Category: Cardiology
Keywords: PEA (PubMed Search)
Posted: 2/27/2014 by Semhar Tewelde, MD
(Updated: 3/2/2014)
Click here to contact Semhar Tewelde, MD
Pulseless Electrical Activity (PEA)
ACLS algorithm for PEA focuses on memorizing the “ H's & T's" without a systematic approach on how to evaluate & treat the possible etiologies
A modified approach to PEA focuses on “cause-specific” interventions utilizing two simple tools: ECG and Bedside Ultrasound (US)
Simplified PEA Algorithm
♦1st obtain the ECG and assess the QRS-complex length (narrow vs. wide)
♦ A narrow QRS-complex suggests a mechanical problem: RV inflow or outflow obstruction
Utilize bedside US to assess for RV collapsibility vs. dilation
A collapsed RV suggests tamponade, tension PTX or mechanical hyperinflation
A dilated RV suggests PE
The above listed etiologies all have a preserved/hyperdynamic LV Tx begins w/aggressive IVF’s followed by “cause-specific” therapy: pericardiocentesis, needle decompression, forced expiration/vent management, and thrombolysis respectively
♦ A wide QRS-complex suggests a metabolic (hyperK/acidosis/toxins), ischemic, or LV problem
Utilize bedside US to assess for LV hypokinesis/akinesis
For metabolic/toxic etiologies treat w/calcium chloride and sodium bicarbonate +/- vasopressors
For ischemia and LV failure treat w/cardiac cath. vs. thrombolysis +/- vasopressors/inotropes
♦Trauma and several other etiologies of PEA that are seldom forgotten in any critically ill patient (hypothermia, hypoxia, and hypoglycemia) are not included in this algorithm.
Littmann L, Bustin D, Haley M. A Simplified and Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity. Med Princ Pract 2014; 23:1-6
Category: Cardiology
Posted: 2/16/2014 by Semhar Tewelde, MD
(Updated: 2/1/2026)
Click here to contact Semhar Tewelde, MD
Early Atherosclerosis Detection
50 middle-aged asymptomatic subjects free of vascular disease underwent carotid ultrasound (CUS) for risk stratification were also invited to undergo coronary computed tomography angiography (CCTA) or coronary artery calcium score (CAC) to identify which of the 3 imaging modalities was best at identification of early atherosclerosis
Atherosclerosis was observed in 28%, 78%, and 90% of subjects using CAC, CCTA, and CUS, respectively
36 patients with a CAC score = 0, 69% and 86% had atherosclerosis on CCTA and CUS, respectively
Concordance between modalities was highly variable
CUS and CCTA detection of plaque were significantly more sensitive than CAC
Considering the prevalence of subclinical disease on CUS and CCTA, the threshold at which to treat warrants further research
Schroeder B, Francis G, et al. Early Atherosclerosis Detection in Asymptomatic Patients: A Comparison of Carotid Ultrasound, Coronary Artery Calcium Score, and Coronary Computed Tomography Angiography. Canadian Journal of Cardiology, 2013-12-01, Volume 29, Issue 12, Pages 1687-1694
Category: Cardiology
Posted: 2/2/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Myocardial Infarction in Women After Childbirth
World Health Organization reports that obesity is the 5th leading cause of global death with the highest impact on women <65 years of age
The association of obesity and cardiovascular risk in young women is currently being researched
A recent nationwide cohort looking at obesity and future cardiovascular risk looked at Danish women giving birth (2004-2009) and followed them a median time of 4.5 years
This study grouped women via pre-pregnancy body mass index (BMI)
1. Underweight (BMI <18.5)
2. Normal weight (BMI <25)
3. Overweight (BMI <30)
4. Obese (BMI >30)
Data revealed that healthy women of fertile age, pre-pregnancy obesity alone was associated with increased risk of myocardial infarction in the years after childbirth
Schmiegelow M, Andersson C, Kober L, et al. Prepregnancy Obesity and Associations With Stroke and Myocardial Infarction in Women in the Years After Childbirth. Circulation 2014;129:330-337.
Category: Cardiology
Posted: 1/19/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Pacing Atrioventricular Block
- Atrioventricular (AV) block is classically treated with restoration of heart rate via right ventricular pacing, however high rates of right ventricular pacing is associated w/ left ventricular systolic dysfunction
- A recent multi-center randomized control trial (RCT) assessed the efficacy of right vs biventricular pacing in heart failure w/ AV block [BLOCK HF Trial]
- Primary outcomes of: morbidity, mortality, and adverse left ventricular remodeling were shown to be significantly lower in biventricular vs right ventricular pacing
- In patients with a high rate of pacing and/or an abnormally low left ventricular ejection fraction biventricular pacing may be more advantageous than conventional right ventricular pacing
Curtis A.B., Worley S.J., Adamson P.B.,et al: Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med 2013; 368: 1585-1593
Category: Cardiology
Posted: 1/5/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Assessment of Intermediate Coronary Lesions
- Coronary angiography alone to assess CAD is fraught with subjectivity
- Fractional flow reserve (FFR) has become the standard to assess/quantify obstructive CAD; it determines the myocardial flow in the presence of stenosis identifying the lesion responsible for ischemia
- FFR assesses focal stenosis, but does not consider diffuse atherosclerotic narrowing or microcirculatory dysfunction as contributors of ischemic heart disease
- An index of microcirculatory resistance (IMR) can be concomitantly measured with FFR during cardiac catheterization to specifically evaluate the microvasculature
- Coronary flow reserve (CFR) was the 1st proposed method for assessment of intermediate coronary lesion, but proved suboptimal because of its variability especially in patients with microvascular dysfunction (diabetes, prior MI, etc.)
- Utilization of FFR, IMR, and CFR together support the existence of differentiated patterns of ischemic heart disease & may help to determine future ischemic events
Echavarria-Pinto M, Escaned J, Macias E, et al. Disturbed Coronary Hemodynamics in Vessels With Intermediate Stenosis Evaluated With Fractional Flow Reserve: A Combined Analysis of Epicardial and Microcirculatory Involvement in Ischemic Heart Disease. Circulation Volume 128(24), 17 December 2013, p 2557–2566
Category: Cardiology
Posted: 12/22/2013 by Semhar Tewelde, MD
(Updated: 2/1/2026)
Click here to contact Semhar Tewelde, MD
Metoprolol Usage Cardioprotective
Ibanez B, Sanchez-Brunete V, Pizarro G, et al. Effect of early metoprolol on infarct size in ST-segment-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial. Circulation. 2013 Oct 1; 128(14):1495-503.
Category: Cardiology
Keywords: Cardiac Transplant (PubMed Search)
Posted: 12/1/2013 by Semhar Tewelde, MD
(Updated: 8/28/2014)
Click here to contact Semhar Tewelde, MD
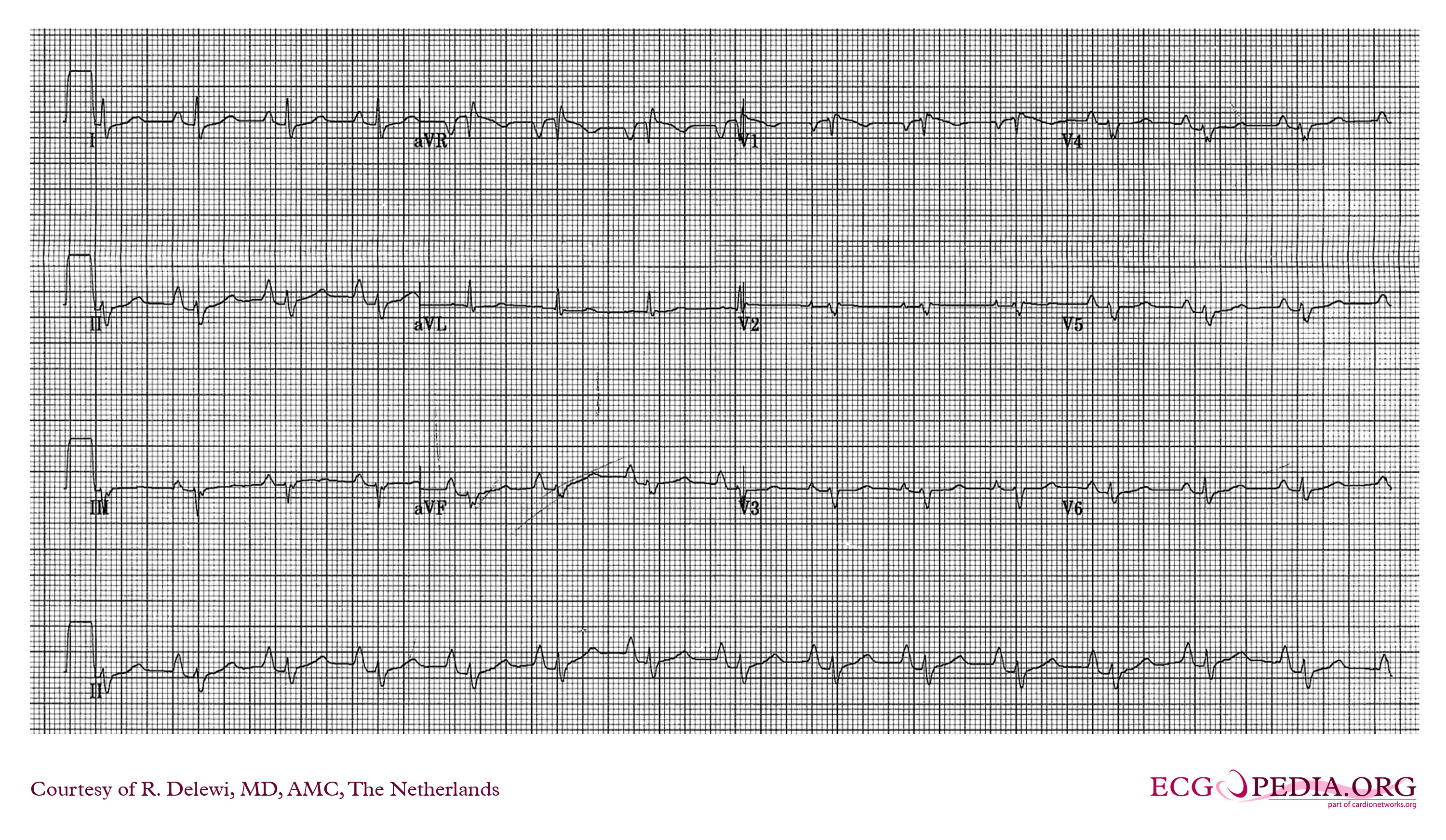
ECG Following Cardiac Transplant
Chou's Electrocardiography in Clinical Practice: Adult and Pediatric 6th Edition
Category: Cardiology
Keywords: Intra-Aortic Balloon Pump, Cardiogenic Shock (PubMed Search)
Posted: 11/15/2013 by Semhar Tewelde, MD
(Updated: 11/17/2013)
Click here to contact Semhar Tewelde, MD
Utility of Intra-Aortic Balloon Pump (IABP)
Kettner J, Sramko M, Holek M, et al. Utility of Intra-Aortic Balloon Pump Support For Ventricular Septal Rupture and Acute Mitral Regurgitation Complicating Acute Myocardial Infarction. American Journal of Cardiology. 2013 Vol 112 Issue 11 Pages 1709-1713
Category: Cardiology
Posted: 11/3/2013 by Semhar Tewelde, MD
(Updated: 11/16/2013)
Click here to contact Semhar Tewelde, MD
Secondary Prevention in AMI
Just as aspirin is pivotal in the treatment of acute coronary syndrome, medications such as beta-blocker, statins, and angiotensin-converting enzyme inhibitors have been proven to be essential in secondary prevention of AMI.
Patients after AMI are typically discharged on appropriate secondary prevention medications; however the prescribed doses are often far below the proven efficacy based on clinical trials.
A review of 6,748 patients from 31 hospitals enrolled in 2 U.S. registries (2003 to 2008) illustrated that only 1 in 3 patients were prescribed these medications at goal doses.
Of patients not discharged on goal doses, up-titration during follow-up occurred infrequently ~25%.
Optimal medication dosing and appropriate titration is integral to prevention of further morbidity and mortality.
Arnold S, Spertus J, Masoudi F, et al. Beyond Medication Prescription as Performace Measure: Optimal Secondary Prevention Dosing After Acute Myocardial Infarction. JACC Nov 5, 2013 Vol 62:19;1791-1801
Category: Cardiology
Posted: 10/20/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Ebstein's Anomaly
Osiro S, Tiwari K, Mathenge N, et al. When Lithum Hurts: A Look at Ebstein Anomaly. Cardiology in Review. Oct 2013, Vol 21(5); pgs 257-263.
Category: Cardiology
Keywords: Aortic Syndrome, Aortic Dissection, Intramural hematoma, Atheromatous ulcer (PubMed Search)
Posted: 10/6/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Acute Aortic Syndromes
Classically, aortic dissection is considered the primary culprit in patients with chest pain that radiates to the back (aortic pain) or chest pain combined with ischemia (cerebral, cardiac, peripheral), syncope, or cardiac arrest. However, it should not be your only concern: the rate of aortic rupture is much higher in penetrating atheromatous ulcer (42%) and intramural hematoma (35%) than in aortic dissection (types A 7.5% and type B 4.1%).
Chest pain with concomitant ischemic symptoms and acute decompensation should prompt consideration of several etiologies under the umbrella of aortic syndromes and not limited to dissection :
Sheikh A, Ali K, Mazhar S. Acute Aortic Syndrome. Circulation 2013;128:1122-1127
Coady MA, Rizzo JA, Elefteriades JA. Pathological Variants of thoracic aortic dissection. Penetrating atherosclerotic ulcers and intramural hematomas. Cardiol Clin. 1999;17:637-657
Category: Cardiology
Keywords: Bundle branch block (PubMed Search)
Posted: 9/22/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Is RBBB More Indicative of Large Anteroseptal MI?
Strauss DG, Loring Z, Selvester RH, et al. Right, But Not Left, Bundle Branch Block Is Associated With Large Anteroseptal Scar. JACC. Sept 2013; 62(11): 959-967.
Category: Cardiology
Posted: 9/8/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
*Please see the attachment below for Figures A-D
1. Adler A, Rosso R, Viskin D, et al. JACC. Sept. 2013: Vol. 62(10) pgs. 863-868
2. Haissaguerre M., Derval N., Sacher F., et al: Sudden cardiac arrest associated with early repolarization. N Engl J Med 2008; 358: 2016-2023
3. Tikkanen J.T., Anttonen O., Junttila M.J., et al: Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med 2009; 361: 2529-2537
Category: Cardiology
Posted: 8/25/2013 by Semhar Tewelde, MD
(Updated: 2/1/2026)
Click here to contact Semhar Tewelde, MD
Palmerini T, et al. Clinical Outcomes With Drug-Eluting and Bare-Metal Stents in Patients With ST-Segment Elevation Myocardial Elevation. JACC. 2-13, Vol. 62:2 pgs.196-504
Category: Cardiology
Posted: 8/5/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Category: Cardiology
Posted: 7/29/2013 by Semhar Tewelde, MD
(Updated: 2/1/2026)
Click here to contact Semhar Tewelde, MD
Tight glycemic control (HbA1C<7%) has previously been recommended in CAD based on data from the United Kingdom Prospective Diabetes Study (UKPDS)
A recent study (JACC) evaluated the relationship between glycemic control, cardiovascular disease (CVD) risk, and all-cause mortality
Patients with a mean HbA1C 7-7.4% were compared to those with mean HbA1C <6%; tight glycemic control had a 68% increased risk of CVD hospitalization
Lenient HbA1C>8.5% also had significantly higher risk
CVD risk and all-cause mortality is greater with both aggressive and lax glycemic control and the optimal reference range may lie between 7-7.4%
| Nichols G, Joshua-Gotlib S, Parasuraman. Glycemic Control and Risk of Cardiovascular Disease Hospitalization and All-Cause Mortality. JACC. 62: 2; 121-127. |
Category: Cardiology
Posted: 7/21/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Westfall M, Krantz S, Mullin C, Kaufman C. Mechanical versus manual chest compressions in out-of-hospital cardiac arrest. Crit Care Med 2013 Jul; 41(7):1782-9
Category: Cardiology
Posted: 7/14/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Radiation therapy is frequently utilized in the management of numerous thoracic malignancies
Cardiovascular disease is now the leading cause of nonmalignancy death in radiation-treated cancer survivors
The spectrum of radiation-induced cardiac disease is broad
The relative risk of CAD, CHF, pericardial/valvular disease, and conduction abnormalities is particularly increased
Early identification of potential cardiac complications w/cardiac MR and echocardiography provides an opportunity for regular assessment and potentially improved long term mortality
Jaworksi C, Mariani J, et al. Cardiac Complication of Thoracic Irradiation. JACC Vol 61, No 23, 2013.
Category: Cardiology
Posted: 7/7/2013 by Semhar Tewelde, MD
(Updated: 2/1/2026)
Click here to contact Semhar Tewelde, MD
Barthwal SP, Agarwal R, Sarkari NB et al. Diagnostic Significance of TI < T III and TVI > TV6 signs in ischemic heart disease . J Assoc Phys India 1993;41:26-7
Category: Cardiology
Posted: 6/30/2013 by Semhar Tewelde, MD
(Updated: 2/1/2026)
Click here to contact Semhar Tewelde, MD
Kini A, Baber U, et al. Changes in Plaque Lipid Content After Short-Term Intensive Versus Standard Statin Therapy. JACC. Vol. 62, No. 1, 2013
