Category: Visual Diagnosis
Posted: 1/13/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
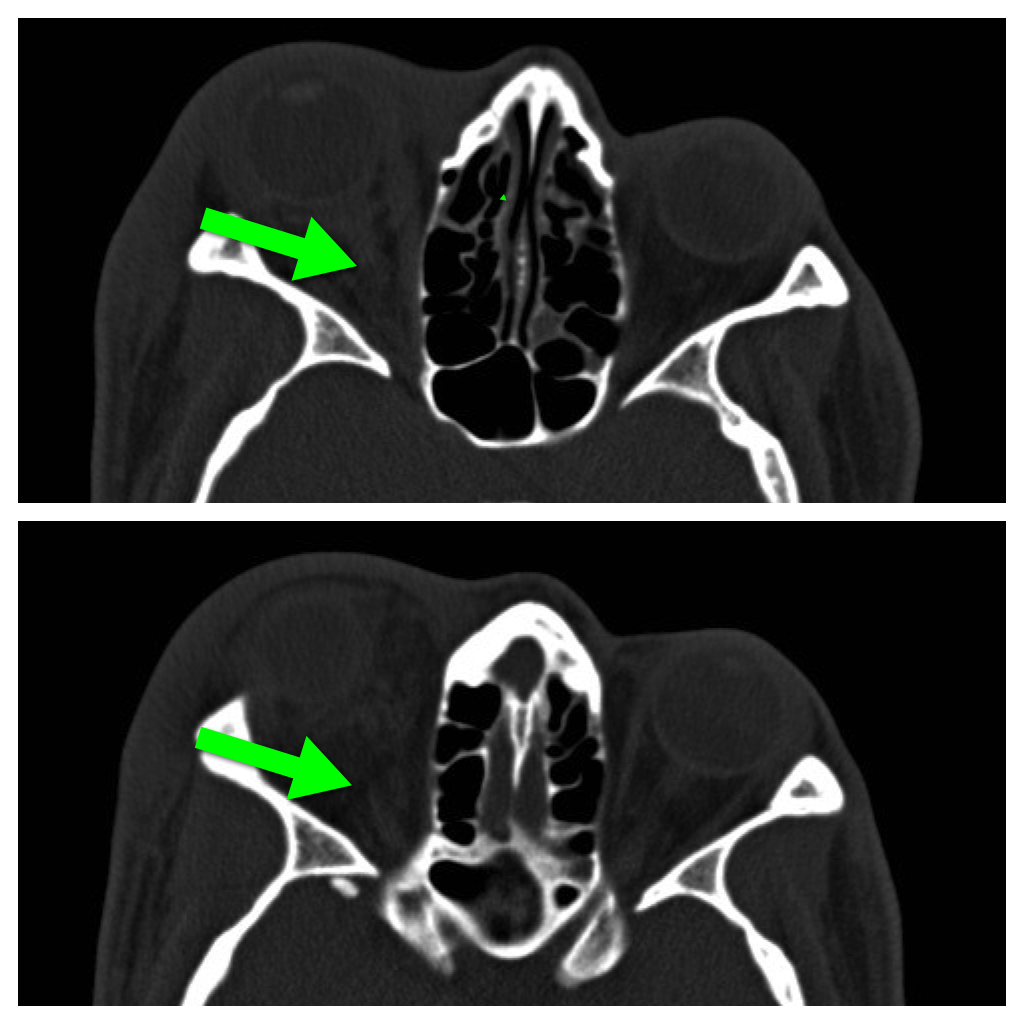
42 year-old male s/p assault complains of right sided facial pain, swelling, and decreased vision. Physical exam reveals subconjunctival hemorrhage, proptosis, afferent pupillary defect, and a firm globe. What's the diagnosis and what's the emergent treatment?

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/6/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
37 year-old male presents after sustaining a burn from a pot of boiling water. He states that his skin started to blister a few hours after and it’s quite painful. What type of burn does he likely have?

A non-circumferential, superficial partial-thickness burn; it was treated with Silvadene (silver sulfadiazine)
Burn Classification:

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine). New York: McGraw-Hill Companies. pp. 1374–1386.
Category: Visual Diagnosis
Posted: 12/30/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
68 year-old male presents with weakness after surgical repair of his abdominal aorta. What’s the diagnosis and name at least one eponym for the signs displayed (there are five total)?
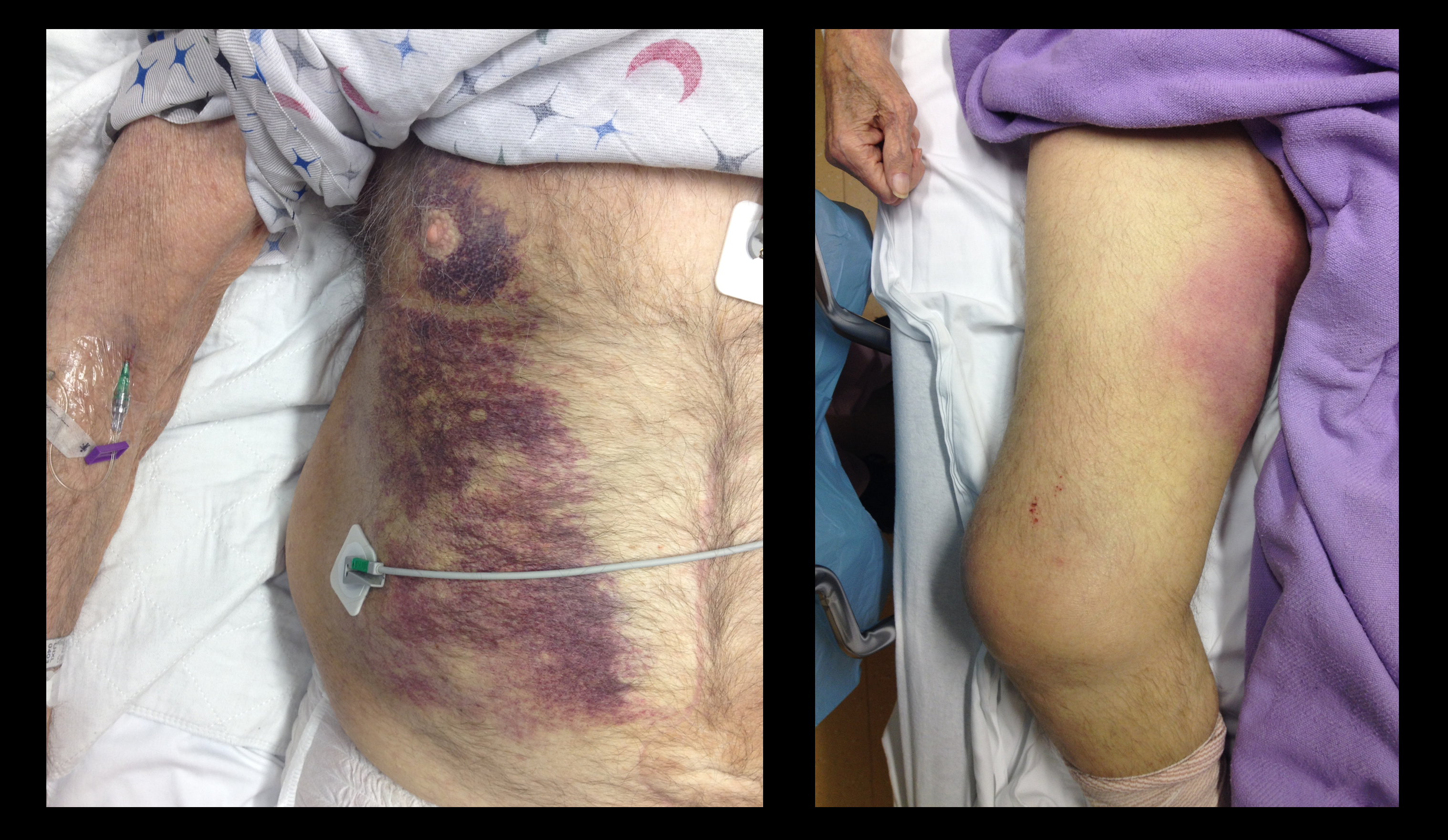
Grey-Turner and Fox's sign; these signs indicate retroperitoneal hemorrhage.

There are five signs suggesting retroperitoneal bleeding. They generally appear 24 hours after bleeding starts, occurring when blood extravasates along ligamentous connections between the retroperitoneal space and skin surface.
1. Grey-Turner Sign: Named for the surgeon who identified it in 1920; a bluish hematoma across the lateral abdominal wall when blood from the pararenal space leaks along the quadratus lumborum.
2. Fox’s Sign: Described by Dr. Fox in 1966 in two patients, (ruptured AAA and pancreatitis); ecchymosis over anteromedial thigh secondary to blood seeping along the fascia of psoas and iliacus.
3. Cullen’s Sign: Dr. Cullen (gynecologist), described this in 1918 as a sign of a ruptured ectopic pregnancy; bruise around the umbilicus from retroperitoneal blood tracking along falciform ligament.
4. Bryant’s Sign: Dr. Bryant initially described this sign; ecchymosis of the scrotum from blood tracking down the spermatic cord.
5. Stabler’s sign: Ecchymosis over the inguinal ligament
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 12/24/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The morbidity and mortality from pseudomonas aeruginosa infections is high and empiric double-antibiotic coverage (DAC) is sometimes given; quality evidence for this practice is lacking.
Although there is little supporting data, the following reasons have been given for DAC:
The potential harm of antibiotic overuse cannot be ignored, however, and include adverse reaction, microbial resistance, risk of super-infection with other organisms (e.g., Clostridium difficile), and cost.
There may be a signal in the literature demonstrating a survival benefit when using DAC for patients with shock, hospital-associated pneumonia, or neutropenia. The IDSA guidelines, however, do not support DAC for neutropenia alone; only with neutropenia plus pneumonia or gram-negative bacteremia.
Bottom line: Little data supports the routine use of DAC in presumed pseudomonal infection. It may be considered in patients with shock, hospital-associated pneumonia, or neutropenia (+/- pneumonia), but consult your hospital’s antibiogram or ID consultant for local practices.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/23/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient with a history of osteogenesis imperfecta presents with right lateral chest pain following a sneeze. The ultrasound of his chest is shown (hint: arrow points to a rib). What's the diagnosis?
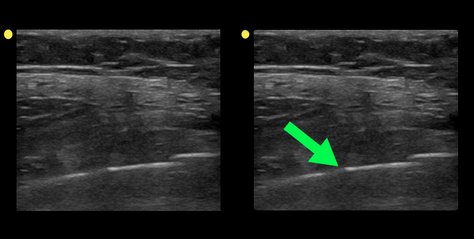
Rib fracture
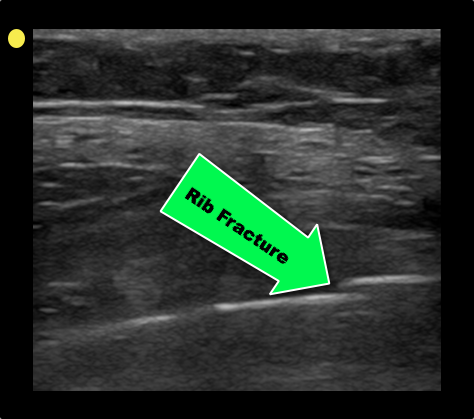
Turk F. et al. Evaluation by ultrasound of traumatic rib fractures missed by radiography. Emerg Radiol. 2010 Nov;17(6):473-7. doi: 10.1007/s10140-010-0892-9
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/16/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
46 year-old female found unresponsive at a party. EMS transports the patient in cardiac arrest. A parasternal-long axis view of the heart is obtained during the pulse check. What's the diagnosis?
Hemopericardium
The heterogeneous appearance of the pericardial fluid indicates that is likely a complex pericardial effusion; the fluid could be blood, pus, or a malignant effusion.
Differential diagnosis of hemopericardium includes:
Based on this initial ECHO, a pericardiocentesis was performed and blood was aspirated.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/9/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
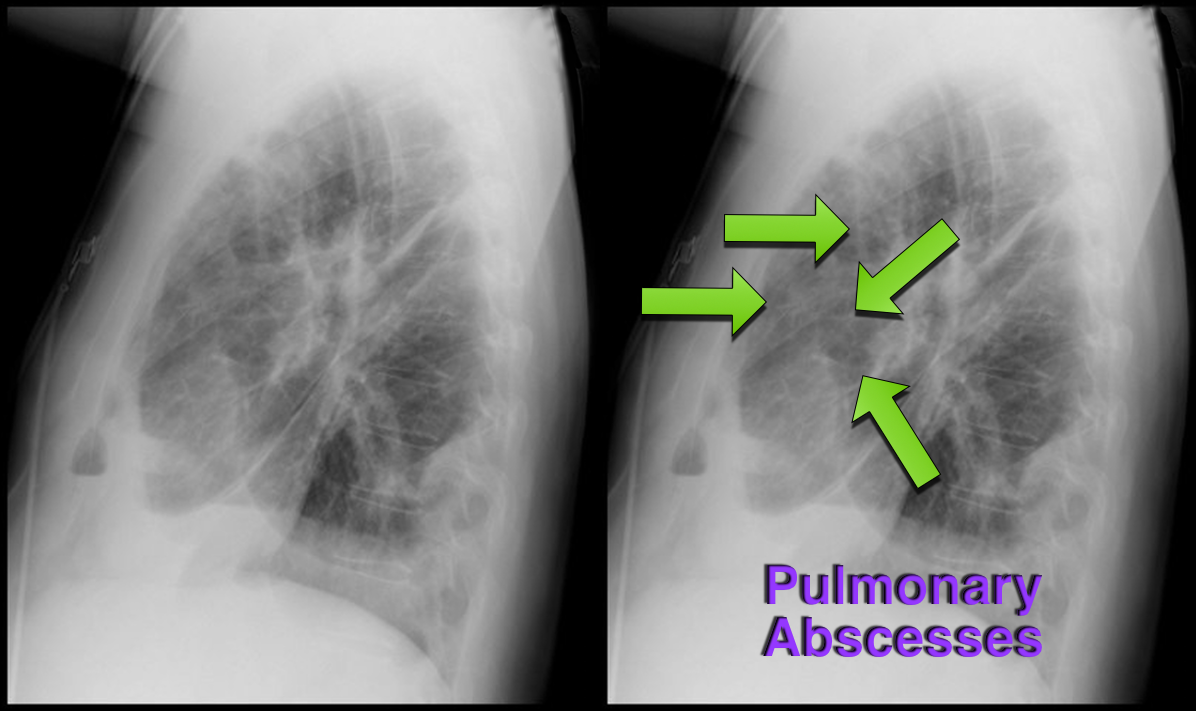
37 year-old male presents with cough and a fever. What's the diagnosis and name three risk factors assiciated with disease?

Answer: Lung Abscesses
Lung Abscess
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/2/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Which view of the heart is this and can you name the structures from A-G?
1. Subcostal or Subxiphoid view; this view is obtained by placing the probe under the ribs with the patient supine. The liver is used as an acoutic window to image the heart.
2. Name the items labeled A-G:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 11/26/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The management of alcohol withdrawal syndrome (AWS) includes supportive care focusing on the ABC’s and administration of benzodiazepines (BDZ).
While BDZ are effective in the treatment of AWS, some patients may require very high doses of BDZ to control symptoms (tachycardia, hypertension, diaphoresis, etc.); unfortunately, high-doses of BDZ may lead to suppression of the respiratory drive and endotracheal intubation.
Dexmedetomidine (DEX) is a sedative agent that is an intravenous alpha2-agonist (it's like clonidine); it reduces sympathetic outflow from the central nervous system and it may help treat withdrawal syndromes. The major benefit of DEX is that it does not suppress the respiratory drive, thus intubation is not required.
Smaller trials and case series have shown that patients with AWS who were treated with BDZ in addition to DEX had better symptom control, lower overall BDZ doses, and less respiratory depression/intubation.
Bottom-line: While more trials are needed, consider adding DEX for patients with AWS who require high-doses of BDZ.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/25/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
What view of the heart is this and can you name everything from A-G?
1. Apical-four chamber view; this view is obtained by placing the probe in the 4-5th intercostal space at the anterior axillary-line. The patient can be placed in left lateral decubitus to improve imaging.
2. Name the items labeled A-G:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
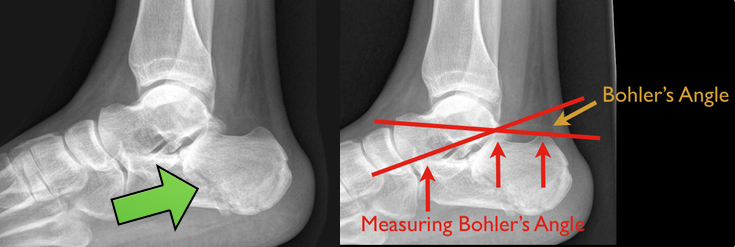
48 year-old presents after falling 15 feet following a “misunderstanding” with police. What's the diagnosis? ...and for a bonus question, why is this called a “Lover’s Fracture”?

Calcaneus fracture
Answer to Bonus Question: Historically called a “Lover’s Fracture” for “lovers” jumping out of bedroom windows (to evade suspicious spouses) who then land directly on their feet.
Calcaneus fractures
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/11/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
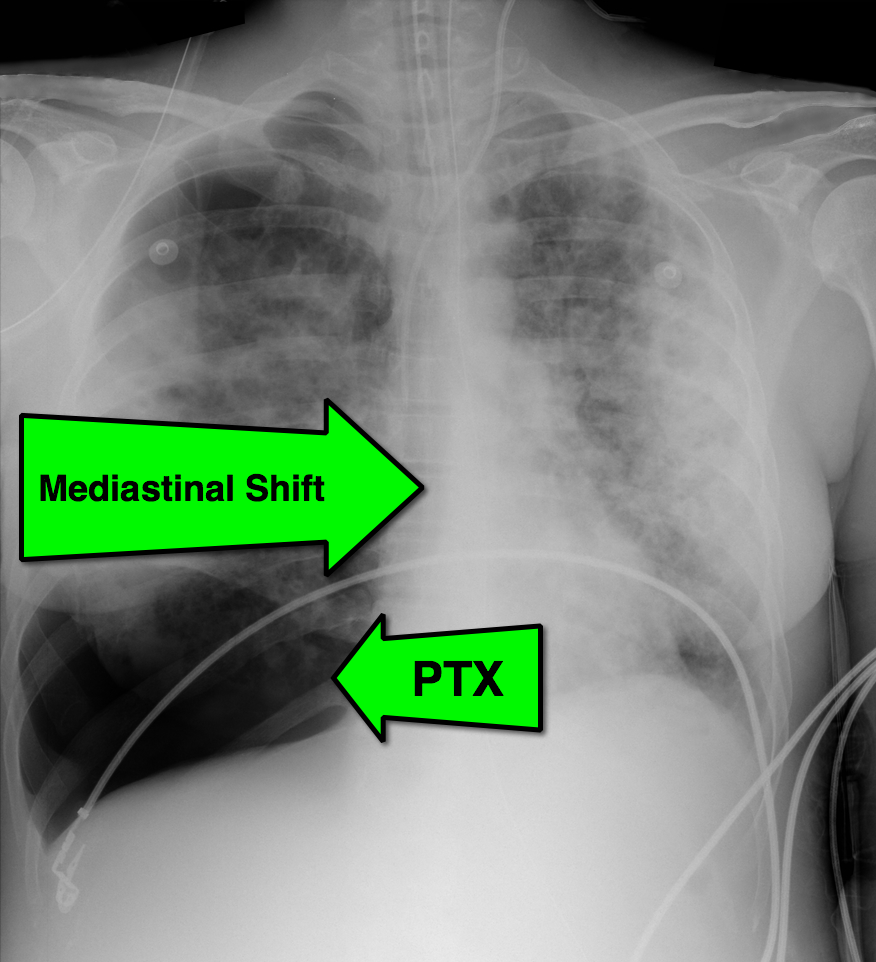
28 year-old cachectic female presents in respiratory distress and is immediately intubated on arrival to Emergency Department. What's the diagnosis and what are some potential etiologies?

Pneumothorax with mediastinal shift
Differential Diagnosis
The patient in this case had undiagnosed HIV/AIDS and presented with PTX secondary to PJP. The lifetime risk of PTX with HIV is 6% and 85% of those cases are secondary to PJP.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
This week's visual pearl reviews the structures of the heart when being viewed in a parasternal long-axis view. What do the labels correspond to in the clip below (note: "E" and "F" are valves) and do you see any obvious abnormalities?
The parasternal long-axis is obtained by scanning to the left (patient's left) of the sternum through the 2nd-5th intercostal space. Click here for a tutorial on the technique.
Answer to Bonus Question: Dilation of the RVOT
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 10/29/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The pregnant patient normally has increased cardiac output and minute ventilation by the third trimester. Despite this increase, however, these patients have little cardiopulmonary reserve should they become critically-ill.
Remember the mnemonic T.O.L.D.D. for simple tips that should be done for the pregnant patient who presents critically-ill or with the potential for critical illness:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/27/2013 by Haney Mallemat, MD
(Updated: 10/28/2013)
Click here to contact Haney Mallemat, MD
15 year-old right-hand dominant male received a direct blow to the right arm with a hockey stick. What’s the diagnosis?

Monteggia Fracture
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/20/2013 by Haney Mallemat, MD
(Updated: 12/5/2023)
Click here to contact Haney Mallemat, MD
55 year-old male presents with chest pain. You take a look at his cardiac function with ultrasound and here's the patient's apical four-chamber view. What's in his right ventricle and why would it be there?
AICD
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 10/16/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There have been so many great talks at ACEP 2013, but Dr. Michael Winters' talk "The ICU is NOT Ready for Your Patient" was chock full of great critical care pearls. Here are just a few:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/14/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A 23 year-old male presents with the rash below. He originally presented to his primary care doctor for a sore throat and was given a prescription for a medication; this rash subsequently broke out. What's the diagnosis and which medication did he receive?
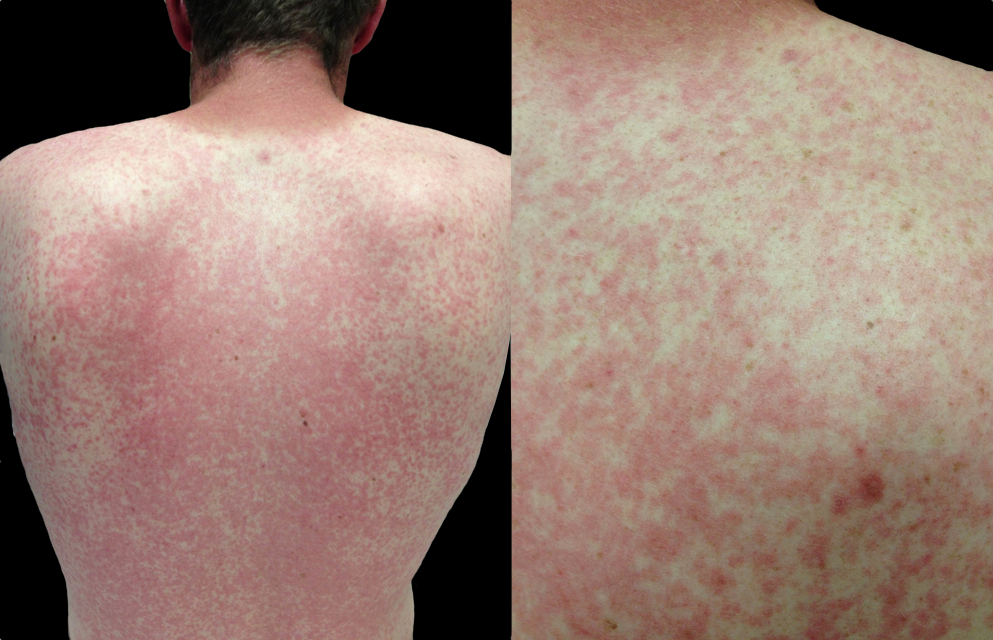
Rash secondary to Epstein-Barr pharyngitis treated with amoxicillin
Luzuriaga, K., Sullivan, J. Infectious Mononucleosis. N Engl J Med 2010; 362:1993-2000
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old female struck in the left hand by a football. Presents with pain, visible deformity, and the Xray below. What are the next step(s) in management?

Dorsal Metacarpophalangeal (MCP) Dislocation

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 9/30/2013 by Haney Mallemat, MD
(Updated: 10/1/2013)
Click here to contact Haney Mallemat, MD
The efficacy of epinephrine during out-of hospital cardiac arrest has been questioned in recent years, especially with respect to neurologic outcomes (ref#1).
A recent study demonstrated both a survival and neurologic benefit to using epinephrine during in-hospital cardiac arrest when used in combination with vasopressin and methylprednisolone.
Researchers in Greece randomized 268 consecutive patients with in-hospital cardiac arrest to receive either epinephrine + placebo (control group; n=138) or vasopressin, epinephrine, and methylprednisolone (intervention arm; n=130)
Vasopressin (20 IU) was given with epinephrine each CPR cycle for the first 5 cycles; Epinephrine was given alone thereafter (if necessary)
Methylprednisolone (40 mg) was only given during the first CPR cycle.
If there was return of spontaneous circulation (ROSC) but the patient was in shock, 300 mg of methylprednisolone was given daily for up to 7 days.
Primary study end-points were ROSC for 20 minutes or more and survival to hospital discharge while monitoring for neurological outcome
The results were that patients in the intervention group had a statistically significant:
probability of ROSC for > 20 minutes (84% vs. 66%)
survival with good neurological outcomes (14% vs. 5%)
survival if shock was present post-ROSC (21% vs. 8%)
better hemodynamic parameters, less organ dysfunction, and better central venous saturation levels
Bottom-line: This study may present a promising new therapy for in-hospital cardiac arrest and should be strongly considered.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
