Category: Neurology
Keywords: pseudotumor cerebri, idiopathic intracranial hypertension, headache, lumbar puncture (PubMed Search)
Posted: 11/17/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
-- CSF reforms within 6 hours, making its removal short-term, unless there is a CSF leak.
-- LP can be challenging in obese patients and uncomfortable for patients, in general.
-- LP complications such as low pressure headaches, CSF leak, CSF infection, and intraspinal epidermoid tumors.
Category: Neurology
Keywords: movement disorders, chorea, athetosis, fasiculations, dystonia (PubMed Search)
Posted: 11/10/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: sah, subarachnoid hemorrhage, hunt and hess scale, intracranial hemorrhage (PubMed Search)
Posted: 11/3/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Optimal management of subarachnoid hemorrhage requires prognostic understanding and effective communication with neurology and neurosurgical consultants, as well as the patient and their family members.
It is therefore often helpful to utilize and reference the widely recognized Hunt and Hess Scale in grading symptoms of ruptured cerebral aneurysm and subarachnoid hemorrhage severity:
For your convenience, an online Hunt and Hess Scale calculating tool can be found at:
http://www.mdcalc.com/hunt-and-hess-classification-of-subarachnoid-hemorrhage-sah
The following historical references retrieved from http://www.strokecenter.org/trials/scales/hunt_hess.html:
Category: Neurology
Keywords: csf, meningitis, lumbar puncture, subarachnoid hemorrhage, herpes simplex encephalitis (PubMed Search)
Posted: 10/28/2010 by Aisha Liferidge, MD
(Updated: 10/30/2010)
Click here to contact Aisha Liferidge, MD
Classic Cerebrospinal Fluid Characteristics
Category: Neurology
Keywords: concussion, traumatic brain injury, minor traumatic brain injury (PubMed Search)
Posted: 10/20/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: stroke, cerebral edema, tPA, hemorrhage, NIHSS (PubMed Search)
Posted: 10/13/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
--- High NIH Stroke Scale scores.
--- Large areas of infarct.
--- Cerebellar infarcts.
--- Extended time to tPA administration.
--- Previous stroke.
--- Older age.
Category: Neurology
Keywords: diplopia, cranial nerve palsy, monocular diplopia, binocular diplopia (PubMed Search)
Posted: 10/6/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: ulnar nerve, median nerve, radial nerve (PubMed Search)
Posted: 9/22/2010 by Aisha Liferidge, MD
(Updated: 2/22/2011)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: radial nerve palsy, saturday night palsy, honeymoon palsy, wrist drop (PubMed Search)
Posted: 9/15/2010 by Aisha Liferidge, MD
(Updated: 9/18/2010)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: median nerve block, nerve blok, median nerve (PubMed Search)
Posted: 9/8/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
How to Perform a Median Nerve Block
Category: Neurology
Keywords: ulnar nerve block, ulnar nerve, nerve block (PubMed Search)
Posted: 9/1/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
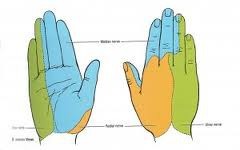
Keywords: hand examination, sensory function, median nerve, ulnar nerve, radial nerve (PubMed Search)
Posted: 8/25/2010 by Aisha Liferidge, MD
(Updated: 8/28/2014)
Click here to contact Aisha Liferidge, MD
-- ulnar nerve >>> supplies palmar surface and dorsal tips of little finger and medial half of ring finger, including
adjacent parts of hand.
-- median nerve >>> supplies palmar and dorsal aspects of thumb, index finger, middle finger, and lateral half
of ring finger, including adjacent parts of hand.
-- radial nerve >>> supplies most of dorsal surface of hand.
Category: Neurology
Keywords: cervicogenic headache, headache (PubMed Search)
Posted: 8/18/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: headaches, cervicogeic headache (PubMed Search)
Posted: 8/12/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Consider the diagnosis of a Cervicogenic Headache when the following findings are present:
A. Pain localized to the neck and occipital region, potentially with projection to forehead, orbits, temples, vertex or ears.
B. Pain is precipitated or aggravated by particular neck movements or sustained postures.
C . At least one of the following:
1. Resistance to or limitation of passive neck movements.
2. Changes in neck muscle contour, texture, tone or response to active and passive stretching and contraction.
3. Abnormal tenderness of neck muscles.
D. Radiological imaging reveals at least one of the following:
1. Movement abnormalities in flexion/extension.
2. Abnormal posture.
3. Fractures, congenital abnormalities, bone tumors, rheumatoid arthritis or other distinct pathology (not spondylosis or osteochondrosis).
1. Headache classification committee of the IHS. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988 8: 1-96.
Category: Neurology
Keywords: Cluster, headaches (PubMed Search)
Posted: 8/4/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Cluster headaches are defined as a group of at least five headache attacks causing unilateral orbital, supraorbital and/or temporal pain, with at least one of the following simultaneous associated findings on the affected side:
Cluster headaches can occur at a frequency of one every other day t eight episodes per day.
Category: Neurology
Keywords: migraine headache with aura, aura, headache (PubMed Search)
Posted: 7/28/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
A. At least two attacks with at least 3 of the following:
1. One or more fully reversible aura symptoms (indicates focal cerebral cortical and/or brain stem functions).
2. At least 1 aura symptom develops gradually over greater than 4 minutes, or 2 or more symptoms occur in succession.
3. No aura symptom lasts greater than 60 minutes.
4. Headache follows aura with free interval of at least 60 minutes.
B. At least 1 of the following aura features establishes a diagnosis of migraine with typical aura:
1. Homonymous visual disturbance.
2. Unilateral paresthesias and/or numbness.
3. Unilateral weakness.
4. Aphasia or speech difficulty.
Category: Neurology
Keywords: Migraine headache without aura, Headache, International Headache Society, International Headache Society Criteria for Migraine (PubMed Search)
Posted: 7/21/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
A.
1. Pulsatile or throbbing in quality
2. Unilateral in location
3. Moderate to severe in intensity
4. Aggravated by activity (i.e.climbing stairs, exertion), plus
B. at least 1 of the following 2 during the headache ("VP"):
1. Vomiting and/or nausea
2. Photophobia and/or phonophobia
Category: Neurology
Keywords: stroke, lacunar infact, clumsy hand dysarthra syndrome, hemiparesis, ataxia (PubMed Search)
Posted: 7/14/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: stroke, brain CT (PubMed Search)
Posted: 7/7/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: TIA, Stroke (PubMed Search)
Posted: 7/1/2010 by Aisha Liferidge, MD
(Updated: 2/1/2026)
Click here to contact Aisha Liferidge, MD
