Category: Pulmonary
Keywords: pulmonary embolism, intervention, scoring, out come (PubMed Search)
Posted: 7/18/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
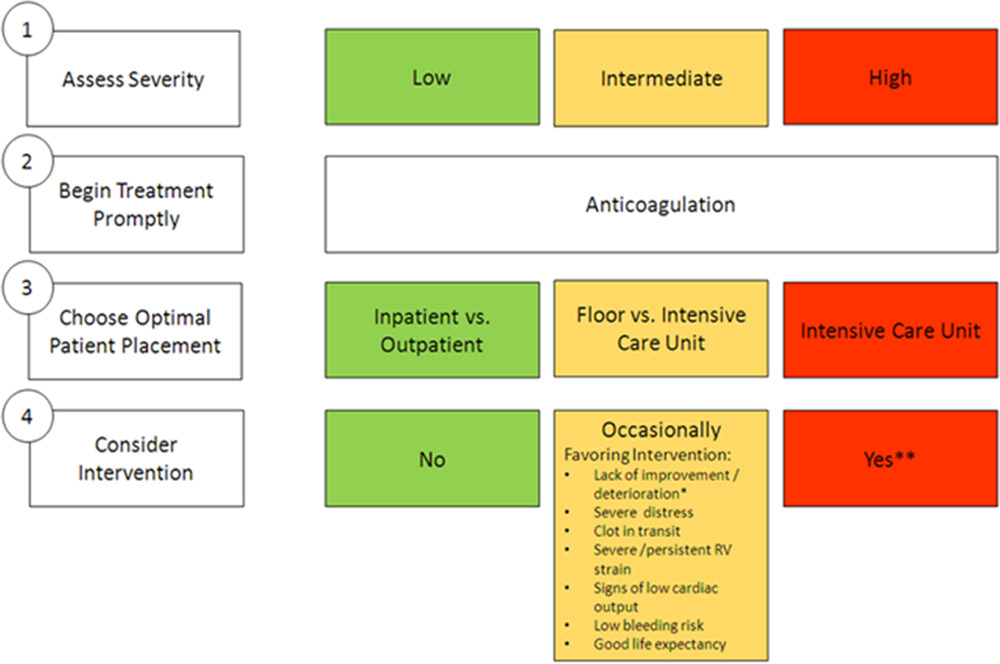
Deciding which pulmonary embolism patient needs thrombolytics/catheter based intervention is a shared decision among emergency physicians, intensivists, interventionalists, hospitalists, and the patient/family. This article provides evidence to help guide this decision. Keep in mind “The use of either CDL or catheter-based embolectomy in patients with intermediate-risk PE has, thus far, been correlated only with more rapid improvement of RV dysfunction than anticoagulation alone, not short- or long-term clinical or functional outcomes.”
"1. Massive (AHA) or high risk (ESC): Hypotension, defined as a systolic blood pressure <90 mm?Hg, a drop of >40 mm?Hg for at least 15 minutes (this latter criterion may be difficult to ascertain in some clinical circumstances), or need for vasopressor support, identifies these patients. They account for ?5% of hospitalized patients with PE and have an average mortality of ?30% within 1 month.
2.Submassive (AHA) or intermediate risk (ESC): RV strain without hypotension (see above) primarily identifies these patients. RV strain includes RV dysfunction on computed tomography pulmonary angiography or echocardiography (RV/left ventricular [LV] ratio >0.9)6,7 or RV injury and pressure overload detected by an increase in cardiac biomarkers such as troponins or brain natriuretic hormone.
3.Low risk (ESC and AHA): These patients do not meet criteria for submassive (AHA) or intermediate-risk (ESC) PE"
Interventional Therapies for Acute Pulmonary Embolism: Current Status and Principles for the Development of Novel Evidence: A Scientific Statement From the American Heart Association
Jay Giri, MD, MPH, FAHA, Chair, Akhilesh K. Sista, MD, FAHA, Vice Chair, Ido Weinberg, MD, MSc, Clive Kearon, MB, PhD, Dharam J. Kumbhani, MD, FAHA, Nimesh D. Desai, MD, PhD, Gregory Piazza, MD, MS, FAHA, Mark T. Gladwin, MD, FAHA, Saurav Chatterjee, MD, Taisei Kobayashi, MD, Christopher Kabrhel, MD, MPH, and Geoffrey D. Barnes, MD, MSc, FAHAAUTHOR INFO & AFFILIATIONS
Circulation
https://doi.org/10.1161/CIR.0000000000000707
