Category: Infectious Disease
Keywords: Mpox, monkeypox, outbreak, democratic republic of congo (PubMed Search)
Posted: 8/25/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Background:
What’s new?
Who is at risk?
Patients with epidemiologic characteristics and lesions or other signs and symptoms consistent with mpox. This includes anyone with travel to DRC or any of its neighboring countries (ROC, CAR, Rwanda, Burundi, Uganda, Zambia, Angola, Tanzania, and South Sudan) in the previous 21 days.
What to look for?
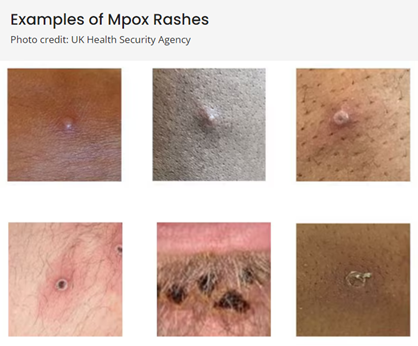
(Above photos from https://www.cdc.gov/poxvirus/mpox/clinicians/clinical-recognition.html)
What to do?
If mpox is suspected in a patient:
Duwell M. Mpox Clinician Letter. Maryland Department of Health. August 19, 2024.
Mpox Caused by Human-to-Human Transmission of Monkeypox Virus in the Democratic Republic of the Congo with Spread to Neighboring Countries. US Centers for Disease Control and Prevention. CDC Health Alert Network, August 7, 2024, 3:15 PM ET, Accessed at https://emergency.cdc.gov/han/2024/han00513.asp# on August 25, 2024.
Mpox. US Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/mpox/index.html, Accessed on August 25, 2024.
