Category: Cardiology
Keywords: Brain-heart syndrome, Neurogenic Stress Cardiomyopathy (PubMed Search)
Posted: 4/27/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
Category: Cardiology
Keywords: Out of hospital cardiac arrest, OHCA, Prehospital airway management (PubMed Search)
Posted: 4/13/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
Optimal out of hospital cardiac arrest (OHCA) airway management strategies remain unclear. In the US, 80% of OHCA patients receive prehospital airway management, most commonly endotracheal intubation (ETI). There is growing enthusiasm for use of supra-glottic airways (SGA) by EMS because of ease of insertion, and the thought that use of SGA reduces interruptions in chest compressions. More recently, studies have suggested improved survival without the insertion of any advanced airway device at all.
A recent secondary analysis of OHCA outcomes in the Cardiac Arrest Registry to Enhance Survival (CARES) compared patients receiving endotracheal intubation (ETI) versus supra-glottic airway (SGA), and also patients receiving [ETI or SGA] with those receiving no advanced airway.
Of 10,691 OHCA, 5591 received ETI, 3110 SGA, and 1929 had no advanced airway. Unadjusted neurologically-intact survival was: ETI 5.4%, SGA 5.2%, no advanced airway 18.6%. Compared with SGA, ETI achieved higher sustained ROSC, survival to hospital admission, hospital survival, and hospital discharge with good neurologic outcome. Moreover, compared with [ETI or SGA], patients who received no advanced airway attained higher survival to hospital admission, hospital survival, and hospital discharge with good neurologic outcome.
Conclusion: In CARES, patients receiving no advanced airway exhibited superior outcomes than those receiving ETI or SGA. When an advanced airway was used, ETI was associated with improved outcomes compared to SGA.
McMullan J, Gerecht R, Bonomo J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation. 2014;85(5):617–622. doi:10.1016/j.resuscitation.2014.02.007.
Category: Cardiology
Keywords: Cardiac arrest, LVAD, CPR, Chest compressions (PubMed Search)
Posted: 3/23/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
The number of patients with left ventricular assist devices (LVADs) is increasing and development of optimal resuscitative strategies is becoming increasingly important. Despite a lack of evidence, many device manufacturers and hospitals have recommended against performing chest compressions because of fear of cannula dislodgment or damage to the outflow conduit.
A recent retrospective analysis of outcomes in LVAD patients who received chest compressions for cardiac arrest did not support the theory that LVADs would be harmed by conventional resuscitation algorithms.
The study was a limited case series of only 8 LVAD patients over a 4 year period. All patients received compressions and device integrity was subsequently assessed by blood flow data from the LVAD control monitor or by examination on autopsy. Although more research is necessary to determine the utility and effectiveness of compressions in this population, none of the patients in this study had cannula dislodgment and half of the patients had return of neurologic function.
Shinar Z, Bellezzo J, Stahovich M, et al. Chest compressions may be safe in arresting patients with left ventricular assist devices (LVADs). Resuscitation. 2014. doi:10.1016/j.resuscitation.2014.01.003.
Category: Cardiology
Keywords: Echo, Aortic Dissection (PubMed Search)
Posted: 3/9/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
Early diagnosis and surgical consultation for dissection of the ascending aorta can be life saving. Emergency physicians are increasingly using focused cardiac ultrasound to assess chest pain patients in the ED.
The suprasternal notch view (SSNV), may provide additional information in the assessment of thoracic aortic pathology. A recently performed pilot study aimed to determine the accuracy of using the SSNV, in addition to the more traditional parasternal long axis view in assessing aortic dimensions as well as pathology compared to CTA of the chest.
Using a maximal normal thoracic aortic diameter of 40 mm, diagnostic accuracy in detecting dilation of the aorta was 100%. The study showed that the SSNV is feasible and demonstrates high agreement with measurements made on CTA of the chest.
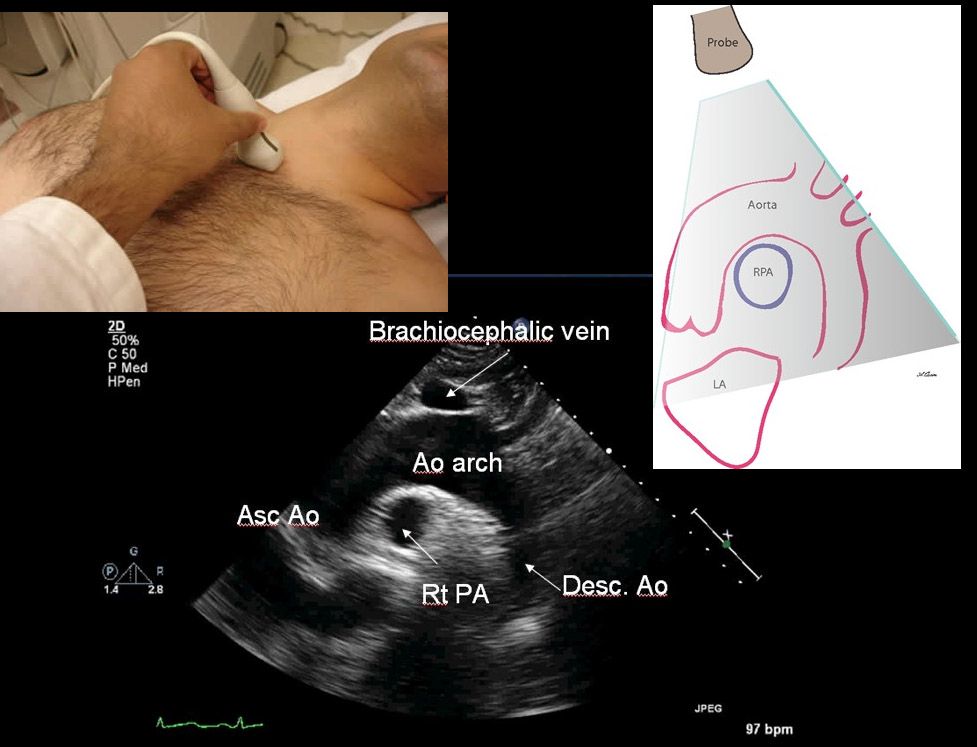
Kinnaman KA, Rempell JS, Kimberly HH, et al. Accuracy of Suprasternal Notch View Using Focused Cardiac Ultrasound to Evaluate Aortic Arch Measurements. YMEM. 2013;62(S):S81. doi:10.1016/j.annemergmed.2013.07.042. Image: http://echocardiographer.org/TTE.html
Category: Cardiology
Keywords: ACS, Stress Test (PubMed Search)
Posted: 2/23/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
1. Banerjee A, Newman DR, Van den Bruel A, Heneghan C. Diagnostic accuracy of exercise stress testing for coronary artery disease: a systematic review and meta-analysis of prospective studies. International Journal of Clinical Practice. 2012;66(5):477–492.
2. Walker J, Galuska M, Vega D. Coronary disease in emergency department chest pain patients with recent negative stress testing. West J Emerg Med. 2010;11(4):384–388.
3. Nerenberg RH, Shofer FS, Robey JL, Brown AM, Hollander JE. Impact of a negative prior stress test on emergency physician disposition decision in ED patients with chest pain syndromes. The American journal of emergency medicine. 2007;25(1):39–44.
Category: Cardiology
Keywords: ECG, STEMI, aVL (PubMed Search)
Posted: 2/9/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
The importance of new ST-segment depressions (STD) and/or T wave inversions (TWI) in lead aVL have not been emphasized or well recognized across specialties. Computer-assisted ECG readings typically report these findings as normal or nonspecific.
There is growing evidence that changes in lead aVL are abnormal, and that paying attention to that lead can be clinically useful. Reciprocal changes presenting as STD or TWI in lead aVL may be indicative of a significant coronary artery lesion and can sometimes be the only ECG manifestation of acute MI.
STD in lead aVL is considered a sensitive marker for early inferior STEMI, and has been shown to help differentiate STEMI from pericarditis. Another recent retrospective study suggests that TWI in aVL might be associated with significant LAD lesions.
Bottom Line: Paying close attention to subtle changes and abnormalities in lead aVL may help in early identification and initiation of therapy for patients who are having an acute MI.
Hassen GW, Costea A, Smith T, et al. The Neglected Lead on Electrocardiogram: T Wave Inversion in Lead aVL, Nonspecific Finding or a Sign for Left Anterior Descending Artery Lesion?. Journal of Emergency Medicine. 2014;46(2):165–170.
Category: Cardiology
Keywords: Wide complex tachycardia, ventricular tachycardia (PubMed Search)
Posted: 1/26/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
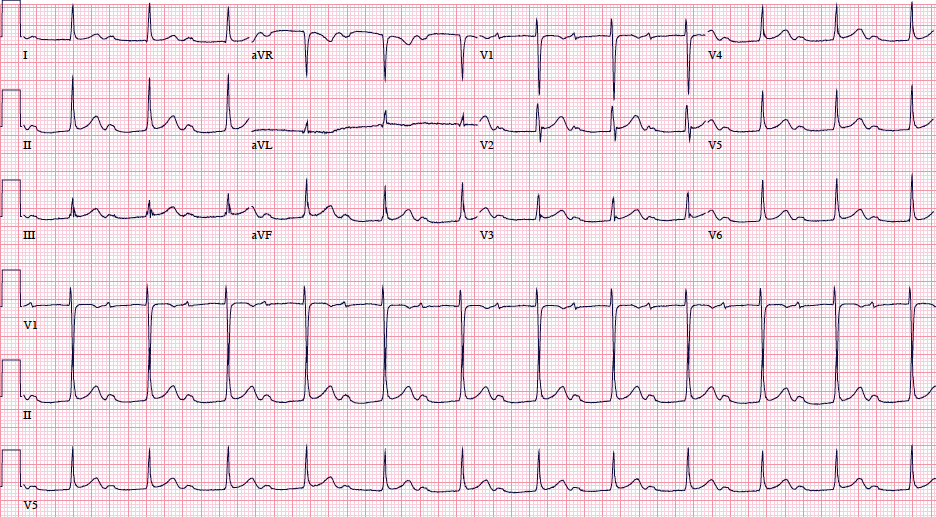
A 48 year old woman has acute chest pain and palpitations over the past several hours. She has felt similar palpitations in the past but never sought medical attention. She arrives to your ED alert and anxious. HR = 270, BP=130/100. ECG is below. What’s the diagnosis and treatment?
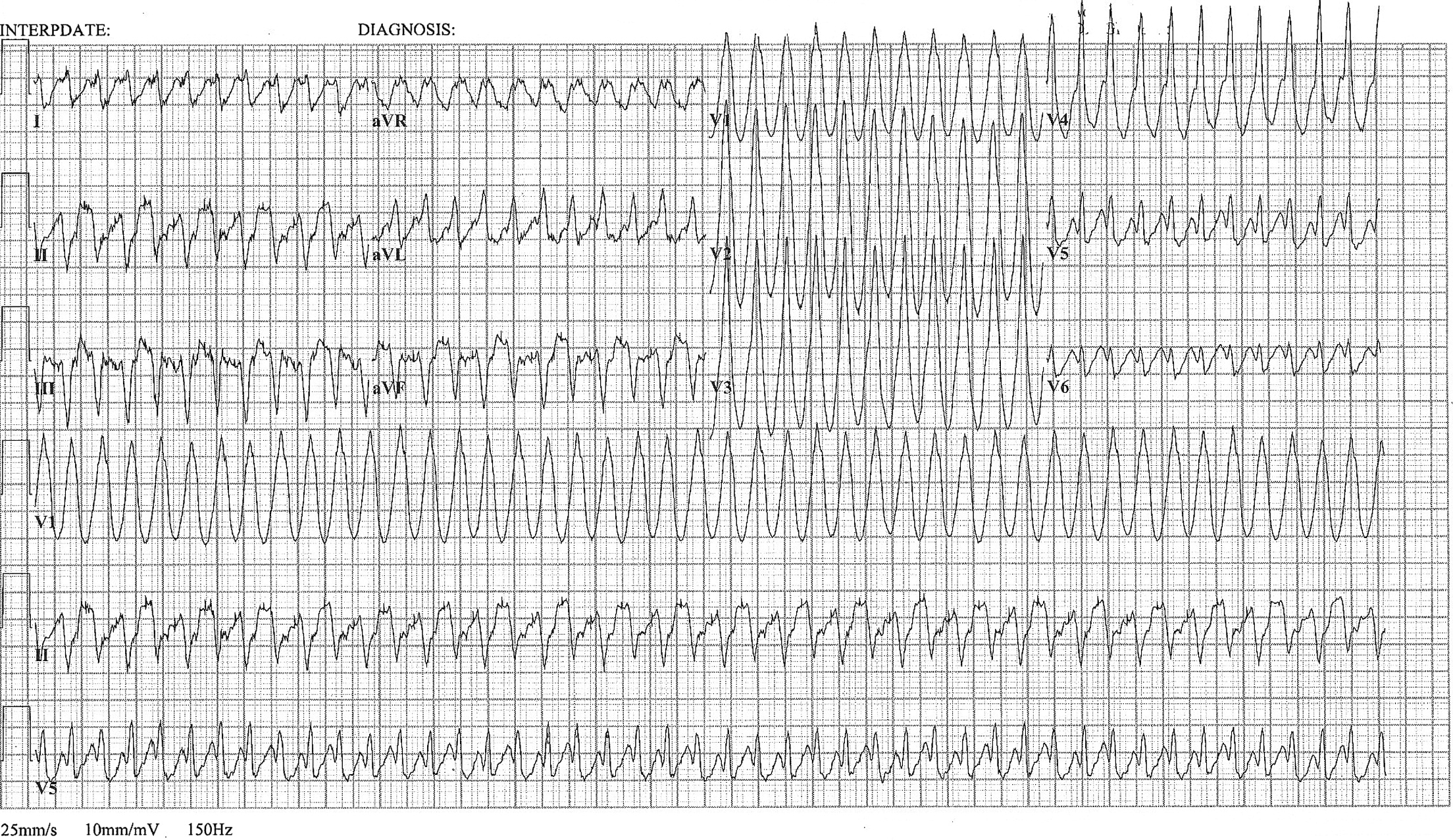
Most wide complex regular tachycardias are ventricular tachycardia (VT). However, supraventricular tachycardias can also cause wide complexes through aberrant conduction and accessory pathways.
Nelson JG, Zhu DW. Atrial Flutter with 1:1 Conduction in Undiagnosed Wolff-Parkinson-White Syndrome. The Journal of Emergency Medicine. January 2014. Pubmed Link
Category: Cardiology
Keywords: PVC, Premature ventricular beats, Premature ventricular complexes (PubMed Search)
Posted: 1/12/2014 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Differentiation between right and left ventricular origin of premature beats can be useful clinically.
PVCs arising from the right ventricle have a left bundle branch block morphology (dominant S wave in V1)
PVCs arising from the left ventricle have a right bundle branch block morphology (dominant R wave in V1)
Left Ventricular premature beats are more often associated with heart disease and may precipitate ventricular fibrillation, whereas right ventricular premature beats are commonly seen in individuals with normal hearts.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Wagner, Galen. Chapter 15 - Premature Beats. Marriott's Practical Electrocardiography, 12th Edition. 2013
Category: Cardiology
Keywords: ST-elevation, Cardiology, MI (PubMed Search)
Posted: 12/29/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
There is debate and confusion regarding where and how to measure ST elevation (STE). Do you measure the STE at the J-point? Or at 40 msec after the J-point? And how much STE is considered significant? The current guidelines have clarified this issue.
- STE should be measured at the J-point.
- STEMI is defined by STE ≥ 1 mm in at least 2 contiguous leads, with the exception of leads V2-V3.
- STEMI is defined by STE ≥ 2 mm in leads V2-V3 in men.
- STEMI is defined by STE ≥ 1.5 mm in leads V2-V3 in women.
For more cardiology pearls from the 2013 literature , check out Amal Mattu's Articles You've Gotta Know!
Want more emergency cardiology pearls? Follow me @alifarzadmd
2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction
O'Gara PT, Kushner FG, Ascheim DD, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Circulation. 2013;127:e362-e425 Pubmed Link
Category: Cardiology
Keywords: ACS, Chest Pain, HEART score (PubMed Search)
Posted: 12/8/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Bottom-line: The HEART score can help to objectively risk stratify ED patients with chest pain into low, intermediate, and high risk groups. Using the HEART score can also facilitate more efficient and effective communication with colleagues.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. International Journal of Cardiology. 2013;168(3):2153–2158.
Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191–196.
Category: Cardiology
Keywords: Therapeutic Hypothermia, ROSC, Cardiac Arrest, Resuscitation (PubMed Search)
Posted: 11/23/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Want more emergency cardiology pearls? Follow me @alifarzadmd
Category: Cardiology
Keywords: AMI, LBBB, Sgarbossa criteria (PubMed Search)
Posted: 11/9/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Diagnosis of STEMI in patients with LBBB can be challenging. Guidelines that previously recommended emergent reperfusion for these patients have been reconsidered to avoid inappropriate cath lab activation and fibrinolytic therapy.
The 2013 ACC/AHA STEMI guidelines no longer consider new or presumably new LBBB a STEMI equivalent. This dramatic change may prevent inappropriate therapy for some, but fail to help identify patients with LBBB who are having STEMI's. Delayed reperfusion in this population could be fatal and is estimated to affect 5,000-10,000 patients per year in the US alone.
The Sgarbossa ECG criteria are the most validated tool to aid in the diagnosis of STEMI in the presence of LBBB. A Sgarbossa score of ≥ 3 has high specificity (>98%) and positive predictive value for acute MI and angiography-confirmed coronary occlusion. The following algorithm has been recently proposed to identify the high-risk population in which reperfusion therapy would be denied by the 2013 STEMI guidelines.
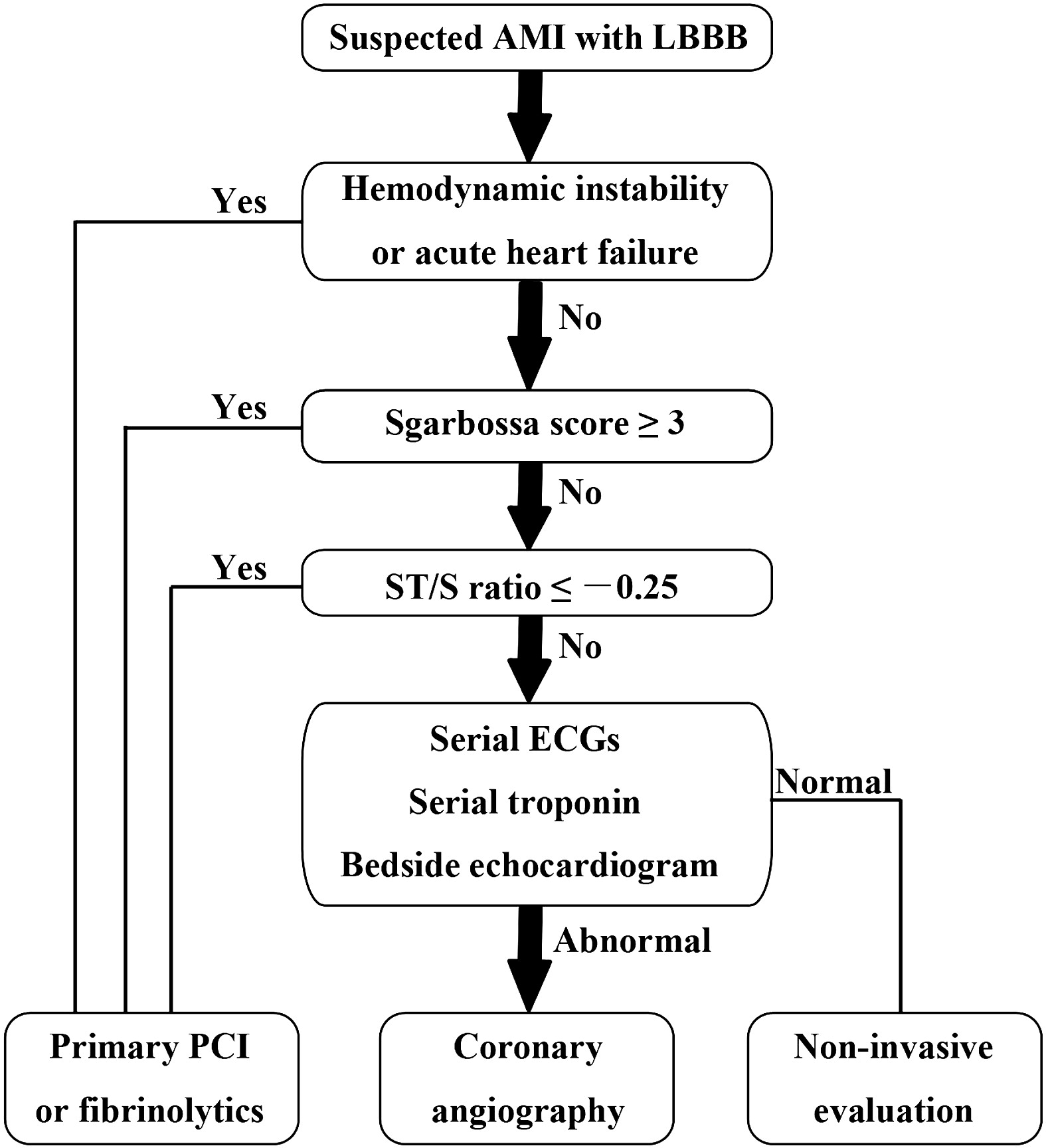
Watch this video to review Sgarbossa criteria and the modified Sgarbossa rule.
Want more emergency cardiology pearls? Follow me @alifarzadmd
The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? American Heart Journal. 2013;166(3):409–413.
Category: Cardiology
Keywords: AV Block (PubMed Search)
Posted: 10/27/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
First-degree atrioventricular (AV) block is defined as an abnormally prolonged PR-interval >200ms. Although traditionally considered to be a benign clinical entity, not all first degree AV blocks are treated the same.
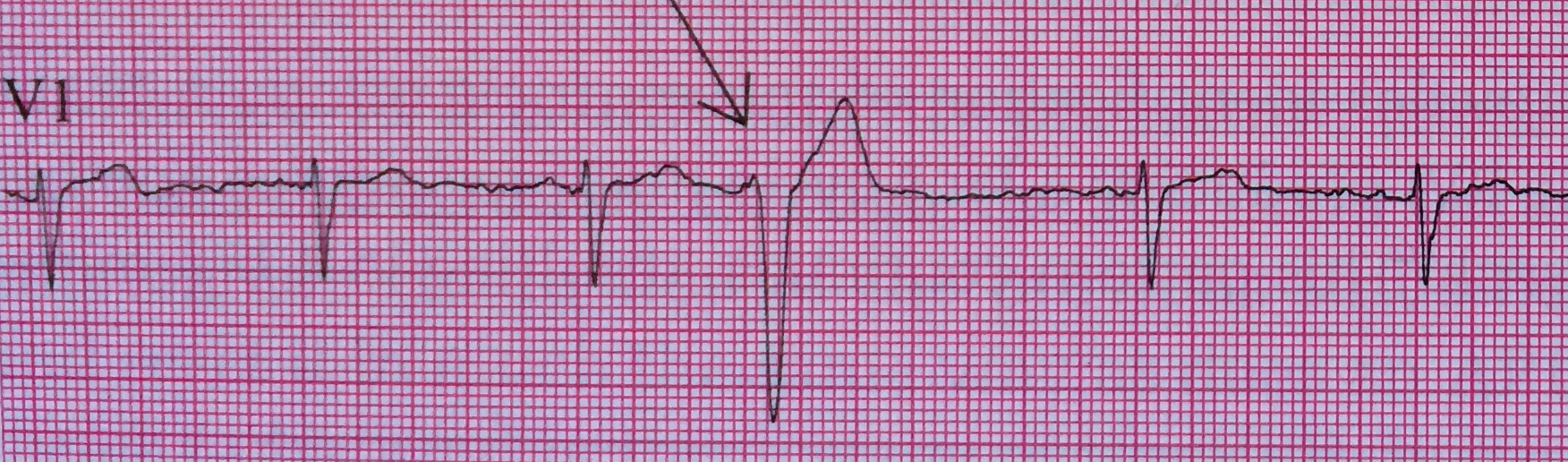
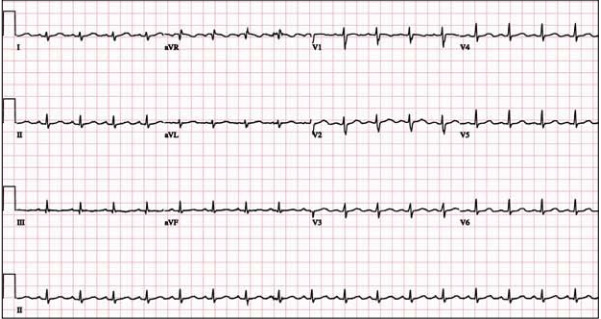
Markedly prolonged PR-intervals (PR >300ms) can cause symptoms and hemodynamic compromise due to inadequate timing of atrial and ventricular contractions. Consider the following ECG from a 32 YOF with intermittent episodes of syncope and dizziness…
There is marked first degree AV block (PR=434 ms). When the PR-interval gets too long, AV dyssynchrony compromises ventricular filling and decreases cardiac output, similar to the so-called pacemaker syndrome.
Current ACC/AHA guidelines state that permanent pacemaker implantation is reasonable for marked first degree AV block with hemodynamic compromise or symptoms similar to those of pacemaker syndrome. (Class IIa, Level of Evidence B). The guidelines caution that pacemakers are not indicated in asymptomatic patients with isolated first degree AV block.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Special thanks to Dr. Brandon Cole for submitting the ECG
References / Further Reading (Attached)
First-Degree AV Block-An Entirely Benign Finding or a Potentially Curable Cause of Cardiac Disease? Annals of Noninvasive Electrocardiology.2013;18(3):215–224. doi:10.1111/anec.12062.
ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008;117(21):e350–e408. doi:10.1161/CIRCUALTIONAHA.108.189742.
Category: Cardiology
Keywords: Dyspnea, Chest Pain (PubMed Search)
Posted: 10/13/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
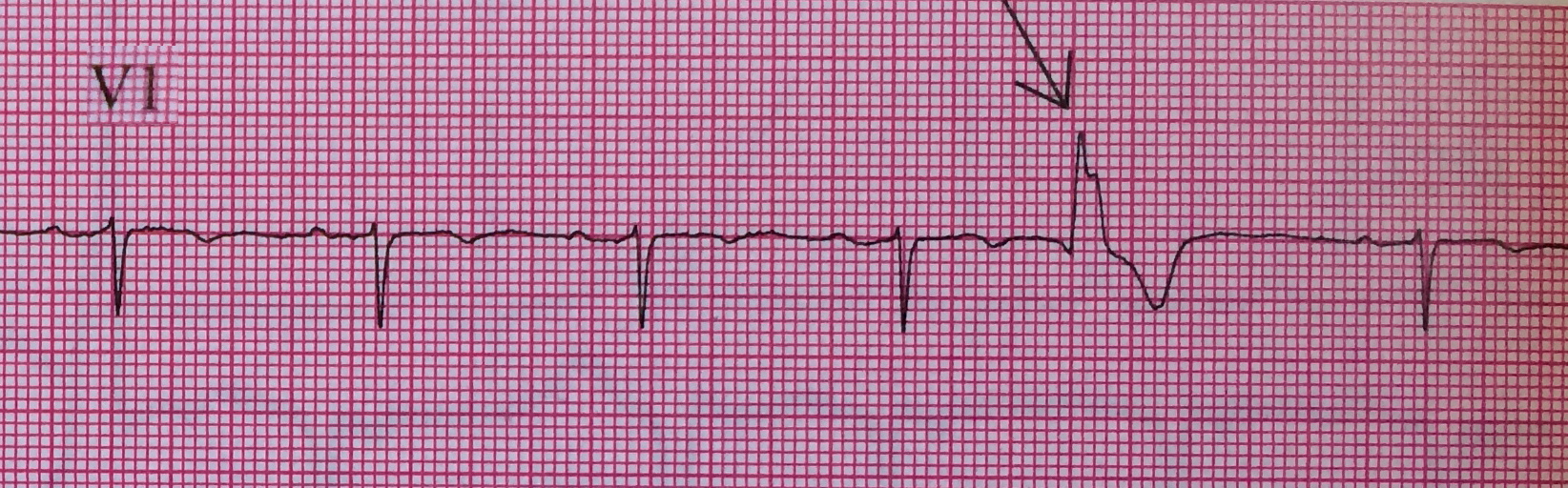
A 48 year-old female presents to the ED with progressive dyspnea and chest discomfort over the past 3 months. HR = 105, BP = 100/60 mmHg, with mild JVD on exam. Her ECG is shown below. What ECG abnormalites are present? What does your differential diagnosis include? What is the best initial diagnostic test?
The ECG shows sinus tachycardia at rate of 107 with low QRS voltage diffusely. Echocardiogram revealed significant pericardial effusion with signs of impending tamponade. Emergent pericardiocentesis was performed and her symptoms improved.
Low QRS voltage (LQRSV)
LQRSV Differential
Want more emergency cardiology pearls? Follow me @alifarzadmd
Category: Cardiology
Posted: 9/29/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
The primary goal in management of STEMI is rapid coronary revascularization. STEMI's are occasionally complicated by ventricular fibrillation (VF) arrest. High quality chest compressions and early defibrillation will improve survival. But what can be done in cases where conventional ACLS measures fail and patients have shock-refractory VF?
Some have suggested that emergent PCI with ongoing CPR en route may be beneficial. This option may be considered in close consultation with cardiology if the arrest is thought to be driven by ongoing ischemia and infarction. However, definitive data is lacking and this has only been described in a handful of case reports.
There may also be a role for venoarterial ECMO to aid in perfusion of vital organs and limit the risk of multisystem organ failure. The ECMO circuit can also help facilitate therapeutic hypothermia after the culprit vessel(s) is revascularized and rhythm is restored.
Chances for survival are highest in younger patients, those that do not have chronic illnesses, and those who received immediate CPR after arrest.
Summary:
Consider emergent consultation for salvage PCI and ECMO in select cases of shock-refractory ventricular fibrillation associated with STEMI
Want more emergency cardiology pearls? Follow me @alifarzadmd
A recently published case report (attached) presents a fascinating case where salvage PCI and ECMO were used for shock-refractory VF. The patient survives with good neurological outcome. It highlights the multidisciplinary cooperation and resources necessary to utilize these heroic practices.
Brown DFM, Jaffer FA, Baker JN, Gurol ME. Case records of the Massachusetts General Hospital. Case 28-2013. A 52-year-old man with cardiac arrest after an acute myocardial infarction. N Engl J Med. 2013;369(11):1047–1054. doi:10.1056/NEJMcpc1304164.
Category: Cardiology
Keywords: Acute Pericarditis, Colchicine (PubMed Search)
Posted: 9/15/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Colchicine is known to be effective in treatment of recurrent pericarditis, but until recently its efficacy during the first attack of acute pericarditis has been uncertain.
A recent multicenter, double-blinded, RCT of patients with acute pericarditis found colchicine to be effective in reducing the rate of incessant or recurrent pericarditis (primary outcome), as well as the rate of hospitalization. Here are some highlights:
Bottom-line:
Colchicine is a safe and effective drug for the treatment of acute pericarditis. Consider adding colchicine to conventional therapies to reduce duration of symptoms, recurrences, and rate of hospitalization.
Imazio M, Brucato A, Cemin R, et al. A Randomized Trial of Colchicine for Acute Pericarditis. N Engl J Med. 2013 (.pdf attached)
Do you know the ECG findings of pericarditis and how to differentiate from other causes of diffuse ST-segment elevation? Check out these previous ECG videos to refresh your memory...
STEMI vs. Benign early repolarization vs. Pericarditis
Category: Cardiology
Keywords: Hypertension (PubMed Search)
Posted: 9/1/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Adult ED patients are commonly found to have markedly elevated blood pressures (>160/100) without any signs or symptoms of acute organ injury (ie, cardiovascular, renal, or neurological).
A recently revised ACEP clinical policy aims to guide emergency physicians in the evaluation and management of such patients.
They make the following recommendations (Level C):
Bottom-line:
There's little evidence to guide the decision of which patients with markedly elevated blood pressures to test or treat in the ED. This new clinical policy suggests that routine screening and treatment is not required. Asymptomatic patients should be referred for close follow-up, but consider a BMP in patients with poor follow up.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Wolf SJ, Lo B, Shih RD, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients in the Emergency Department with Asymptomatic Elevated Blood Pressure. Ann Emerg Med. 2013;62(1):59–68.
