Category: Critical Care
Posted: 2/26/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Excessive and improper administration of local anesthetic (a.k.a. local anesthetic systemic toxicity or L.A.S.T.) can lead to cardiac toxicity with symptoms ranging from benign arrhythmias to overt cardiac arrest.
Administration of a 20% intra-lipid emulsion has been experimentally known to reverse L.A.S.T in animal models, but in 2006 the first documented human case of ILE was successfully used during cardiac arrest secondary to L.A.S.T. with hemodynamic recovery and good neurologic outcome. Many case reports have emerged since then, including the use of ILE in toxicity with other lipophilic drugs (e.g., calcium channel blockers, tricyclic antidepressants, etc.)
Several mechanisms have been proposed explaining how ILE works. They include:
Dosing of ILE:
Check out this video by our own Dr. Bryan Hayes(@PharmERToxGuy) and Lipidrescue.org for more information.
Weinberg, G. Lipid emulsion infusion: resuscitation for local anesthetic and other drug overdose. Anesthesiology 2012 Jul;117(1):180-7.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
68 year-old female presents with stridor and palpable goiter. Here's a clip from CT of the chest. What's the diagnosis?
Category: Critical Care
Posted: 2/12/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Propofol is generally a well-tolerated sedative / amnestic but occasionally it can lead to the propofol infusion syndrome (PRIS); a metabolic disorder causing end-organ dysfunction.
Suspect PRIS in patients with increasing lactate levels, worsening metabolic acidosis, worsening renal function, increased triglyceride levels, or creatinine kinase levels. End-organ effects include:
The true incidence of PRIS is unknown, however, certain risk factors have been identified:
Prevent PRIS by using adequate analgesia (with morphine or fentanyl) post-intubation, which may reduce the overall dosage of propofol ultimately reducing the risk.
If PRIS develops, stop propofol and provide supportive care; IV fluids, ensuring good urine output, adequate oxygenation, dialysis (if indicated), vasopressor and inotropic support.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/10/2013 by Haney Mallemat, MD
(Updated: 2/11/2013)
Click here to contact Haney Mallemat, MD
A 25 year-old female presents complaining of a "net-like" rash bilaterally on her medial thighs. She denies any pain but states that the rash looks “pretty scary” What's the diagnosis?

Answer: Erythema ab igne (a.k.a. "toasted-skin syndrome")
Erythema ab igne
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/4/2013 by Haney Mallemat, MD
(Updated: 3/20/2013)
Click here to contact Haney Mallemat, MD
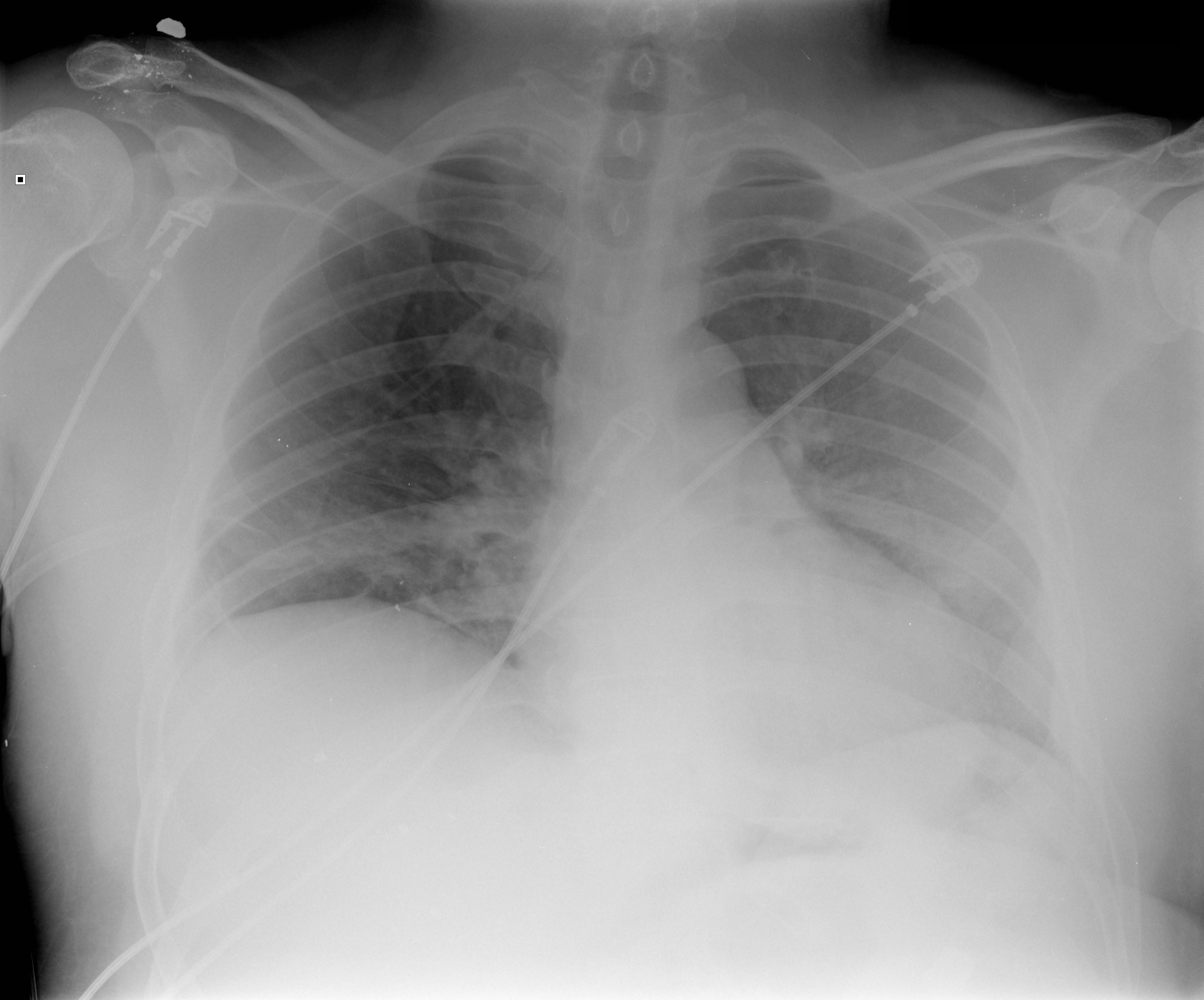
40 year-old male presents with fever, chills, & cough. What’s the diagnosis and the MOST likely cause?
Answer: Pneumatocele from MRSA pneumonia
Pneumatocele
Pneumatoceles are thin-walled, air-filled cysts with lung parenchyma; they may be solitary or multiple
Most commonly a sequellae to pneumonia secondary to Staphylococcus aureus (up to 85% of cases), although other etiologic agents have been found (Streptococcus pneumonia, E. coli, Klebsiella, Adenovirus and Tuberculosis). Non-infectious causes include trauma, hydrocarbon ingestion, and positive pressure ventilation.
Pneumatoceles are typically asymptomatic and require treatment of the inciting etiology (e.g., antibiotics for pneumonia), but complications may occur including tension pneumatocele, pneumothorax, and secondary infection of the pneumatocele.
Surgical resection is typically not needed but percutaneous catheter drainage may be required if the pneumatocele involves >50% of the hemithorax
Advise patients against exposure to high altitudes, skydiving and scuba diving until pneumatocele(s) resolve, to avoid progression to pneumothorax.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 1/29/2013 by Haney Mallemat, MD
(Updated: 1/30/2013)
Click here to contact Haney Mallemat, MD
The updated Surviving Sepsis Guidelines have been released (click here) and here are some recommendations as they pertain to hemodynamic management (grades of recommendations in parenthesis).
Fluid therapy
Vasopressors (targeting MAP of at least 65 mmHg)
Corticosteroids
Inotropic Therapy
Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock. Crit Care Med. 2013 Feb;41(2):580-637.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/28/2013 by Haney Mallemat, MD
(Updated: 1/29/2013)
Click here to contact Haney Mallemat, MD
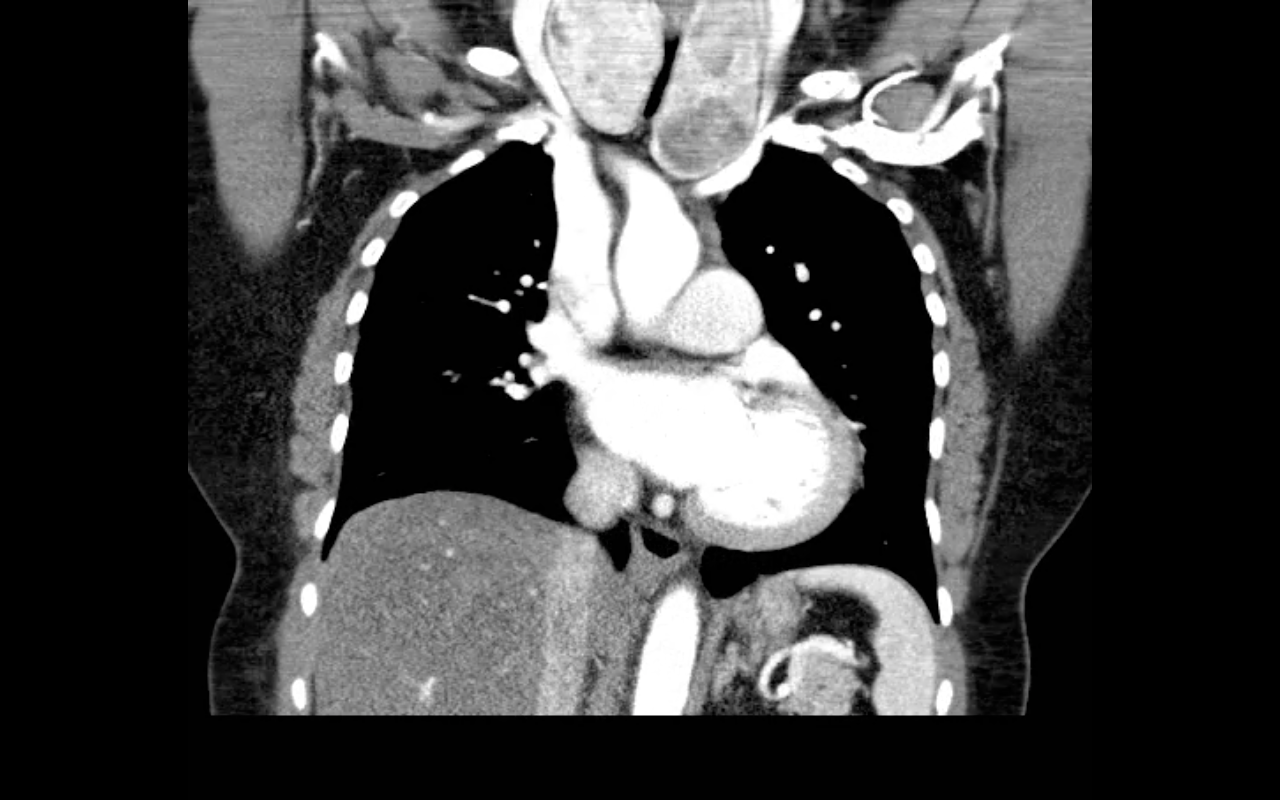
40 year-old female drove into a ditch. Right sided chest pain and stable vitals. Here's the CT but what do you think the initial CXR showed (Hint: it's a trick)?
Here's the initial CXR. Click here for the video presentation.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/21/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
45 year-old male complains of chest pain and cough. He also tells you, "...oh, and by the way doc, I just smoked something." What's the diagnosis?
Visual pearls is two years old!!! I want to take this time to thank you all for your support....and now, your answer.
Restrepo, C. et al. Pulmonary complications from cocaine and cocaine-based substances: imaging manifestations. Radiographics. Jul-Aug 2007; 27(4): 941-56
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 1/15/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intra-aortic balloon pumps (IABP) are devices that provide hemodynamic support during cardiogenic shock; the balloon inflates during diastole (improving coronary artery perfusion) and deflates during systole (reducing afterload and improving systemic perfusion). Click here to see a 41 second video illustrating how it works.
Several guidelines recommend placement of an IABP for patients in cardiogenic shock secondary to acute myocardial infarction (AMI), if early revascularization (e.g., CABG) is planned (Class I recommendation). Data behind this recommendation, however, is limited.
The IABP-SHOCK II trial was a randomized, multi-center, open-label study that enrolled 600 patients (598 in the analysis) with cardiogenic shock secondary to AMI (STEMI or NSTEMI). Patients were randomized to the control group (receiving standard therapy; N=298) or the experimental group (receiving IABP; N=300).
No significant difference was found between groups with respect to 30-day mortality (primary end-point), secondary end-points (e.g., time to hemodynamic stabilization, renal function, lactate levels, etc.), or complications (e.g., major bleeding, peripheral ischemic complications, etc.).
Bottom line: Perhaps it is time to reassess the approach to cardiogenic shock secondary to AMI when early revascularization is planned. At this time consultation with local expertise is recommended.
Category: Visual Diagnosis
Posted: 1/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
4 year-old female with the post-procedural CXR shown below. What's the diagnosis? (Hint: use the zoom...this one is tricky)
Answer: Nasogastric tube in the left mainstem bronchus. Patient was asymptomatic but ironically bubbling was heard when air was injected into the NG tube.
Nasogastric tube (NGT) pearls
The risk of NGT misplacement is 4% in adults, but is 21-43% in children.
Risk factors for misplacement are:
The ability to aspirate gastric contents, pH testing of the aspirated fluid, and the auscultation of “bubbling” over the epigastrium have all been suggested as reliable methods to confirm proper placement; unfortunately, they are often unreliable.
Visualization of the NGT by X-ray is the only way to be 100% certain of placement.
The risks of misplacement include pneumonia and pneumothorax.
Farrington et al. Nasogastric tube placement verification in pediatric and neonatal patients. Pediatric Nursing. Jan-Feb 2009. Vol 35. Issue 1.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 1/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) or DIHS (Drug-Induced Hypersensitivity Syndrome) is a potentially life-threatening adverse drug-reaction.
Incidence is 1/1,000 to 1/10,00 drug exposures. It occurs 2-6 weeks after the drug is first introduced, distinguishing it from other adverse drug-reactions which typically occur sooner.
The syndrome classically includes:
The most commonly implicated drugs are anticonvulsants (e.g., carbamazepine, phenobarbital, and phenytoin), sulfonamides, and allopurinol.
Recovery is typically complete after discontinuing the offending drug; systemic steroids may promote resolution of the illness.
Cacoub P. et al. The DRESS syndrome: a literature review. Am J Med 2011 Jul;124(7):588-97. http://www.ncbi.nlm.nih.gov/pubmed/21592453
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
31 year-old male with recently diagnosed hypertension presents with rapid lip swelling. He started taking an unknown medication for his hypertension last week. Further history reveals that he has had prior, although milder, episodes previously. Name two medications that may help treat him.

Answer: The patient has hereditary angioedema with an episode triggered by an ACE inhibitor. Treatment includes the usual cocktail of histamine blockers and steroids plus:
The precipitant cause is unknown in most cases, but common etiologies include drugs (e.g. ACE inhibitors), infections, dental work, or stress.
Serum C4 level may assist in the diagnosis, but are rarely helpful acutely.
Fifty percent of patients will have laryngeal swelling at one point in their lives and asphyxiation is the leading cause of death; mortality is ~14-33%
The airway must be emergently evaluated to determine the need for intubation. If required, the most skilled person should take the first look.
If access to the oropharynx is limited (secondary to lip and tongue swelling) fiberoptic nasolaryngoscopy may be considered however, always be prepared to perform an emergent surgical airway.
Bonus Pearl: Check out this months V-Cast hosted by Dr. Amal Mattu. Dr. Jim Roberts (of Roberts and Hedges fame) reviews angioedema. Check out this great review here: http://cmedownload.com/lecture/angioedema-v-cast
References
Joseph J. Moellman, and Jonathan A. Bernstein. Diagnosis and Management of Hereditary Angioedema: An Emergency Medicine Perspective. Journal of Emergency Medicine 2012 http://www.jem-journal.com/article/S0736-4679(11)01116-4/abstract
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/24/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
52 year-old male with diabetes complains of severe left foot pain for one month and now inability to ambulate. Vital signs are normal and X-rays are shown below. What's the diagnosis and why should you get a biopsy early?

Answer: Osteomyelitis and a bone biopsy (with culture) should be obtained early and before starting antibiotics.
Osteomyelitis is inflammation of a bone secondary to an infecting organism.
Risk factors include:
Causative bacteria typically include S. Aureus, Pseudomonas, Salmonella (classically with Sickle cell)
Diagnosis
Early and long-term antibiotic treatment (4-6 weeks) is required, but should be done AFTER obtaining bone biopsy and culture; long-term antibiotics are the rule and the most narrow spectrum antibiotic should be determined.
Operative management is sometimes required; especially if secondary to infected prosthetics.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 12/18/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Management of patients with severe traumatic brain injury (TBI) typically involves the use of invasive intra-parenchymal pressure monitors. Although use of these monitors is recommended by TBI management guidelines, good quality evidence of benefit is lacking.
A recently published study evaluated the outcomes of TBI patients using a management protocol incorporating either an intracranial pressure (ICP) monitor compared to use of the clinical exam PLUS serial neuroimaging; a total of 324 patients were prospectively randomized into either group.
The primary study outcome was a composite of survival, impaired consciousness, and functional status at both three and six months.
The results of the study did not show a significant difference in the:
Bottom line: This study suggests that clinical exam PLUS serial neuroimaging may perform as well as invasive intra-parenchymal monitors for guiding therapy in TBI patients.
Chestnut, R. et al. A Trial of Intracranial-Pressure Monitoring in Traumatic Brain Injury. NEJM 2012 Dec 12. http://www.ncbi.nlm.nih.gov/pubmed/23234472
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
50 year-old man with presents with acute-onset sharp left-sided chest pain and dyspnea. What's the diagnosis and the name of the abnormality on chest x-ray?
Answer: Pulmonary embolism with CXR demonstrating "Hampton Hump".
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/10/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
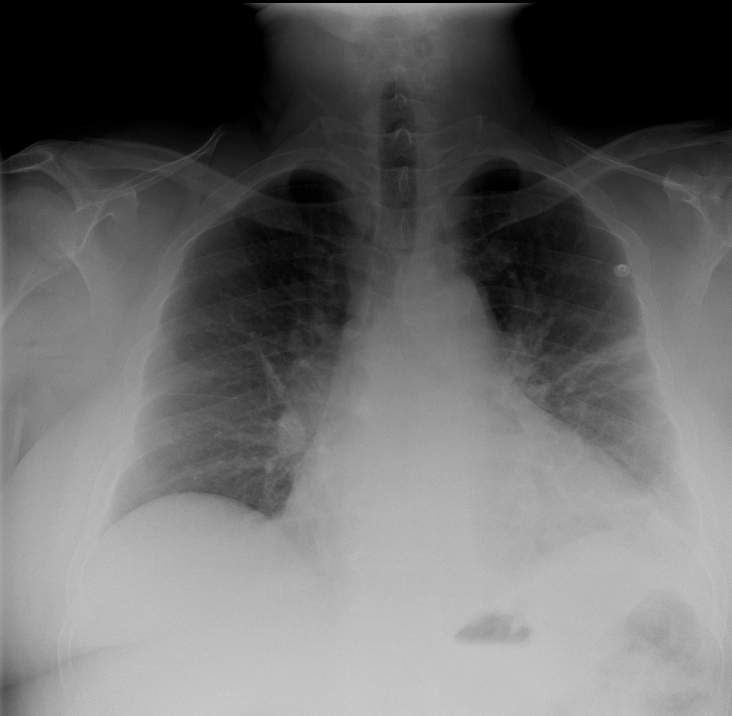
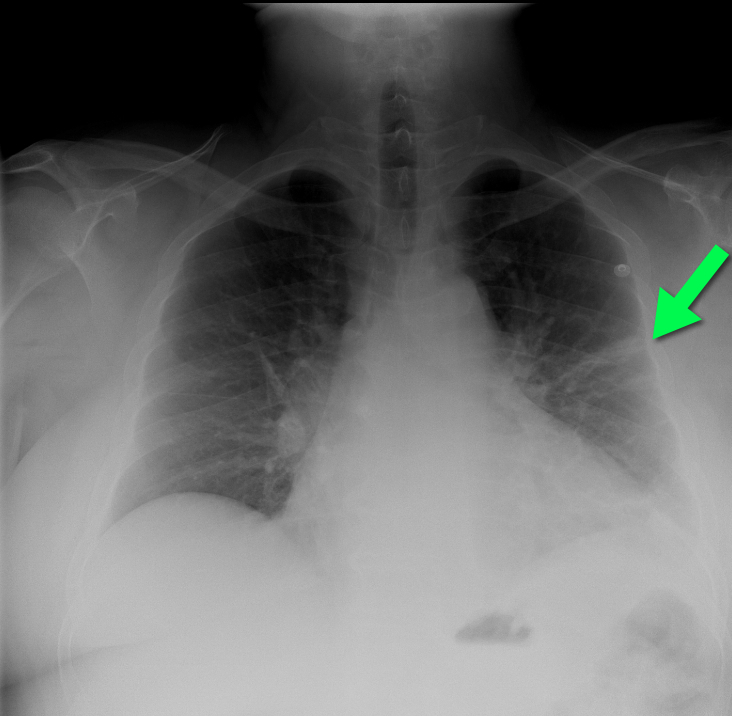
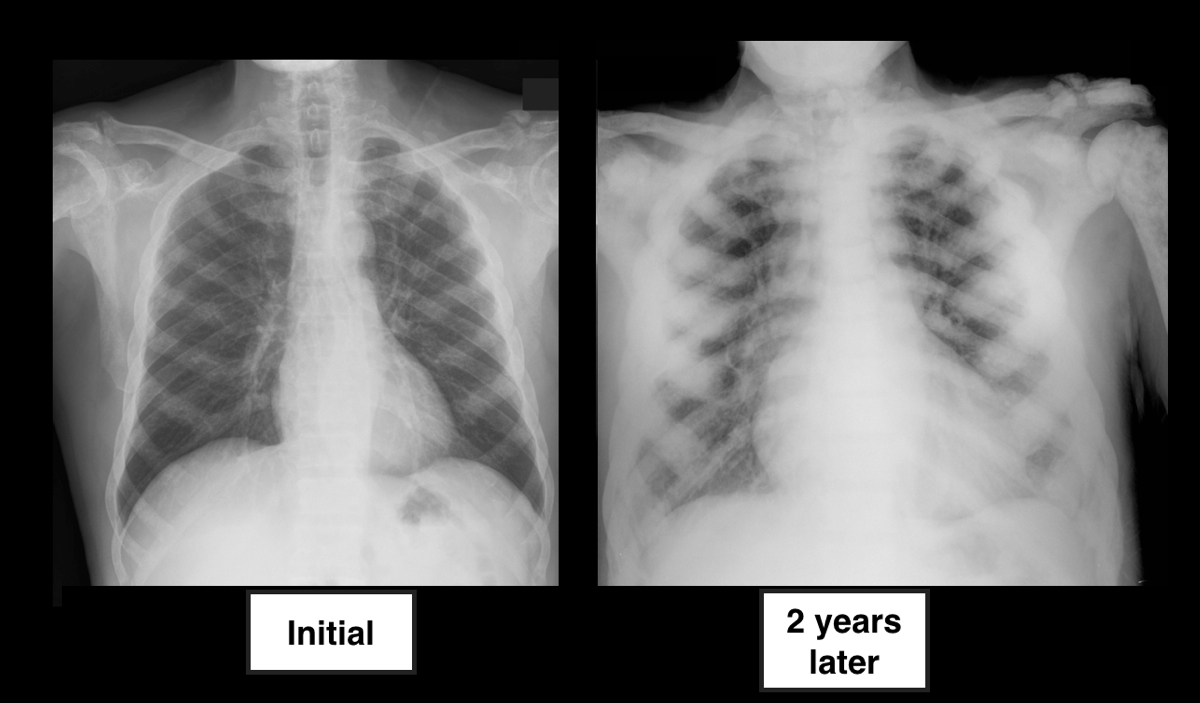
64 year-old male with no past medical history presents complaining of chronic weight-loss and diffuse chest pain; CXR is shown below. What's the diagnosis, and what other disease(s) may present this way?

Answer: Sclerotic bone (osteoblastic) metastasis secondary to prostate cancer. The patient's CXR from 2 years prior is shown below for comparison.
Other malignancies associated with osteoblastic metastasis:
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/4/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
An 86 year-old nursing home resident presents to the ED with a urinary tract infection, four days after discharge from the inpatient service for the same diagnosis. She was discharged from the inpatient service with a prescription for ciprofloxacin to be given through her gastric feeding tube (she does not take anything orally). Could her tube feeds be playing a role in the relapse of her urinary tract infection?
Answer: Ciprofloxacin was not being properly absorbed secondary to enteral tube feeding.
Fluoroquinolones administered via enteral feeding tubes may have reduced efficacy and patient outcomes when given to patients simultaneously receiving tube feeds (e.g., PEG tube feeding).
The reduction in antimicrobial efficacy may be due to improper peak drug concentrations and variability in time to peak serum levels. Studies have demonstrated the bioavailability of Ciprofloxacin varies from 31-82% in patients receiving continuous enteral feeds.
The exact mechanism(s) responsible for the altered pharmokinetics are not completely understood but may involve the binding of divalent cations in the enteral feeds by fluoroquinolones, reducing its absorption and efficacy.
Clinicians should properly educate people who will be administering fluoroquinolones to the patient (e.g., nursing home staff, family, etc.). It is recommended that fluoroquinolones be given:
Perhaps easiest of all, is to consider discharging patients with a prescription for parenterally administered antibiotics for the duration of the infection.
Beckwith MF, Feddema SS, Barton RG, Graves C. A guide to drug therapy in patients with enteral feeding tubes: Dosage form selection and administration methods. Hosp Pharm. 2004;39:225–37
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/2/2012 by Haney Mallemat, MD
(Updated: 12/3/2012)
Click here to contact Haney Mallemat, MD
11 year-old boy presents with right knee pain and swelling after falling off of his bicycle. What's the diagnosis?
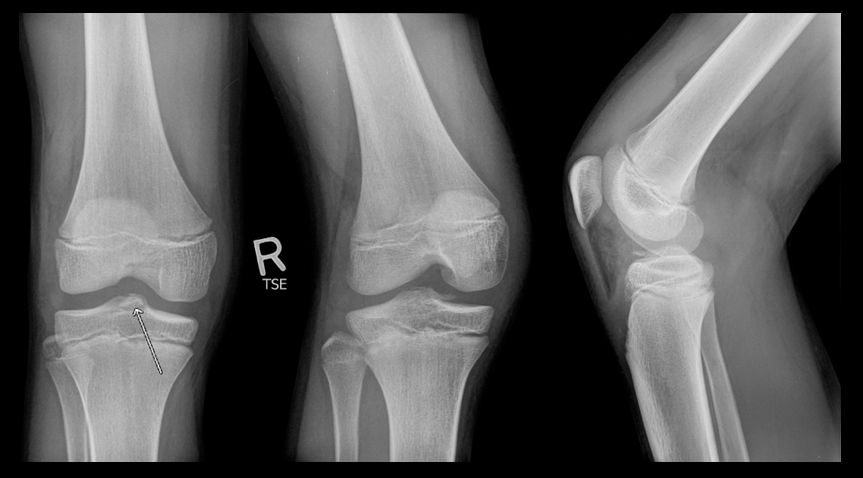
Answer: Fracture of the intercondylar eminence of the tibia; Meyers & McKeever Grade II (grading system described below)
Intercondylar Eminence Fracture
Reference: Tudisco, C., et al Intercondylar eminence avulsion fracture in children: long-term follow-up of 14 cases at the end of skeletal growth, J Pediatr Orthop B 19:403–408 c 2010
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/25/2012 by Haney Mallemat, MD
(Updated: 11/26/2012)
Click here to contact Haney Mallemat, MD
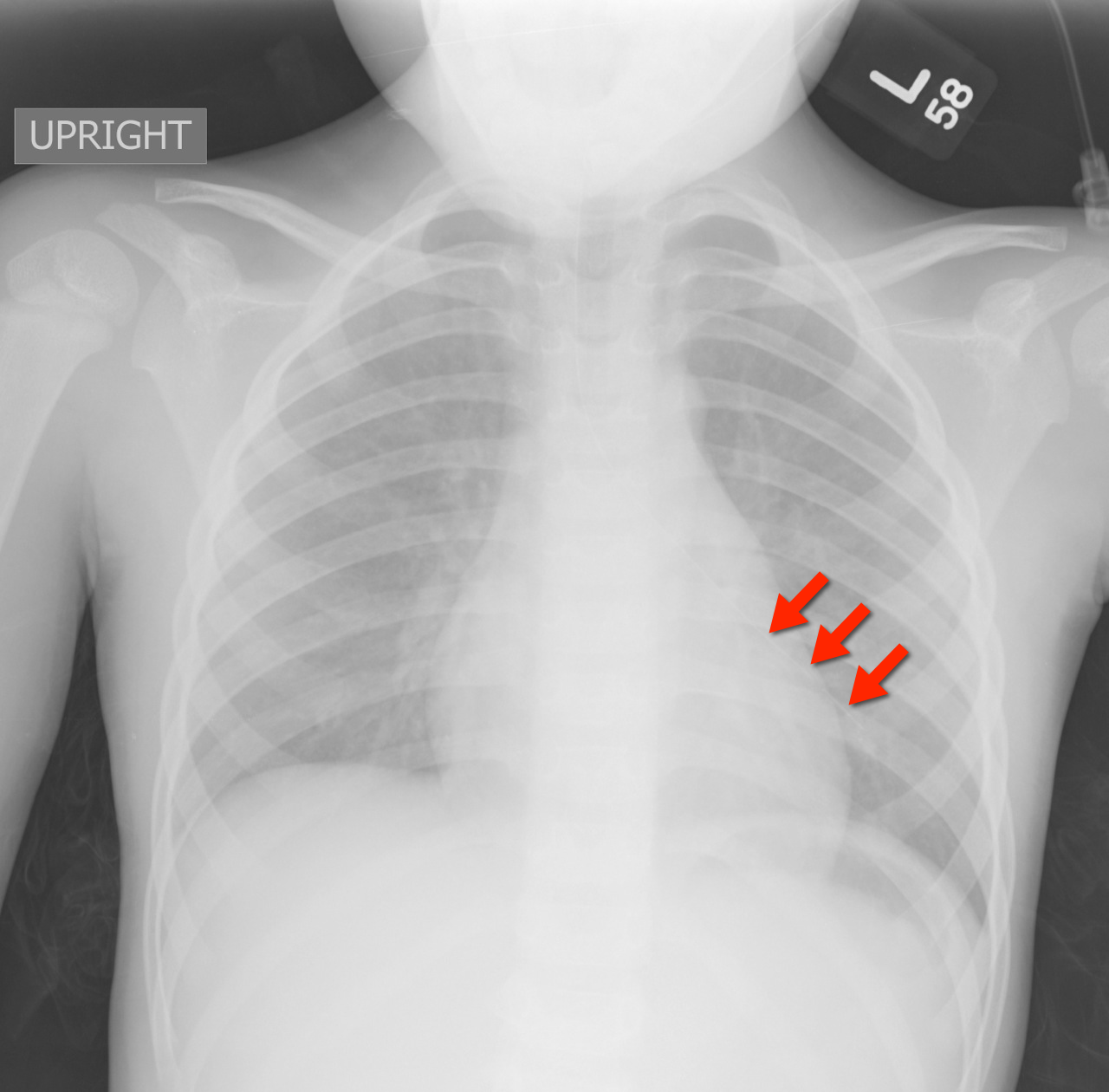
2 year-old male with past medical history of asthma presents with fever and respiratory distress. CXR is shown below. What’s the diagnosis? (Hint: ...look beyond the obvious)

Answer #1: Multifocal opacities predominantly in left lower lobe representing pneumonia
Answer #2 Healing left-sided rib fractures involving the lateral aspects of ribs 8 through 10th suspicious for non-accidental trauma (see X-ray below)
Pediatric CXR pearls
Bottom line: Screen patients for the above risk factors when rib fractures have been identified, but always think of abuse and the child’s safety first….and don’t forget to thoroughly examine radiology despite finding one abnormal finding.

Reference: Cosway et al. Diagnostic indicators for NAI in children with rib fractures: A retrospective study. Arch Dis Child 2011; 96 (supplement)
Follow me on Twitter (@criticalcarenow) or Google+ (+Haney Mallemat)
Category: Critical Care
Posted: 11/20/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A low-tidal volume (or protective) strategy of mechanical ventilation (i.e., tidal volume of 6-8cc/kg of ideal body weight) has previously been demonstrated to be beneficial in patients with acute respiratory distress syndrome (ARDS).
A meta-analysis was recently performed to determine whether this strategy of mechanical ventilation is also beneficial for patients without lung injury prior to initiation of mechanical ventilation.
Dr. Neto, et al. performed a meta-analysis of 20 studies (total of 2,822 mechanically ventilated patients) comparing a conventional ventilation strategy (average tidal volume was 10.6 cc/kg) to a protective ventilation strategy (average tidal volume was 6.4 cc/kg) of mechanical ventilation.
The authors concluded that patients ventilated with a protective lung-strategy had reductions in:
Bottom-line: This meta-analysis supports the notion that a strategy of low-tidal volume ventilation may have benefits for patients without ARDS, however prospective studies are needed.
Neto, S. et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome. JAMA, Oct. 24/31; 308;16.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
