Category: Geriatrics
Keywords: Tramadol, geriatrics (PubMed Search)
Posted: 1/29/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Tramadol has been viewed as a safer alternative for pain control than opioids. This study says differently.
“Tramadol use was associated with increased risk of multiple ER utilizations, falls/fractures, CVD hospitalizations, safety event hospitalizations, and mortality (new users only) compared to nonuse.”
Musich S, Wang SS, Schaeffer JA, Slindee L, Kraemer S, Yeh CS. Safety Events Associated with Tramadol Use Among Older Adults with Osteoarthritis. Popul Health Manag. 2021 Feb;24(1):122-132. doi: 10.1089/pop.2019.0220. Epub 2020
Category: Geriatrics
Keywords: Delerium, antihistamine, geriatrics (PubMed Search)
Posted: 1/18/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In 261 ED patients over age 65 receiving first generation antihistamines, 15% had an adverse reaction. Most common was delirium and urinary retention. Age over 85, previous cognitive impairment and multiple doses increased the risk of adverse reaction. Along with previous literature, this should discourage use of first generation antihistamines in older ED patients.
Killen, E., Cusumano, M., Zhang, Z., Newman, R., Voigtmann, J., Sanford, A. M, & Bitter, C. C. (2025). First-Generation Antihistamine Use in Geriatric Emergency Department Patients: Retrospective Review. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 27(1). http://dx.doi.org/10.5811/westjem.47491 Retrieved from https://escholarship.org/uc/item/7230n5z1
Category: Geriatrics
Keywords: FRAIL, geriatric, prediction tool, Barthel (PubMed Search)
Posted: 1/1/2026 by Robert Flint, MD
(Updated: 1/3/2026)
Click here to contact Robert Flint, MD
The Geriatric Measurement Tool (GMT) was used in this study prospectively to assess 24 hour mortality rate in ED patients over age 65. The GMT is a combination of FRAIL Questionnaire and Barthel index for Activity of Daily Living. The study found:
“ From 700 enrolled patients, GMT categorization revealed that 53.6% of patients were in Category-4 (moderate/more dependent and frail), while 34% were in Category-1 (independent or slight dependency, prefrail/fit). The 24-h mortality rate was 9%. GMT Category-4 demonstrated high sensitivity (87.3%) for mortality prediction, but low specificity (49.7%). Conversely, GMT Category-1 showed low sensitivity (44.1%) but high specificity (90.2%) for predicting discharge.”
Probably the biggest take away is we should be thinking about assessing our older patient's health status using some validated scale/tool to help us have conversations with patients and families regarding prognosis and interventions.
Category: Geriatrics
Keywords: FRAIL, geriatric, prediction tool, mortality, (PubMed Search)
Posted: 1/1/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
The Geriatric Measurement Tool combines the FRAIL Questionnaire with the Barthel Index For Daily Living to give a prognosis on your patient's mortality. First used to predict mortality in older patients with pneumonia during COVID-19 pandemic. Now being investigated for other ED patient populations.
FRAIL Questionnaire: Fatigue, Resistance, Aerobic, Illness, Weight loss. https://www.activeagingweek.com/pdf/abbott/FRAILQuestionnaire.pdf
Barthel: Ten questions about ADL's to create a score 0-100. https://www.mdcalc.com/calc/3912/barthel-index-activities-daily-living-adl
Zaman, Süeda et al. Journal of Emergency Medicine, Volume 79, 560 - 567
2. Gómez-Moreno, C., Chacón-Corral, A.A., Pérez-Méndez, A. et al. Association between a geriatric measure tool and adverse outcomes among older adults treated in an emergency department: a retrospective cohort study. Intern Emerg Med 20, 2205–2213 (2025). https://doi.org/10.1007/s11739-024-03843-w
Category: Geriatrics
Keywords: delirium, hip fracture, nerve block (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study is a reminder of the efficacy of regional nerve blocks for older patient's with hip fractures. The authors trained EM physicians for 2 hours then evaluated delirium levels in patients who did and did not receive nerve blocks for hip fractures.
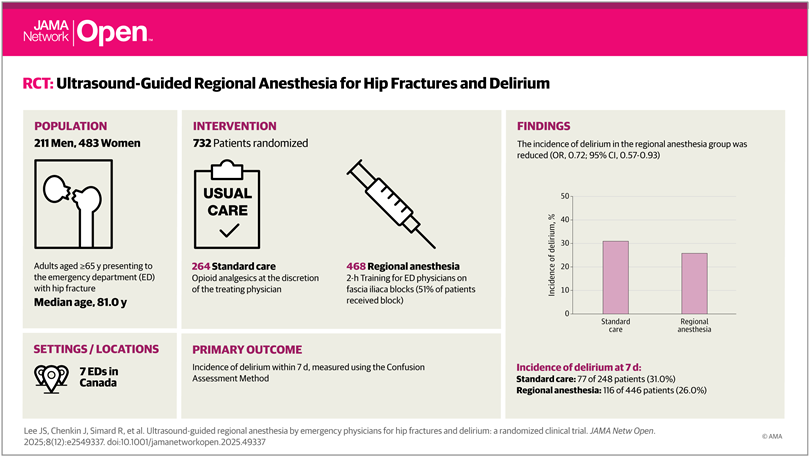
Lee JS, Chenkin J, Simard R, et al. Ultrasound-Guided Regional Anesthesia by Emergency Physicians for Hip Fractures and Delirium: A Randomized Clinical Trial. JAMA Netw Open. 2025;8(12):e2549337. doi:10.1001/jamanetworkopen.2025.49337
Category: Geriatrics
Keywords: frail, frailty scale, geriatrics, critical care (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/27/2025)
Click here to contact Robert Flint, MD
A prospective cohort of South Korean patients over 65 years admitted from the ED with critical illness had Clinical Frailty Scale (CFS) performed on them. Those with a high CFS had increased 3 month mortality. CFS helps us prognosticate morbidity and mortality in our older critically ill patients.
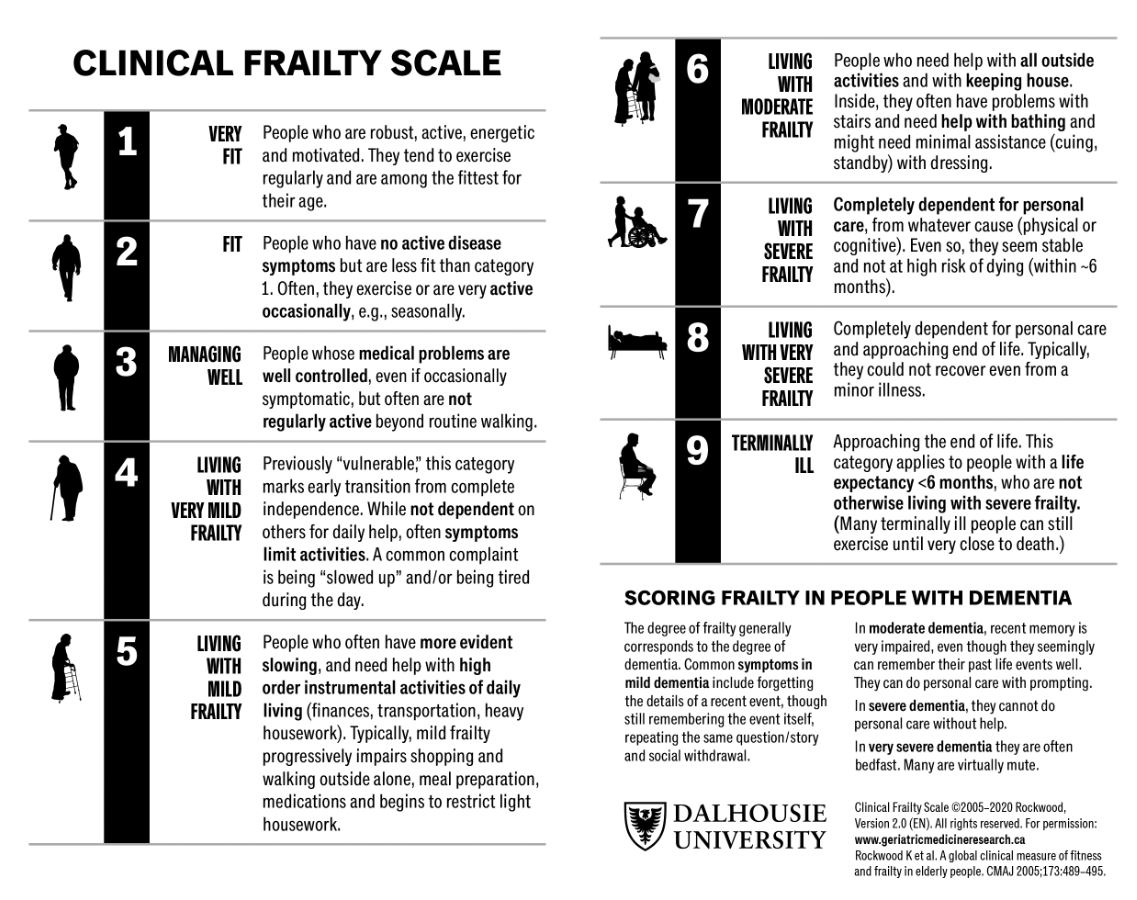
Um, Young Woo et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Geriatrics
Keywords: hip fracture, nerve block, mortality, delerium (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/20/2025)
Click here to contact Robert Flint, MD
In reviewing the limited literature available, the authors found that fascia iliaca blocks did not improve mortality but did improve hospital length of stay, decreased opiate use, and decreased delirium rates. More research is needed, however this tool should be added to our multimodal pain control toolbox.
Finch, Alexander S. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Geriatrics
Keywords: cardiac arrest, older, epinephrine (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/29/2025)
Click here to contact Robert Flint, MD
These authors looked at survival to discharge pre and post-implementation of a single dose epinephrine protocol for out of hospital cardiac arrest as it relates to age ranges. They found that older patients had a survival rate of 12% in the single dose protocol compared to 6% in the multidose protocol. Younger and middle aged patients had no difference in survival pre and post-implementation. At least in older adults, epinephrine does not seem to offer much benefit when given more than one time during cardiac arrest.
Single Dose Epinephrine Protocol Is Associated With Improved Survival of Older Adults With Out-Of-Hospital Cardiac Arrest
Ethan J. Lilien, Nicklaus P. Ashburn, Tyler S. George, Anna C. Snavely, Bryan P. Beaver, Casey G. Costa, Michael A. Chado, Harris A. Cannon, James E. Winslow, R. Darrell Nelson … See all authors
First published: 25 September 2025 Academic Emergency Medicine
Category: Geriatrics
Keywords: RSV, geriatric, heart failure, morbidity (PubMed Search)
Posted: 10/19/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This study looked at older patients admitted to the hospital with a diagnosis of one of the following: RSV infection, UTI, influenza, fracture. Those patients with RSV had longer stays, higher mortality, higher ICU length of stay and interestingly more cardiovascular complications up to one year after hospitalization. Further evidence we should be testing for RSV in our ill older patients and encouraging vaccination.
Category: Geriatrics
Keywords: fall, score, geriatric, prediction (PubMed Search)
Posted: 10/11/2025 by Robert Flint, MD
(Updated: 10/12/2025)
Click here to contact Robert Flint, MD
These authors used information available from both the medical record as well as from a survey instrument given in the emergency department to created this fall risk score. A score over 6 had a 63% sensitivity and 75% specificity of predicting future falls.
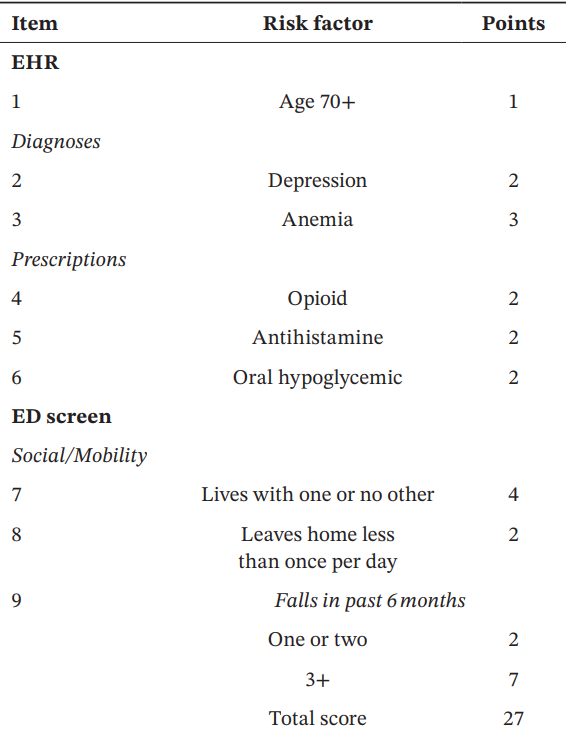

Acaemic Emergency Medicine 2025 0:1-12
Category: Geriatrics
Keywords: trauma, geriatric, prehospital, EMS (PubMed Search)
Posted: 10/4/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Reenforcing the recent pearl on geriatric trauma patient care, here is the National Association EMS Physicians statement on prehospital care.
"EMS clinicians should use age-adjusted, physiologic criteria to guide decisions to transport geriatric trauma patients to the most appropriate level of trauma center available in the community.
Geriatric trauma patients should be promptly evaluated for pain and should receive analgesic interventions in a timely manner. Analgesic medications should be dosed following weight-based guidance and should be administered with consideration of potential drug interactions and age-related changes in drug metabolism and side effects.
EMS clinicians should consult advance care planning documents, e.g., Physician Orders for Life-Sustaining Treatment (POLST), when available, to guide care in emergency scenarios, including management of traumatic injuries.
While older patients are at higher risk for spinal injuries, including lumbar and cervical spine fractures, traditional spinal motion restriction practices may not be suitable for older patients due to age-related anatomic changes in spinal alignment and increased risk for cutaneous pressure-related injuries. EMS clinicians should exercise judgment to determine when and how to best achieve spinal motion restriction if spinal injury is suspected in geriatric trauma patients."
Haussner, W. K., Breyre, A. M., Bascombe, K., Barrett, W. J., Camacho, M. A., Overton-Harris, P., … Colwell, C. (2025). Prehospital Trauma Compendium: Management of Geriatric Trauma Patients – A Position Statement and Resource Document of NAEMSP. Prehospital Emergency Care, 1–10. https://doi.org/10.1080/10903127.2025.2557006
Category: Geriatrics
Keywords: geriatrics, frail, diverticulitis (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 10/1/2025)
Click here to contact Robert Flint, MD
This retrospective study looking at a readmission database for patients greater than 65 years categorized 10,000 patients into non-frail, pre-frail and frail based on the five-factor modified frailty index. They found no difference in recurrent diverticulitis among the groups but did find:
“frailty was a predictor of mortality on index hospitalization (adjusted odds ratio, 1.99; p < 0.001) and readmissions (adjusted odds ratio, 3.05; p < 0.001)…frail patients are at increased risk of mortality once they develop diverticulitis. Optimal management for frail patients with diverticulitis must be defined to improve outcomes.”
Once again, assessing your patient's frailty can help you predict outcomes and have meaningful discussions with patients and their families.
Hejazi, Omar MD; Colosimo, Christina DO, MS, FACS; Khurshid, Muhammad Haris MD; Stewart, Collin MD, FACS; Al Ma'ani, Mohammad MD; Anand, Tanya MD, MPH, FACS; Castillo Diaz, Francisco MD; Castanon, Lourdes MD, FACS; Magnotti, Louis J. MD, MS, FACS; Joseph, Bellal MD, FACS. Does frailty predict readmission and mortality in diverticulitis? A nationwide analysis. Journal of Trauma and Acute Care Surgery 99(4):p 605-610, October 2025. | DOI: 10.1097/TA.0000000000004707
Category: Geriatrics
Keywords: frailty, geriatrics, troponin, syndrome (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 8/27/2025)
Click here to contact Robert Flint, MD
This editorial reminds us about the use of frailty measures in the geriatric population.
The authors write that frailty “describes a state of vulnerability causing an impaired ability to maintain homeostasis due to reduced physiologic reserve. Frailty is associated with disability, multimorbidity, cognitive impairment, institutionalization, and mortality. **Analogous to troponin testing, frailty assessment has been used to risk stratify older adults.**”
They also remind us that frailty is a syndrome not a disease in and of itself. It impacts how disease affects the patient and should inform our care, but not generate ageism or therapeutic nihilism.
Once frailty is identified, it allows for further assessment looking at the “Geriatric 5M's framework: Mind, Mobility, Medications, Multicomplexity, and Matters Most.”
Is Frailty the Geriatric Troponin?
Jacqueline M. McMillan, Julian Falutz Journal of the American Geriatrics Society
First published: 12 March 2025 https://doi.org/10.1111/jgs.19423
Category: Geriatrics
Keywords: Anxiety, older, risk (PubMed Search)
Posted: 8/2/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
A scoping review of the literature regarding anxiety in older patients found the follow areas had the biggest impact on anxiety level:
“The variables most strongly associated with anxiety—either as risk or protective factors—are age, female gender, physical activity, physical health conditions, depression, perceived and family support, and social participation. New variables linked to anxiety include body mass index (BMI) and dietary habits.”
Asking questions related to these areas can give you a better picture of your patient’s risk for anxiety.
Geriatrics 2025, 10(4), 83; https://doi.org/10.3390/geriatrics10040083
Category: Geriatrics
Keywords: Geriatric l, trauma, triage (PubMed Search)
Posted: 7/30/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This prospective cohort study from Germany found an under triage rate of 58% of trauma patients over 70 years presenting to 12 trauma centers. One area that consistently lead to undertriage was not using a systolic blood pressure under 110 as a criteria for trauma team activation.
The older cohort had 3 times the mortality than younger, were more likely not to arrive by helicopter and mechanism was more commonly ground level fall. This study echos many others in USA and Australia. Better trauma triage criteria are needed for older patients.
Koch, D.A., Becker, L., Schweigkofler, U. _et al._Undertriage in geriatric trauma: insights from a multicentre cohort study. Scand J Trauma Resusc Emerg Med 33, 123 (2025). https://doi.org/10.1186/s13049-025-01432-0
Category: Geriatrics
Keywords: Geriatric, critical care, vasopressors. (PubMed Search)
Posted: 7/12/2025 by Robert Flint, MD
(Updated: 7/14/2025)
Click here to contact Robert Flint, MD
An open label pragmatic study in 29 Japanese hospitals randomized septic shock patients over age 65 to either a high (MAP 80-85) or control (65-70) group. They then looked at all cause 90 day mortality. The study was stopped early due to a significantly higher percentage of mortality in the higher MAP group.
The study isn’t blinded and is only done in one country, however it does raise the question of what is the ideal MAP for older septic shock patients.
Endo A, Yamakawa K, Tagami T, Umemura Y, Wada T, Yamamoto R, Nagasawa H, Takayama W, Yagi M, Takahashi K, Kojima M, Narita C, Kazuma S, Takahashi J, Shiraishi A, Todani M, Nakane M, Nagata T, Tanaka S, Yokokawa Y, Takahashi K, Ishikita H, Hisamune R, Sasaki J, Muramatsu KI, Sonobe H, Minami K, Hoshi H, Otomo Y; OPTPRESS trial investigators. Efficacy of targeting high mean arterial pressure for older patients with septic shock (OPTPRESS): a multicentre, pragmatic, open-label, randomised controlled trial. Intensive Care Med. 2025 May;51(5):883-892. doi: 10.1007/s00134-025-07910-4. Epub 2025 May 13. PMID: 40358717; PMCID: PMC12130109.
Category: Geriatrics
Keywords: Age friendly, geriatric, healthcare, quality improvement (PubMed Search)
Posted: 7/6/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
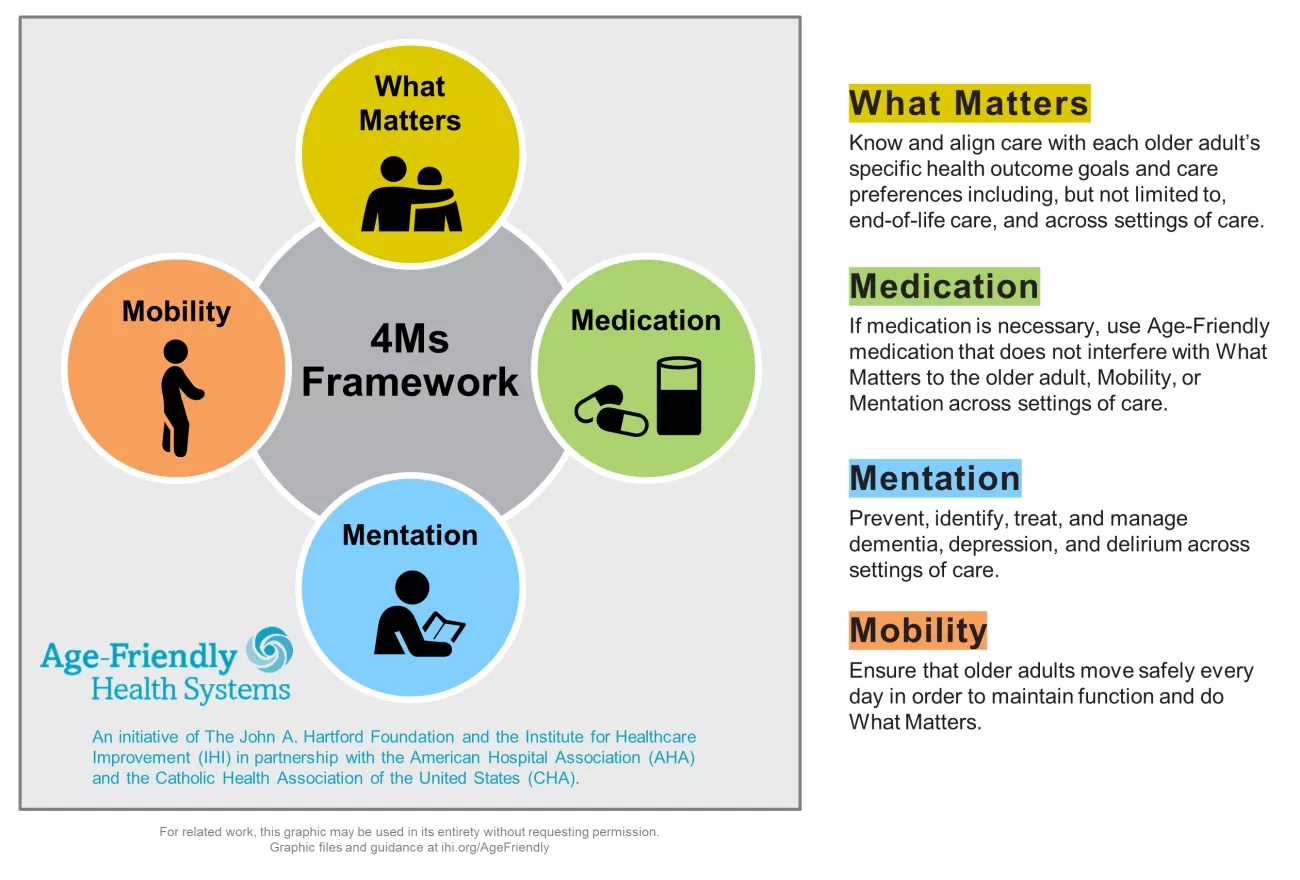
In mid-2024 the Center for Medicare and Medicaid Services introduced a new quality measure entitled Age Friendly Hospital Measure. The initial phase went into effect 1/1/25. It is built around programs from the American College of Surgeons, the American College of Emergency Physicians as well as the Institute for Healthcare Improvement (IHI). It is modeled around the IHI’s 4M Framework.
Category: Geriatrics
Keywords: Beers criteria, geriatric, prescribing, elderly, drug interaction, pharmacology (PubMed Search)
Posted: 11/30/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
As a reminder, prescribing medications to older patients should be done with caution because of changed physiology, co-morbid conditions and other currently used medications. The Beers Criteria is a helpful list of medications that may cause trouble for your older patients. https://www.guidelinecentral.com/guideline/340784/#section-2776198 is a list of medications to either avoid or prescribe carefully in this patient population.
Pay particular attention to medications that have anticholinergic properties as they cause change in mental status and increase the risk for falls.
By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel
Pages: 2052-2081
First Published: 04 May 2023 https://agsjournals.onlinelibrary.wiley.com/doi/epdf/10.1111/jgs.18372
2. https://www.carepatron.com/templates/beers-criteria-template
Category: Geriatrics
Keywords: Geriatric fever score (PubMed Search)
Posted: 9/22/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This study attempts to validate the use of the Geriatric Fever Score to predict 30 day mortality in patients over age 65 presenting to an emergency department with fever.
The Geriatric Fever Score uses: leukocytosis, severe coma, and thrombocytopenia. One point is award for each abnormality.
Not surprisingly, mortality went up with the higher the score (33%, 42% and 57% for 0,1,2 points)
For me, I’m not discharging anyone with severe coma, leukocytosis or thrombocytopenia in this patient population therefore I’m not sure this scale has much utility for the practicing emergency physician.
Akbari, H., Mirfazaelian, H., Safaei, A. _et al._Predicting mortality in geriatric patients with fever in the emergency departments: a prospective validation study. BMC Geriatr 24, 758 (2024). https://doi.org/10.1186/s12877-024-05346-x
Category: Geriatrics
Keywords: Geriatrics, high risk medications, pharmacy (PubMed Search)
Posted: 8/3/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This article serves as a great reminder that our older patients are on a significant amount of medications and many of these medications effect cognition. Cognitively impaired patients are at risk of medication errors. High risk medications in older patients include anticoagulants, opioids, anticholinergics, hypoglycemic/insulin and sedating medications. The authors found:
It is important to ask how the patient takes (or doesn’t take) their medications as well as other social determinate of health such as living alone.
Journal of the American Geriatrics SocietyEarly View
CLINICAL INVESTIGATION
High-risk medication use among older adults with cognitive impairment living alone in the United States
Matthew E. Growdon MD, MPH, Bocheng Jing MS, Kristine Yaffe MD, Leah S. Karliner MD, MAS, Katherine L. Possin PhD, Elena Portacolone MBA, MPH, PhD, W. John Boscardin PhD, Krista L. Harrison PhD, Michael A. Steinman MD
First published: 26 July 2024
