Category: Cardiology
Keywords: early repolarization, ST segment elevation, STEMI, ST elevation (PubMed Search)
Posted: 10/17/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
ECG early repolarization (or sometimes referred to as "benign early repolarization" or BER) is a common finding on ECGs, especially in young patients. It is a common "confounding" pattern when trying to identify STEMI. Here are some pearls that help in distinguishing BER vs. true STEMI. Remember at the outset, though, nothing in medicine is 100%....and that getting old ECGs or getting serial ECGs can be incredibly helpful.
1. BER is ONLY allowed to have STE that is concave upwards. If you ever see STE that is convex upwards (like a tombstone) or horizontal, it MUST be a STEMI.
2. BER should not have ST-segment depression, except maybe in aVR and V1. If there is ST depression in any of the other 10 leads, it is almost definitely a STEMI.
3. If you see STE in the inferior leads, compare the STE in lead II vs. lead III. If the STE in lead III is greater than the STE in lead II, it rules out BER....gotta be STEMI.
4. STE from BER is usually maximal in the mid precordial leads. You CAN have STE in the inferior leads with BER also, but you really shouldn't have STE isolated to the inferior leads. In other words, BER can have (1) STE in the precordial leads alone, or (2) STE in the precordial + inferior leads, but it should never have STE isolated to the inferior leads, and also the STE in the precordial leads should be more prominent than the STE in the inferior leads.
5. BER should usually not have STE > 5 mm. However, I've seen some occasional exceptions when the patient has large voltage QRS complexes.
Category: Cardiology
Keywords: oxygen, acute myocardial infarction (PubMed Search)
Posted: 10/3/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
The traditional teaching has always been to use supplemental high-flow oxygen routinely for patients with acute MI. I recall specifically being taught in residency by EM, IM, and cardiology attendings that every acute MI patient should receive a minimum of 6 liters of supplemental oxygen via nasal canula, if not 100% oxygen, regardless of the initial pulse oximetry.
Mounting evidence, however, is demonstrating that the use of supplemental oxygen in patients that are "normoxic" (i.e. the production of "hyperoxia") is detrimental. Studies are demonstrating that there is no improvement in mortality or prevention of dysrhythmias; and in fact a trend towards increased mortality when patients are hyperoxic. This detrimental effect is likely the result of coronary vasoconstriction which occurs through several different mechanisms, all induced by hyperoxia. Oxygen, it turns out, is a vasoactive substance.
The takeaway point is very simple: if an AMI patient is not hypoxic, don't go overboard with the supplemental oxygen!
[Moradkhan R, Sinoway LI. Revisiting the role of oxygen therapy in cardiac patients. J Am Coll Cardiol 2010;56:1013-1016.]
Category: Cardiology
Keywords: electrocardiography, posterior, myocardial infarction (PubMed Search)
Posted: 9/26/2010 by Amal Mattu, MD
(Updated: 10/3/2010)
Click here to contact Amal Mattu, MD
Approximately 4% of acute MIs will present as an isolated posterior MI (AKA "true posterior MI"). These are easily misdiagnosed as simply anterior ischemia because of the ECG findings. However, the distinction is critically important because posterior STEMI is now considered an indication for immediate reperfusion (PCI or lytics), whereas anterior ischemia is not.
The diagnosis of posterior STEMI is made by looking for:
1. ST segment depression, typically in leads V1-V3
2. upright T-waves in leads V1-V3
3. development of tall R-waves (R > S in amplitude) in V1-V3 over the course of a few hours (this is analogous to Q-waves forming in the posterior portion of the ventricle)
Early on, you may not be able to rely on the presence of tall R-waves to help you. Therefore, it's best to simply do the following: whenever you find ST-segment depression in leads V1-V3, always repeat the ECG using posterior leads (simply place a couple of the V leads on the left mid-back area). These leads will "look" directly at the posterior heart. If those leads show ST elevation, the diagnosis is posterior STEMI. If those leads don't show ST elevation, you can then make the diagnosis of simply anterior ischemia and hold off on immediate PCI or lytics.
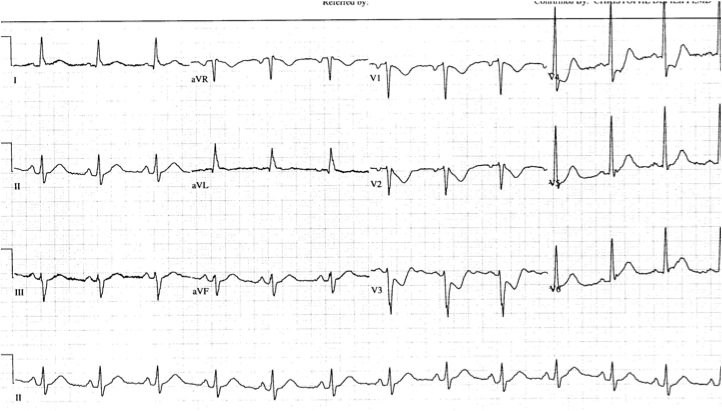
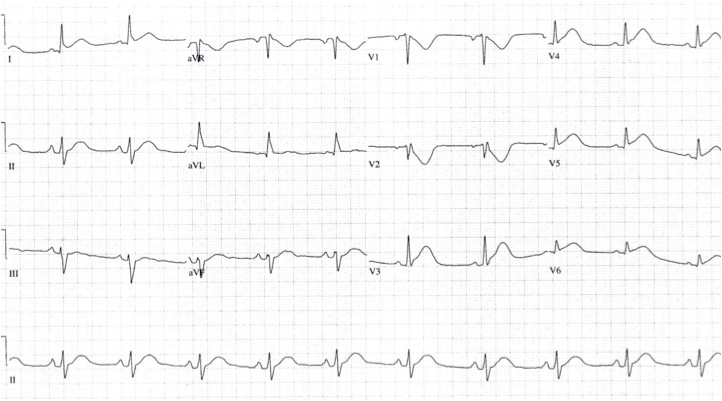
The first ECG below shows ST depression in the anteroseptal leads, suspicious for posterior STEMI. The ECG was then repeated, second ECG, with leads V3-V6 placed wrapping around to the left mid-back area. The ST elevation in these leads confirmed the presence of a posterior STEMI and justified immediate reperfusion therapy.
Category: Geriatrics
Keywords: erythrocyte sedimentation rate, sed rate, temporal arteritis (PubMed Search)
Posted: 9/19/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
There is a correction factor for erythrocyte sedimentation rate in the elderly. The top normal ESR in the elderly is (age + 10)/2. For example, an 80 yo patients would have a top normal ESR of (80+10)/2 = 45. Most laboratories do not, however, report this correction factor, but simply list < 20 (or thereabouts) as normal.
Be certain to take this correction factor into account when using ESRs for workups for temporal arteritis or other similar conditions.
Category: Cardiology
Keywords: syncope, arrhythmias, dysrhythmias (PubMed Search)
Posted: 9/12/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
17-18% of cases of syncope are attributable to arrhythmias
The greatest predictors of arrhythmias as the cause of syncope are:
a. Abnormal ECG (odds ratio 8.1)
b. History of CHF (odds ratio 5.3)
c. Age older than 65 (odds ratio 5.4)
[Sarasin, et al. Academic Emergency Medicine 2003]
Category: Cardiology
Keywords: cocaine, myocardial infarction, atherosclerosis (PubMed Search)
Posted: 9/5/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Acute use of cocaine increases risk of acute MI due to tachydysrhythmias, vasospasm, and increased platelet aggregation. There is a 24-fold increased risk of MI in the first hour after use of cocaine. 6% of patients presenting with cocaine-chest pain rule in for acute MI.
[Weber, Acad Emerg Med 2000]
Category: Cardiology
Keywords: SVT, atrial fibrillation, WPW, antidromic, orthodromic (PubMed Search)
Posted: 8/29/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Some confusion exists regarding proper distinction and treatment between the different tachydysrhythmias associated with WPW. Here's the scoop:
1. orthodromic SVT: narrow regular tachycardia, looks just like a routine SVT, treat just like any other SVT (AV nodal blockers work fine)
2. antidromic SVT: wide regular tachycardia, looks just like VTach, treat like VTach (amiodarone, procainamide, shock; lidocaine won't work, though won't harm either)
3. atrial fibrillation: very different!! irregularly irregular, morphologies of the QRS complexes vary between narrow and wide, some areas may have rates as high as 250-300/min, MUST avoid all AV nodal blockers (which includes adenosine, CCBs, BBs, digoxin, amiodarone); treat with procainamide or sedation+cardioversion
Category: Cardiology
Keywords: hypercalcemia, hypocalcemia, electrocardiography (PubMed Search)
Posted: 8/22/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
typical ECG findings associated with hypercalcemia: short QT (e.g. QTc < 400 msec), ST-segment depression
typical ECG findings associated with hypocalcemia: prolonged QT
note that hyperkalemia is often associated with hypocalcemia, and as a result hyperkalemic patients often have a prolonged QT, but it's not the hyperkalemia that prolongs the QT, it's the hypocalcemia
Category: Cardiology
Keywords: cardioversion, atrial fibrillation (PubMed Search)
Posted: 8/15/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Increasing literature is supportive of the idea of electrically cardioverting new-onset atrial fibrillation (onset < 48 hours). The traditional concerns are that (1) cardioversion doesn't work well with atrial fibrillation and that (2) you will induce an embolic event. The literature actually indicates that both of these concerns are not true. The success rate of electrically cardioverting new-onset atrial fibrillation is actually >90% and the risk of embolism is < 1% (Burton, Ann Emerg Med). Many EDs already utilize such protocols that recommend routine cardioversion for these patients and discharge after a brief observation period.
In coming years, fueled by issues pertaining to hospital overcrowding and cost containment, we'll all be seeing more and more papers and guidelines recommending early electrical cardioversion, so if you aren't comfortable with the idea....you will be!
Category: Cardiology
Keywords: ventricular, aneurysm, myocardial infarction, electocardiography, electrocardiogram (PubMed Search)
Posted: 8/8/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
The ECG distinction between ventricular aneurysm vs. true STEMI is a tough one. Aside from reviewing the patient's history, here are a few pearls that may help.
1. Both entities cause Q-waves and STE that can be concave or convex upwards. However, aneurysms shouldn't cause reciprocal depression, whereas a true STEMI often does.
2. Serial ECGs and old ECGs are helpful. The aneurysm shouldn't change from a recent ECG or with serial testing, but STEMI ECGs often do, even over the course of 1-2 hours. Look for any changes in ST segments, T-wave morphology changes, or development of Q-waves.
3. Aneurysms are almost always associated with STE in the anterior leads (because most aneurysms involve the anterior wall). STEMI can involve anterior, lateral, or inferior wall.
4. Aneurysms are almost always associated with Q-waves, whereas STEMI may not (yet) have Q-waves.
Category: Cardiology
Posted: 7/25/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Classic electrocardiographic findings for hypokalemia:
u-waves (produces appearance of long QT), especially in the precordial leads
ventricular ectopy (PVCs typically)
ST segment depression or downward sagging, especially in the precordial leads
note that the sagging ST segments that terminate in large U-waves end up producing biphasic T-waves; these have the mirror image appearance of Wellens waves
Category: Cardiology
Keywords: ST segment elevation, myocardial infarction (PubMed Search)
Posted: 7/18/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
There are multiple reasons for ST-segment elevation, the most important of which is acute myocardial infarction. However, because the treatment difference between MI vs. other more benign causes is so important, one should keep in mind the following factors that strongly point toward the diagnosis of MI:
1. the presence of ST-segment depression in any lead aside from aVR or V1
2. ST elevation that is horizontal or convex upwards (like a tombstone)
3. ST or T-wave morphologies that change over time with serial testing
4. ST changes compared to old ECGs
5. the development of Q-waves
6. ST elevation that follows coronary anatomy (e.g. limited to inferior leads, anterior leads, or lateral leads)
Category: Geriatrics
Keywords: infection, cellulitis, geriatric, elderly (PubMed Search)
Posted: 7/11/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Elderly patients are at higher risk for skin infections for numerous reasons:
1. Blunted immune system response of skin to infections.
2. Slower wound repair after 3rd decade.
3. More frequent exposure to infections, especially drug resistant infections, especially if the patient is frequently hospitalized or in nursing homes.
4. Frequent portals of entry for skin infections: indwelling tubes and lines, leg ulcers, fissures and maceration on feet and between toes.
A key takeaway point is to always check the skin thoroughly of your elderly patients when searching for infections, especially the feet and toes!
Category: Geriatrics
Keywords: tachypnea, pneumonia, elderly, geriatric (PubMed Search)
Posted: 7/4/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
The majority of "classic" symptoms and signs in elderly patients with pneumonia (fever, cough, sputum production, leukocytosis,chest pain) are unreliably present. However, tachypnea is one of the most reliable early findings in elderly patients with pneumonia, and in fact the same can be said about other serious bacterial illnesses in the elderly. The takeaway point here is simple: always count the respiratory rate in elderly patients (and don't trust those triage respiratory rates)!
Category: Geriatrics
Keywords: leukocytosis, WBC, fever, elderly, geriatric, infection (PubMed Search)
Posted: 6/27/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
The WBC count is not an accurate predictor of bacteremia in the elderly. 20-45% of elderly patients with proven bacteremia have a normal WBC on presentation.
[from Caterino JM, et al. Bacteremic elder emergency department patients: procalcitonin and white count. Acad Emerg Med 2004;11:393-396.]
Category: Geriatrics
Keywords: nitritie, infections, elderly, geriatric (PubMed Search)
Posted: 6/20/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
The nitrite test on urine dipstick is commonly used for diagnosis of UTI. However, the test is only reliable in those bacteria that convert nitrates to nitrites, which primarily includes enterobaceriaceae. However, elderly patients often develop UTIs with Staph saprophyticus, pseudomonas, and enterococcus, none of which produce positive nitrites on dipstick testing. The takeaway point here is very simply....don't assume you've excluded UTI (esp. in elderly populations) just because the nitrite test is negative.
reference: Anderson RS, Liang SY. Infections in the elderly. Critical Decisions in Emergency Medicine, April 2010.
Category: Cardiology
Keywords: pericardial effusion, tamponade (PubMed Search)
Posted: 6/13/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Pericardial tamponade is a physiological diagnosis, not an ECG diagnosis. At best, the ECG can suggest the presence of large pericardial effusions--look for the combination of low voltage, tachycardia, and electrical alternans.
Be aware, however, that electrical alternans is only present in < 1/3 of patients with large pericardial effusions. Although it is "classic" and always seems to show up on board exams, in the textbooks, and in lectures, electrical alternans in not a consistent finding in patients with large effusions or tamponade.
Category: Geriatrics
Keywords: geriatrics, elderly, appendicitis (PubMed Search)
Posted: 6/7/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Up to 25% of elderly patients with appendicitis are initially sent home from the ED, an indication of the high misdiagnosis rate for appendicitis in the elderly population. Why are elderly patients so often misdiagnosed when they have appendicitis? The answer is simple....they present very atypically.
Expect the atypical in elderly patients!
Category: Geriatrics
Keywords: fever, elderly, geriatrics (PubMed Search)
Posted: 5/30/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Fever is less common in infectious states in the elderly than in young patients. However, in contrast to younger patients, when an elderly patient does have a fever it is much more likely to be associated with a serious bacterial infection. It has been estimated that the source of fever in elderly ED patients is viral in only 5% of cases.
[from Hals G. Common diagnoses become difficult diagnoses when geriatric patients visit the emergency department, part I. Emergency Medicine Reports 2010;31(9):101-110.]
Category: Geriatrics
Keywords: fever, elderly, geriatric (PubMed Search)
Posted: 5/23/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Elderly patients have slightly lower body temperatures than younger adults, and as a result it has been suggested that "fever" be defined as anything > 99 degrees F. One study found that by lowering the definition to this number improved the sensitivity and specificity to 83% and 89%, respectively.
from Hals G. Common diagnoses become difficult diagnoses when geriatric patients visit the emergency department, part I. Emergency Medicine Reports 2010;31(9):101-110.
study referred to: Castle SC, et al. Fever response in elderly nursing home residents: are the older truly colder? J Am Geriatric Soc 1991;39:853-857.
