Category: Cardiology
Keywords: therapeutic hypothermia, hypothermia, hypokalemia, cardiac arrest (PubMed Search)
Posted: 1/2/2011 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Induced hypothermia is associated with a decline in serum potassium levels. The cold myocardium is already mildly predisposed to arrhythmias, and the combination of hypokalemia + hypothermia appears to increase the risk of polymorphic ventricular tachycardia. Two simple measures should be taken during post-arrest therapeutic hypothermia:
1. Correct hypokalemia before and during cooling.
2. Monitor the patient's potassium level and QT interval during cooling, and correct as needed.
Mirzoyev SA, McLeod CJ, Bunch TJ, et al. Hypokalemia during the cooling phase of therapeutic hypothermia and its impact on arrhythmogenesis. Resuscitation 2010;81:1632-1636.
Category: Cardiology
Keywords: isoproterenol, bradycardia, torsades de pointes (PubMed Search)
Posted: 12/26/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Isoproterenol is a non-selective beta-1 and beta-2 agonist. The beta-1 effect produces an increase in heart rate, and the beta-2 effect produces mild vasodilation. Two times to consider its use are the following:
1. For overdriving pacing in cases of intermittent torsades de pointes when magnesium is ineffective.
2. For intractable bradycardia, this is another option besides dopamine or epinephrine. Because of the vasodilation, isoproterenol might be preferred to these other drugs when the bradycardia is accompanied by severe hypertension or when vasoconstrictors are not desired.
The drug is not commonly used anymore but is effective in treating persistent bradycardia or for overdrive pacing in patients with intermittent torsades de pointes when magnesium is ineffective. Be wary, though, that the beta-2 effect produces vasodilation so there may be a mild reduction in blood pressure when the drug is used.
Category: Cardiology
Keywords: Procainamide, ventricular tachycardia, amiodarone (PubMed Search)
Posted: 12/19/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
The September 5 2006 issue of Circulation contained a guideline, based on collaboration between the American Heart Assn, the American College of Cardiology, and the European Society of Cardiology, indicating that procainamide was preferable to amiodarone for the treatment of stable monomorphic ventricular tachycardia.
The 2010 AHA Guidelines have now also listed procainamide as the preferred drug for stable monomorphic ventricular tachycardia, giving it a Class IIa ("probably helpful") rating vs. amiodarone which has a Class IIb ("possibly helpful") rating. [thanks to Dr. Mike Abraham for pointing this out]
Procainamide is also the safest drug for use in tachydysrhythmias when an accessory pathway (e.g. Wolff-Parkinson-White syndrome) is present.
The caveat is that neither procainamide nor amiodarone should be used in the presence of a prolonged QTc.
Acute care physicians should (re-)familiarize themselves with the use of procainamide, and emergency departments should maintain quick access to this drug to stay up-to-date with current national and international guidelines.
ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death — Executive Summary (many many authors) Circulation 2006;114:1088-1132.
Neumar RW, et al. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S729-767.
Category: Cardiology
Keywords: end tidal CO2 monitoring (PubMed Search)
Posted: 12/5/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
In order to minimize interruptions in compressions due to pulse checks, continuous end tidal CO2 (ETCO2) monitoring during compressions is recommended. Before spontaneous circulation returns, the ETCO2 is likely to be on the order of < 10 mmg Hg. At the moment spontaneous circulation returns, the ETCO2 is expected to abruptly increase to at least 35-40 mm Hg. Be wary, though, that the administration of sodium bicarbonate may transiently increase the ETCO2 even in the absence of return of spontaneous circulation (ROSC).
Use of ETCO2 in this manner allows one to assess the patient for ROSC without ever having to stop compressions for pulse checks.
Category: Cardiology
Keywords: pregnancy, cardiac arrest, compressions (PubMed Search)
Posted: 11/28/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
In the second half of pregancy, we've traditionally learned that the gravid uterus compresses the inferior vena cava and therefore decreases cardiac output when patient is in a supine position. Therefore, we've learned that patients in the second half of pregnancy the patient should be placed in a left lateral tilt position.
However, it is difficult to perform good quality chest compressions when the patient is in a titled position.
Therefore, the optimal position for chest compressions on the patient in cardiac arrest in the second half of pregnancy is to have the patient in a supine position; and have another rescuer manually deflect the uterus to the patient's left side. This provides optimal compressions + optimal venous return.
Category: Cardiology
Keywords: bradycardia, bradydysrhythmia, atropine, transplant (PubMed Search)
Posted: 11/21/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
We mentioned atropine's elimination from the cardiac arrest (asystole, PEA) protocols last week. Atropine (0.5 mg) is still indicated in unstable bradycardias that appear to be vagally-mediated, such as sinus bradycardia and Mobitz I bradycardia.
Beware, however, that atropine is not recommended in patients with transplanted hearts. These hearts lack vagal innervation, and in fact there's one small study suggesting that atropine may be associated with paradoxical slowing of the heart rate and worsening AV block. Go straight to pacing with these patients.
Neumar RW, Otto CW, Link MS, et al. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S729-S767.
Category: Cardiology
Keywords: atropine, cardiac arrest (PubMed Search)
Posted: 11/14/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
The new 2010 AHA Guidelines no longer recommend the use of atropine in caring for patients with cardiac arrest. While it may be useful in vagally-mediated bradycardias, the evidence does NOT support the use of atropine in patients with asystole or PEA; therefore, it has been removed from the cardiac arrest algorithm.
Category: Cardiology
Keywords: airway, ACLS, AHA (PubMed Search)
Posted: 11/7/2010 by Amal Mattu, MD
(Updated: 11/14/2010)
Click here to contact Amal Mattu, MD
The new 2010 AHA guidelines have provided greater focus on airway issues in patients suffering from cardiac arrest. Amongst the important areas of new emphasis are: (1) Cricoid pressure is no longer routinely recommended during intubation, and in fact it has been given a Class III rating ("harmful"); and (2) there is now a very strong push to use quantitative end-tidal CO2 monitoring (rather than just qualitative confirmation) of the airway after endotracheal intubation.
Category: Cardiology
Keywords: acute myocardial infarction, hyperglycemia (PubMed Search)
Posted: 10/31/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
In honor of Halloween and candy....
Hyperglycemia (> 140 mg/dl) at the time of admission is an independent risk factor for adverse outcomes and mortality both during the hospital stay and long-term in patients with acute MI. Hyperglycemia is associated with adverse platelet function, thrombolysis, and coagulation. Tight glucose control is recommended to begin as soon as possible after admission in patients with acute MI in order to optimize outcomes.
Zarich SW, Nesto RW. Implications and treatment of acute hyperglycemia in the setting of acute myocardial infarction. Circulation 2007;115:e436-e439.
Category: Cardiology
Keywords: long QT, torsade, torsades, torsade de pointe, magnesium (PubMed Search)
Posted: 10/24/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Magnesium is considered a mainstay of treatment of prolonged QT syndrome leading to torsade de pointe, including those cases caused by drugs. The exact mechanism of action is unknown, though it is thought to stabilize the myocardium. Interestingly, magnesium infusions will not necessarily change the heart rate or QT interval on ECG.
The dose is 2 g IV followed by an infusion (similar to treatment of eclampsia/preeclampsia). The bolus should be given slowly if the patient is relatively stable, but can be pushed over 1 minute in a patient with ongoing torsade that is not responding to electricity.
Charlton NP, Lawrence DT, Brady WJ, et al. Termination of drug-induced torsades de pointes with overdrive pacing. Am J Emerg Med 2010;28:95-102.
Category: Cardiology
Keywords: early repolarization, ST segment elevation, STEMI, ST elevation (PubMed Search)
Posted: 10/17/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
ECG early repolarization (or sometimes referred to as "benign early repolarization" or BER) is a common finding on ECGs, especially in young patients. It is a common "confounding" pattern when trying to identify STEMI. Here are some pearls that help in distinguishing BER vs. true STEMI. Remember at the outset, though, nothing in medicine is 100%....and that getting old ECGs or getting serial ECGs can be incredibly helpful.
1. BER is ONLY allowed to have STE that is concave upwards. If you ever see STE that is convex upwards (like a tombstone) or horizontal, it MUST be a STEMI.
2. BER should not have ST-segment depression, except maybe in aVR and V1. If there is ST depression in any of the other 10 leads, it is almost definitely a STEMI.
3. If you see STE in the inferior leads, compare the STE in lead II vs. lead III. If the STE in lead III is greater than the STE in lead II, it rules out BER....gotta be STEMI.
4. STE from BER is usually maximal in the mid precordial leads. You CAN have STE in the inferior leads with BER also, but you really shouldn't have STE isolated to the inferior leads. In other words, BER can have (1) STE in the precordial leads alone, or (2) STE in the precordial + inferior leads, but it should never have STE isolated to the inferior leads, and also the STE in the precordial leads should be more prominent than the STE in the inferior leads.
5. BER should usually not have STE > 5 mm. However, I've seen some occasional exceptions when the patient has large voltage QRS complexes.
Category: Cardiology
Keywords: oxygen, acute myocardial infarction (PubMed Search)
Posted: 10/3/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
The traditional teaching has always been to use supplemental high-flow oxygen routinely for patients with acute MI. I recall specifically being taught in residency by EM, IM, and cardiology attendings that every acute MI patient should receive a minimum of 6 liters of supplemental oxygen via nasal canula, if not 100% oxygen, regardless of the initial pulse oximetry.
Mounting evidence, however, is demonstrating that the use of supplemental oxygen in patients that are "normoxic" (i.e. the production of "hyperoxia") is detrimental. Studies are demonstrating that there is no improvement in mortality or prevention of dysrhythmias; and in fact a trend towards increased mortality when patients are hyperoxic. This detrimental effect is likely the result of coronary vasoconstriction which occurs through several different mechanisms, all induced by hyperoxia. Oxygen, it turns out, is a vasoactive substance.
The takeaway point is very simple: if an AMI patient is not hypoxic, don't go overboard with the supplemental oxygen!
[Moradkhan R, Sinoway LI. Revisiting the role of oxygen therapy in cardiac patients. J Am Coll Cardiol 2010;56:1013-1016.]
Category: Cardiology
Keywords: electrocardiography, posterior, myocardial infarction (PubMed Search)
Posted: 9/26/2010 by Amal Mattu, MD
(Updated: 10/3/2010)
Click here to contact Amal Mattu, MD
Approximately 4% of acute MIs will present as an isolated posterior MI (AKA "true posterior MI"). These are easily misdiagnosed as simply anterior ischemia because of the ECG findings. However, the distinction is critically important because posterior STEMI is now considered an indication for immediate reperfusion (PCI or lytics), whereas anterior ischemia is not.
The diagnosis of posterior STEMI is made by looking for:
1. ST segment depression, typically in leads V1-V3
2. upright T-waves in leads V1-V3
3. development of tall R-waves (R > S in amplitude) in V1-V3 over the course of a few hours (this is analogous to Q-waves forming in the posterior portion of the ventricle)
Early on, you may not be able to rely on the presence of tall R-waves to help you. Therefore, it's best to simply do the following: whenever you find ST-segment depression in leads V1-V3, always repeat the ECG using posterior leads (simply place a couple of the V leads on the left mid-back area). These leads will "look" directly at the posterior heart. If those leads show ST elevation, the diagnosis is posterior STEMI. If those leads don't show ST elevation, you can then make the diagnosis of simply anterior ischemia and hold off on immediate PCI or lytics.
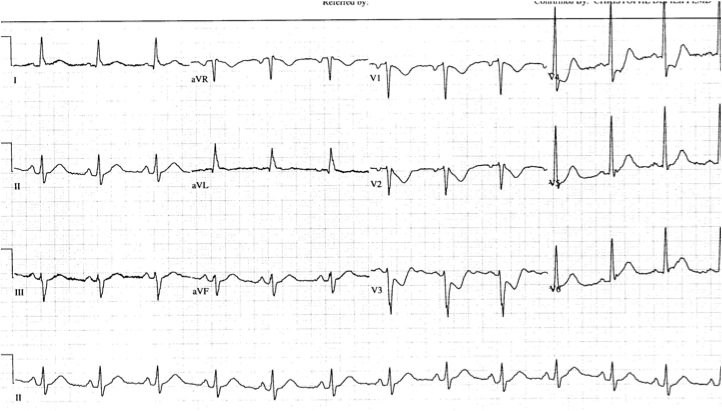
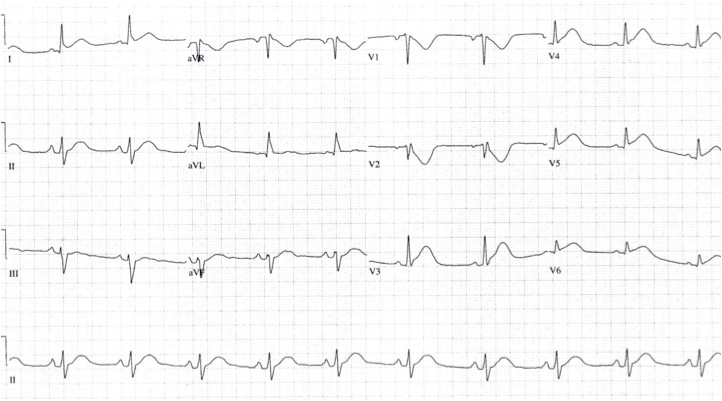
The first ECG below shows ST depression in the anteroseptal leads, suspicious for posterior STEMI. The ECG was then repeated, second ECG, with leads V3-V6 placed wrapping around to the left mid-back area. The ST elevation in these leads confirmed the presence of a posterior STEMI and justified immediate reperfusion therapy.
Category: Cardiology
Keywords: syncope, arrhythmias, dysrhythmias (PubMed Search)
Posted: 9/12/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
17-18% of cases of syncope are attributable to arrhythmias
The greatest predictors of arrhythmias as the cause of syncope are:
a. Abnormal ECG (odds ratio 8.1)
b. History of CHF (odds ratio 5.3)
c. Age older than 65 (odds ratio 5.4)
[Sarasin, et al. Academic Emergency Medicine 2003]
Category: Cardiology
Keywords: cocaine, myocardial infarction, atherosclerosis (PubMed Search)
Posted: 9/5/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Acute use of cocaine increases risk of acute MI due to tachydysrhythmias, vasospasm, and increased platelet aggregation. There is a 24-fold increased risk of MI in the first hour after use of cocaine. 6% of patients presenting with cocaine-chest pain rule in for acute MI.
[Weber, Acad Emerg Med 2000]
Category: Cardiology
Keywords: SVT, atrial fibrillation, WPW, antidromic, orthodromic (PubMed Search)
Posted: 8/29/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Some confusion exists regarding proper distinction and treatment between the different tachydysrhythmias associated with WPW. Here's the scoop:
1. orthodromic SVT: narrow regular tachycardia, looks just like a routine SVT, treat just like any other SVT (AV nodal blockers work fine)
2. antidromic SVT: wide regular tachycardia, looks just like VTach, treat like VTach (amiodarone, procainamide, shock; lidocaine won't work, though won't harm either)
3. atrial fibrillation: very different!! irregularly irregular, morphologies of the QRS complexes vary between narrow and wide, some areas may have rates as high as 250-300/min, MUST avoid all AV nodal blockers (which includes adenosine, CCBs, BBs, digoxin, amiodarone); treat with procainamide or sedation+cardioversion
Category: Cardiology
Keywords: hypercalcemia, hypocalcemia, electrocardiography (PubMed Search)
Posted: 8/22/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
typical ECG findings associated with hypercalcemia: short QT (e.g. QTc < 400 msec), ST-segment depression
typical ECG findings associated with hypocalcemia: prolonged QT
note that hyperkalemia is often associated with hypocalcemia, and as a result hyperkalemic patients often have a prolonged QT, but it's not the hyperkalemia that prolongs the QT, it's the hypocalcemia
Category: Cardiology
Keywords: cardioversion, atrial fibrillation (PubMed Search)
Posted: 8/15/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Increasing literature is supportive of the idea of electrically cardioverting new-onset atrial fibrillation (onset < 48 hours). The traditional concerns are that (1) cardioversion doesn't work well with atrial fibrillation and that (2) you will induce an embolic event. The literature actually indicates that both of these concerns are not true. The success rate of electrically cardioverting new-onset atrial fibrillation is actually >90% and the risk of embolism is < 1% (Burton, Ann Emerg Med). Many EDs already utilize such protocols that recommend routine cardioversion for these patients and discharge after a brief observation period.
In coming years, fueled by issues pertaining to hospital overcrowding and cost containment, we'll all be seeing more and more papers and guidelines recommending early electrical cardioversion, so if you aren't comfortable with the idea....you will be!
Category: Cardiology
Keywords: ventricular, aneurysm, myocardial infarction, electocardiography, electrocardiogram (PubMed Search)
Posted: 8/8/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
The ECG distinction between ventricular aneurysm vs. true STEMI is a tough one. Aside from reviewing the patient's history, here are a few pearls that may help.
1. Both entities cause Q-waves and STE that can be concave or convex upwards. However, aneurysms shouldn't cause reciprocal depression, whereas a true STEMI often does.
2. Serial ECGs and old ECGs are helpful. The aneurysm shouldn't change from a recent ECG or with serial testing, but STEMI ECGs often do, even over the course of 1-2 hours. Look for any changes in ST segments, T-wave morphology changes, or development of Q-waves.
3. Aneurysms are almost always associated with STE in the anterior leads (because most aneurysms involve the anterior wall). STEMI can involve anterior, lateral, or inferior wall.
4. Aneurysms are almost always associated with Q-waves, whereas STEMI may not (yet) have Q-waves.
Category: Cardiology
Posted: 7/25/2010 by Amal Mattu, MD
(Updated: 2/1/2026)
Click here to contact Amal Mattu, MD
Classic electrocardiographic findings for hypokalemia:
u-waves (produces appearance of long QT), especially in the precordial leads
ventricular ectopy (PVCs typically)
ST segment depression or downward sagging, especially in the precordial leads
note that the sagging ST segments that terminate in large U-waves end up producing biphasic T-waves; these have the mirror image appearance of Wellens waves
