, Rondelli D, Sharma A, Sheth S, Soni S, Steinberg MH, Wall D, Yen A, Corbacioglu S. CRISPR-Cas9 Gene Editing for Sickle Cell Disease and ?-Thalassemia. N Engl J Med. 2021 Jan 21;384(3):252-260. doi: 10.1056/NEJMoa2031054. Epub 2020 Dec 5. PMID: 33283989. https://www.nejm.org/doi/10.1056/NEJMoa2031054?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
Interesting read from NPR featuring the first patient to receive this therapy:
Category: Geriatrics
Keywords: Geriatric fever score (PubMed Search)
Posted: 9/22/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study attempts to validate the use of the Geriatric Fever Score to predict 30 day mortality in patients over age 65 presenting to an emergency department with fever.
The Geriatric Fever Score uses: leukocytosis, severe coma, and thrombocytopenia. One point is award for each abnormality.
Not surprisingly, mortality went up with the higher the score (33%, 42% and 57% for 0,1,2 points)
For me, I’m not discharging anyone with severe coma, leukocytosis or thrombocytopenia in this patient population therefore I’m not sure this scale has much utility for the practicing emergency physician.
Akbari, H., Mirfazaelian, H., Safaei, A. _et al._Predicting mortality in geriatric patients with fever in the emergency departments: a prospective validation study. BMC Geriatr 24, 758 (2024). https://doi.org/10.1186/s12877-024-05346-x
