Category: International EM
Posted: 6/4/2014 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
This year there have been over 280 cases of measles in the US, spanning 18 states; early recognition is key to preventing transmission.
Remember the 3 c's for recognition:
Cough, Coryza (runny nose), Conjunctivitis + febrile rash
-Incubation period is 10-12 days
-Symptoms usually start with fever, followed by rash 2-3 days later starting from the hairline and spreading to the trunk and extremities
-Completion of the first series of vaccines provides 90-95% immunity from measles
Relevance to the EM Physician:
-Immediately place any patient suspected of having measles on airborne precautions
-Look for koplik spots on the oral mucosa (commonly described as appearing like small grains of salt)
-Complications include diarrhea, otitis media, “measles croup,” pneumonia, encephalitis (1/1000 cases), and death (2-3/1000 cases)
-Post exposure prophylaxis (PEP) is recommended for unvaccinated exposed individuals and is effective up to 72 hours after exposure; however, vaccination is contraindicated in pregnant women
Bottom Line:
-The incidence of measles is rising sharply in the US. Vaccination, early detection, and post exposure prophylaxis for exposed individuals is key to reversing this trend.
University of Maryland Section of Global Emergency Health
Author: Bradford Schwartz, MD
1. CDC. Measles-January 1-May 23, 2014. MMWR 2014; 63;(1-4).
2. CDC. Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2013;62(RR04);1-34.
3. CDC. Measles Questions and answers. http://www.immunize.org/catg.d/p4209.pdf
4. CDC. Measles-Rubeola. http://www.cdc.gov/measles/index.html
5. Perry and Halsey. Clinical Significance of Measles: A Review. J Infect Dis. 2004 May 1;189 Suppl 1:S4-16.
Category: International EM
Posted: 9/18/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
· The coming of the Affordable Care Act (ACA) is designed to shift patient care from episodic encounters to continuous community based partnerships.
· Elsewhere in the world, community health workers (CHWs) have been used effectively to improve health outcomes, reduce heath care costs and create jobs in infectious disease (TB, HIV), maternal child health and chronic disease management.
· CHWs are paid, full time lay provider members of community health systems.
o Sub-Saharan Africa is training, deploying and integrating one million CHWs into the health system via a targeted campaign.
o Brazil’s CHWs are part of family health teams that care for 110 million people.
o India employs 600,000 CHWs paid through a fee-for-service system for primary care functions.
· CHWs cost less, reduce readmissions and help address root causes of preventable chronic disease while remaining embedded in the community helping to strengthen long-term community relationships.
Relevance to the EM Physician:
As frustration with non-compliant patients mounts and the impact of the ACA looms, CHWs integrated into American communities may be just the answer we haven’t yet considered to help reduce ED overcrowding and improve our patients’ outcomes.
University of Maryland Section of Global Emergency Health
Author: Emilie J.B. Calvello, MD, MPH
Singh,P. Chokshi, D. Community Health Workers – A Local Solution to a Global Problem. NEJM. 2013, 369: 894 – 896.
Category: International EM
Posted: 8/21/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
·You must know the diagnosis to deliver effective and high quality care to patients; likewise for health systems to be effective, it is necessary to understand what the global burden of disease is.
·In 1991, the World Bank and World Health Organization launched the Global Burden of Disease Study which as of 2010 evaluates 291 disease and injuries as well as 1160 sequelae of these causes.
·In order to compare the burden of one disease with that of another, you must consider death and life expectancy of persons affected by the disease as well as disability imposed by the condition.
·The combined composite summary metric is termed disability adjusted life years (DALYs).
·There have been three major worldwide studies to date (1990, 2005, 2010) attempting to quantify the burden of disease yet no study to date has ever attempted to quantify the burden of disease requiring emergent intervention.
Bottom Line:
DALYs are a useful tool for quantifying the burden of disease and provides essential input into health policy dialogues to identifies conditions and risk factors that may be relatively neglected and others for which progress is not what was expected. To date, there has been no rigorous scientific effort to quantify the burden of disease worldwide that requires emergent intervention to avoid death and disability.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
Christopher J.L. Murray, M.D., D.Phil., and Alan D. Lopez, Ph.D. Measuring the Global Burden of Disease. N Engl J Med 2013; 369:448-45
Category: International EM
Posted: 8/8/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
·You must know the diagnosis to deliver effective and high quality care to patients; likewise for health systems to be effective, it is necessary to understand what the global burden of disease is.
·In 1991, the World Bank and World Health Organization launched the Global Burden of Disease Study which as of 2010 evaluates 291 disease and injuries as well as 1160 sequelae of these causes.
·In order to compare the burden of one disease with that of another, you must consider death and life expectancy of persons affected by the disease as well as disability imposed by the condition.
·The combined composite summary metric is termed disability adjusted life years (DALYs).
·There have been three major worldwide studies to date (1990, 2005, 2010) attempting to quantify the burden of disease yet no study to date has ever attempted to quantify the burden of disease requiring emergent intervention.
Bottom Line:
DALYs are a useful tool for quantifying the burden of disease and provides essential input into health policy dialogues to identifies conditions and risk factors that may be relatively neglected and others for which progress is not what was expected. To date, there has been no rigorous scientific effort to quantify the burden of disease worldwide that requires emergent intervention to avoid death and disability.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
Christopher J.L. Murray, M.D., D.Phil., and Alan D. Lopez, Ph.D. Measuring the Global Burden of Disease. N Engl J Med 2013; 369:448-45
Category: International EM
Posted: 7/24/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
· Caused by the ameboflagellate Naegleria Fowleri
· Case fatality rate is estimated at 98%
· Commonly found in warm freshwater environments such as hot springs, lakes, natural mineral water, especially during hot summer months
· Incubation period 2-15 days
Relevance to the EM Physician:
· Clinical presentation: resembling bacterial meningitis/encephalitis
· Final diagnostic confirmation is not achieved until trophozoites are isolated and identified from CSF or brain tissue
· Treatment: Amphotericin B
Bottom Line:
· History of travel to tropical areas or exposure to warm or under-chlorinated water during summer time should raise the suspicion for Naegleria Fowleri. The amoeba is not sensitive to the standard meningitis/encephalitis therapy and amphotericin B must be added to the treatment regimen.
University of Maryland Section of Global Emergency Health
Su MY, Lee MS, Shyu LY, Lin WC, Hsiao PC, Wang CP, Ji DD, Chen KM, Lai SC. A fatal case of Naegleria fowleri meningoencephalitis in Taiwan. Korean J Parasitol. 2013 Apr
Naegleria fowleri, Kelly Fero , ParaSite, February 2010 retrieved from http://www.stanford.edu/group/parasites/ParaSites2010/Katherine_Fero/FeroNaegleriafowleri.htm
Category: International EM
Posted: 5/30/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Background Information:
Each year, an estimated 50 million travelers from Western countries visit tropical regions all over the world.
Given the potentially serious consequences for the patients and, their close contacts and healthcare workers it is important that life threatening tropical diseases are swiftly diagnosed.
Pertinent Study Design and Conclusions:
- Descriptive analysis of acute and potentially life threatening tropical diseases among 82,825 ill western travelers reported to GeoSentinel from June of 1996 to August of 2011.
- Of these travelers, 3,655 (4.4%) patients had an acute and potentially life threatening disease.
- The four most common conditions being falciparum malaria (76.9%), typhoid fever (11.7%), paratyphoid fever (6.4%), and leptospirosis (2.4%).
Bottom Line:
Western physicians seeing febrile and recently returned travelers from the tropics need to consider a wide profile of potentially life threatening tropical illnesses, with a specific focus on the most likely diseases described in this case series.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
Jensenius M, Han PV, Schlagenhauf P, Schwartz E, Parola P, Castelli F, von Sonnenburg F, Loutan L, Leder K, Freedman DO; GeoSentinel Surveillance Network. Acute and potentially life-threatening tropical diseases in western travelers—a GeoSentinel multicenter study, 1996-2011. Am J Trop Med Hyg. 2013 Feb; 88(2):397-404
Category: International EM
Posted: 5/22/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Clinical Presentation:
- A 40-year-old Hispanic man was admitted to the hospital after being found unconscious. He had a 2-day history of disorientation that manifested itself as his being unable to recognize family members.
- Upon admission he regained consciousness, becoming alert and oriented, but developed urinary retention and was unable to move or feel his lower extremities.
- Spinal MRI (with and without gadolinium) showed the spinal cord to be abnormally diffuse, with swelling and edema in the cervicothoracic region.
Diagnosis:
- After an extensive work up for lymphoma and CNS infection, he was discovered to have toxoplasmosis and was found to be HIV positive, which was previously undiagnosed.
Discussion:
- Approximately 10% of patients with AIDS present with some neurological deficit as their initial complaint, and up to 80% will have CNS involvement during the course of their disease.
- Myelitis is a known complication of AIDS and is occasionally the initial complaint.
The incidence of myelopathy may be as high as 20%, with 50% of the cases reported post-mortem
- Toxoplasmosis is the most common cause of cerebral mass lesions in patients with AIDS
Occurring in 3–10% of patients in the United States and in up to 50% of AIDS patients in Europe, Latin America, and Africa
Bottom Line:
New neurological deficit in any patient should raise suspicion of HIV infection
Most patients with AIDS that present with evolving myelopathy, characterized by extremity weakness, sensory involvement, spinal cord enlargement, enhancing lesions in brain or spinal cord CT or MRI, have toxoplasmic myelitis
University of Maryland Section of Global Emergency Health
Author: Terrence Mulligan DO, MPH
"Spinal cord toxoplasmosis as an unusual presentation of AIDS: case report and review of the literature", Int J Emerg Med (2010) 3:439–442
Category: International EM
Posted: 5/15/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General information:
· Salmonella typhi – transmission through fecal-oral, contaminated food, human carriers
· Most cases in the US acquired abroad – Africa, Latin American, Asia
· Vaccine available – not life-long immunity, need 1-2 weeks to take effect
Clinical Presentation:
· sustained high fever (103-104)
· Faget sign: fever and bradycardia (also seen in yellow fever, atypical pneumonia, tularemia, brucellosis, Colorado tick fever))
· Abdominal pain, GI bleed/perforation, hepatosplenomegaly, delirium
· “Rose spots” – erythematous macular rash over chest and abdomen
· Without treatment sx can resolve after 3-4 weeks, mortality from secondary infections 12-30%
Diagnosis:
· Pan-culture for S. typhi
· Serologic: Widal test (negative for 1st week of symptoms, 7-14 days to result)
Treatment:
· Abx: amoxicillin, trimethoprim-sulfamethoxazole, and ciprofloxacin
· MDR typhoid: ceftriaxone or Azithromycine 1st line
Bottom Line:
· Get vaccinated if travelling to endemic areas 1-2 weeks before travel
· Suspect in travelers to endemic areas with sustained high fevers
· Spontaneous resolution does occur but may become carriers without abx
Famous victims or Typhoid fever:
· Wilbur Wright (Wright brothers)
· Prince Albert (Queen Victoria’s husband)
· Hakaru Hashimoto (discovered Hashimoto’s thyroiditis)
· Abigail Adams (1st Lady, wife of John Adams)
University of Maryland Section of Global Emergency Health
Author: Veronica Pei, MD
http://www.cdc.gov/nczved/divisions/dfbmd/diseases/typhoid_fever/technical.html#risk
Category: International EM
Posted: 5/8/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Case Presentation:
A Spanish speaking man in his late 20s is brought in by ambulance for severe dyspnea. Given the language barrier and his clinical status you are unable to obtain any history. He is tachypnic, had a low pulse ox, and was placed on BiPAP. On exam you hear bibasilar rales and a faint holosystolic murmur.
Clinical Question:
What should be included in the differential?
Answer:
Rheumatic heart disease is the result of valvular damage due to an abnormal immune response following a group A streptococcal infection. It affects 15.6 to 19.6 million people worldwide. Most patients present with dyspnea between the ages 20-50. The most common valvular disease is mitral insufficiency, but it may present with mitral stenosis or aortic regurgitation. The disease is most prevalent in sub-Saharan Africa and among the Indigenous population of Australia but it can be found in many developing countries. People who live in rural areas without access to medical care are those at highest risk for developing rheumatic fever and subsequently rheumatic heart disease.
Bottom Line:
Rheumatic heart disease should be considered in patients who present from an endemic region.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD, MPH
Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet. 2012 Mar 10;379(9819):953-64. doi: 10.1016/S0140-6736(11)61171-9.
(Not really a reference but a short documentary nominated for an Oscar this year.)
Category: International EM
Posted: 4/17/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
A parasitic infection caused by the tissue-dwelling filarial nematode worm Wuchereria bancrofti; a wide range of mosquitoes transmit the infection. When the worm is mature, it inhabits lymph nodes and produces sheathed microfilarial larvae that circulate in the peripheral blood.
Clinical Presentation:
- Infection with the adult worms produces painless subcutaneous nodules that are usually less than 2 cm in diameter, typically over bony prominences.
- Symptoms depend on where the microfilariae migrate to, and vary accordingly. They include: pruritus, papular dermatitis, dermal atrophy and depigmentation or hyperreactive skin disease (Sowda), keratitis, iritis, chorioretinitis, optic atrophy and eventually blindness, orchitis, hydrocele, chyluria, elephantiasis, pulmonary eosinophilia, cough, wheezing, and splenomegaly.
Diagnosis:
- Peripheral blood smear taken between 11pm and 1am or after provocation using diethylcarbamazine (DEC).
- Filarial antigen test.
- Eosinophilia, and specific antiflarial IgG and IgE antibodies.
Treatment:
- DEC which must be obtained directly from the CDC.
- Alternatively Doxycycline. Both drugs are effective against both macro and micro-filaria.
Bottom Line:
One billion people globally are at risk for infection with filaria. 120 million already have the infection. Suspect the infection in patients that have been to Africa, Asia, especially India, Western pacific, Haiti, the Dominican Republic, Guyana and Brazil.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MD
James AG Whitworth. Filariasis. Medicine. 2005;33:61
Category: International EM
Posted: 4/3/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Spring is in the air... and so is rotavirus.
Area of the world affected:
· Diarrheal illnesses were responsible for 1.6 million deaths for children under 5 globally in 2002.
· This number has improved over the years, in part due to oral rehydration salts (ORS) which were developed for cholera.
Relevance to the US physician:
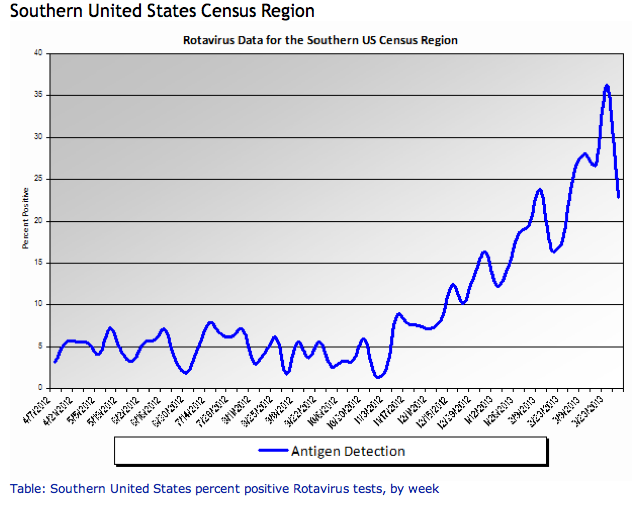
http://www.cdc.gov/surveillance/nrevss/rotavirus/region.html#top
· ORS are also important for rotavirus treatment and uncomplicated gastroenteritis in children and adults.
· Commercially prepared solutions have different concentrations of ingredients, but all will work as better treatment and rehydration than common household products like sports drinks and juice.
Bottom line:
Consider ORS in patients with uncomplicated acute gastroenteritis.
University of Maryland Section of Global Emergency Health
Author: Jennifer Reifel Saltzberg, MD, MPH
Atia AN, Buchman AL. Oral rehydration solutions in non-cholera diarrhea: a review. Am J Gastroenterol 2009;104(10):2596-604.
Sentongo, TA. The Use of Oral Rehydration Solutions in Children and Adults. Current Gastroenterology Reports 2004; 6:307–313.
Category: International EM
Posted: 3/28/2013 by Walid Hammad, MD, MBChB
(Updated: 2/1/2026)
Click here to contact Walid Hammad, MD, MBChB
Background Information:
Combination antiretroviral therapy (cART) reduces HIV-associated morbidities and mortalities but cannot cure infection. Recent literature has suggested that early initiation of cART with primary infection can lead to “functional cure” for HIV infected patients with suppressed viremia and delayed progression to clinical symptoms.
Pertinent Study Design and Conclusions:
- Researchers studied 14 patients whose treatment with combination antiretrovirals began soon after exposure to HIV. The patients' viral loads became undetectable within roughly 3 months, and treatment was interrupted after about 3 years.
- The patients were found to have very low viral loads and stable CD4-cell counts after several years without therapy. The researchers estimate that about 15% of those treated early could achieve similar results.
Bottom Line:
Have a high suspicion of acute anti-retroviral syndrome in the ED (fever, rash, pharyngitis, lymphadenopathy) and test properly (viral load NOT ELISA) to identify patients who may benefit from early, rapid initiation of cART.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
Sáez-Cirión A, Bacchus C, Hocqueloux L, Avettand-Fenoel V, Girault I, et al. (2013) Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. PLoS Pathog 9(3): e1003211.
Category: International EM
Posted: 3/13/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Case Presentation: A 31 yo Hispanic male presents to your emergency department with extensive facial abrasions and contusions from an assault 7-8 days ago, c/o difficulty swallowing for 1-2 days. He was seen at that time in a nearby emergency department for his abrasions and contusions.
Upon examination, you find him to be irritable and restless, diaphoretic, tachycardic, and with mild neck stiffness. Over the course of his stay in the ED, he develops generalized muscle rigidity, severe neck stiffness and opisthotonic posturing.
Clinical Question: What is the diagnosis? And what went wrong?
Answer: This is an early presentation of generalized tetanus.
Unfortunately, little evidence exists to support any particular therapeutic intervention in tetanus. There are only nine randomized trials reported in the literature over the past 30 years. The goals of treatment include:
. At risk populations:
o Elderly patients are substantially less likely than young individuals to have adequate immunity against tetanus.
o Immigrants from Mexico had a 67% non-protective anti-tetanus antibody (ATA) level.
o In a pilot study 86% of Korean immigrants did not have protective ATA levels
o Emergency physicians were less likely to adhere to the tetanus guidelines when admitting patients to the hospital.
· Halting the toxin production: wound management and antimicrobial therapy
o Metronidazole 500mg IV q 6-8 hrs or Penicillin-G 2-4M units IV q4-6 hrs for 7-10 days
· Neutralization of the unbound toxin
o Human Tetanus Immunoglobulin (HTIG): A dose of 3000 to 6000 units intramuscularly should be given ASAP
o Since tetanus is one of the few bacterial diseases that does NOT confer immunity following recovery from acute illness, all patients with tetanus should receive FULL active immunization immediately upon diagnosis
· Treatment of generalized tetanus: this is best performed in the ICU and includes:
o Early and aggressive airway management
o Control of muscle spasms
o Management of dysautonomia
o General supportive management
Bottom Line:
o EP’s consistently under-immunize for tetanus, especially in elderly and immigrant populations, who have a much higher risk of under-immunization.
o Better awareness of tetanus prophylaxis recommendations is necessary, and future tetanus prophylaxis recommendations may be more effective if they are also based on demographic risk factors.
o Emergency physicians must comply with immunization guidelines for injured patients to assure adequate protection from both tetanus and diphtheria.
University of Maryland Section of Global Emergency Health
Author: Terry Mulligan DO, MPH
Alagappan K, Rennie W, Kwiatkowski T, Falck J, Silverstone F, and Silverman R. Seroprevalence of tetanus antibody titers in adults over 65 years of age. Annals of Emergency Medicine. 1996; 28:18-21.
Alagappan K, Rennie W, Kwiatkowski T, and Narang V. Antibody protection to diphtheria in the elderly. Annals of Emergency Medicine. 1997; 30:455-58.
Alagappan K, Rennie W, Narang V and Auerbach C. Immunologic response to tetanus toxoid in the elderly. Annals of Emergency Medicine. 1997; 30:459-462.
Alagappan K, Rennie W, Lin D, Auerbach C. Immunologic response to tetanus toxoid in the elderly:one year follow-up. Annals of Emergency Medicine. 1998; 32:155-60.
Talan D, Abrahamian F, Moran G, Mower W, Alagappan K, Tiffany B, Pollack C, Steele M, Dunbar L, Bajani M, Weyant R, Ostroff S. Tetanus immunity and physician compliance with tetanus prophlyaxis practices among emergency department patients presenting with wounds. Annals of Emergency Medicine. 2004, 43: 305-314
Alagappan K, Pulido G, Caldwell J, Abrahamian FM. Tetanus immunoprophylaxis in the emergency department: physician compliance in admitted versus discharged patients. Southern Medical Journal. Volume 99, No 3, 2006
Alagappan K, McGowan J, DeClaro D, Ng D, Silverman RA, Tetanus antibody protection among HIV-infected US-born patients and immigrants. International Journal of Emergency Medicine, Vol 2 : 123-126, June 2008
Alagappan K, Park R, Kuo T, Naderi S, Silverman R. Seroprevalence of tetanus antibody titers among Korean Americans in the New York City area -a pilot study, J Immigrant Minority Health. 11:105-107, 2009.
World Health Organization. Immunization surveillance, assessment and monitoring. Maternal and Neonatal Tetanus (MNT) elimination. http://www.who.int/immunization_monitoring/diseases/MNTE_initiative/en/index.html (Accessed on March 14, 2011).
Category: International EM
Posted: 3/6/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
-A genetic autosomal recessive blood disorders that result from a defect in either the alpha (α) or Beta (β) globin chain in the hemoglobin molecule.
-Most common in people from a Mediterranean origin.
-Three types depending on the affected globin chain, α, β, or Delta (δ)
-Presents as hemolytic anemia with hepato-splenomegaly.
-Can present as mild anemia and may be misdiagnosed as iron deficiency anemia.
-Diagnosis is made through studies such as bone marrow examination, hemoglobin electrophoresis, and iron studies.
-The disease can cause hemochromatosis, which may be worsened by repeated blood transfusions.
-Hemochromatosis damages multiple organs including the Liver, spleen, endocrine glands and the heart causing cardiomyopathy and consequently heart failure.
-Severe thalassemia usually requires blood transfusion on regular basis (first measure effective in prolonging life)
-Treatment of trait cases is symptomatic with analgesics, anti-inflammatory (steroids or NSAIDs)
-The introduction of chelating agents capable of removing excessive iron from the body has dramatically increased life expectancy.
-Deferasirox (Exjade) was approved by the FDA in January 2013 for treatment of chronic iron overload caused by nontransfusion-dependent thalassemia.
Delvecchio M, Cavallo L. Growth and endocrine function in thalassemia major in childhood and adolescence. J Endocrinol Invest. Jan 2010;33(1):61-8
Cunningham MJ, Macklin EA, Neufeld EJ, et al. Complications of beta-thalassemia major in North America. Blood. Jul 1 2004;104(1):34-9
Fucharoen S, Ketvichit P, Pootrakul P, et al. Clinical manifestation of beta-thalassemia/hemoglobin E disease. J Pediatr Hematol Oncol. Nov-Dec 2000;22(6):552-7
Claude Owen Burdick. "Separating Thalassemia Trait and Iron Deficiency by Simple Inspection". American Society for Clinical Pathology. http://ajcp.ascpjournals.org/content/131/3/444.short
Category: International EM
Posted: 2/13/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
- The most common disease producing enzymopathy in humans
- Affects 400 million people worldwide
- Highest prevalence is among persons of African, Asian, and Mediterranean descent
- Patients can be asymptomatic but may present with symptoms of acute hemolytic anemia, which may be precipitated by certain medications (Oxidative medications) or foods (some types of beans)
- Avoid oxidative drugs (consult your PharmD when your patient has G6PDd)
- Diagnosis: Measure the actual enzyme activity of G6PD rather than the amount of the enzyme. A more practical test is the presence of Indirect hyperbilirubinemia, but it is non specific
- Treatment consists of oxygen and bed rest in minor cases. However, severe cases may require PRBC transfusion
Beutler E. Glucose-6-phosphate dehydrogenase deficiency: a historical perspective. Blood. Jan 1 2008;111(1):16-24
Nkhoma ET, Poole C, Vannappagari V, et al. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. May-Jun 2009;42(3):267-78
Category: International EM
Posted: 1/16/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
More than 1.2 billion people are infected with at least one species.
Most helminth infections are contracted by ingesting the eggs, except strongyloides and hookworm whose larvae penetrate bare skin when it is contact with the soil.
The roundworm (Ascaris lumbricoides) life cycle involves migration through the lung tissue which can cause pneumonitis. Patients can present with interstitial infiltrates, wheeze, and blood tinged sputum. Ascaris than migrates to the intestines where it can cause partial small bowel obstruction. In pediatric patients, the appendix may be invaded causing gangrene with symptoms indistinguishable from appendicitis. In adults, the worms can invade the biliary tract and cause biliary disease or pancreatitis. Fever causes this helminth to migrate and it can emerge from the nasopharynx or the anus.
Whipworms (Trichuris trichiura) present as colitis or symptoms similar to inflammatory bowel disease. Chronic illness can involve anemia and clubbing. In severe cases, trichuris can cause dysentery and rectal prolapse.
Hookworms (Necator americanus or Ancylostoma duodenale) also have a pulmonary phase, but with milder symptoms than Ascaris. Eventually hookworms cause iron deficiency anemia and malnutrition. They can be a primary cause of anemia in pregnancy in endemic areas.
Threadworm (Strongyloides stercoralis) can cause a wide spectrum of disease presentations. The infection can start with a rash, larva currens. The infection may be subclinical or may invade the lung, intestinal wall, or the nervous system. Eventually hyperinfection may develop which is a very large increase in worm burden and then the infection becomes disseminated.
Toxocara canis or toxocara cati have affected approximately 14% of the US population. These helminthes reproduce in dogs or cats, and human infection is not part of the normal life cycle. Most infections are subclinical but it can produce a mild pneumonitis that is very similar to asthma. There can be pain and inflammation as the helminthes travel through organs such as the liver or lung and is called visceral larva migrans. The helminth may also move through the eye and optic never causing an ocular form of the disease, ocular larva migrans.
Pinworms (Enterobius vermicularis) are the cause of most common helminth infection in US and can present with anal pruritus leading to trouble sleeping. When an infection is identified, everyone in the household should be treated, regardless of symptoms.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD, MPH
J Bethony, S Brooker, M Albonico, S M Geiger, A Loukas, D Diemert, P J Hotez. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet: 2006; 367: 1521–32.
S Knopp, P Steinmann, J Keiser, J Utzinger. Nematode Infections: Soil-Transmitted Helminths and Trichinella Infect Dis Clin N Am: 2012; 26:341–358.
Category: International EM
Posted: 12/25/2012 by Walid Hammad, MD, MBChB
(Updated: 2/1/2026)
Click here to contact Walid Hammad, MD, MBChB
Bottom Line: A mild increase in blood parasite count after initiation of treatment is not uncommon. Marked increases should indicated treatment failure and the treatment drug should be changed to another class.
University of Maryland Section for Global Emergency Health
Author: Emilie J.B. Calvello, MD, MPH
Wurts, N. Et al. Early treatment failure during treatment of Plasmodium falciparum malaria with atovaquone-proquanil in the Repulic of Ivory Coast. Malar J 2012 May; 2(11): 146.
Silachomroon, U. Et al. Frequency of Early Rising Parasitemia in Falciparum Malaria Treated with Artemisinin Derivatives. Southeast Asian J Trop Med Pub Health 2001 Mar; 32(1): 50 – 56.
Category: International EM
Keywords: trypanosomiasis, Human African Trypanosomiasis, sleeping sickness, international (PubMed Search)
Posted: 12/19/2012 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
· A parasitic disease transmitted by the bite of the 'Glossina' insect (tsetse fly.)
· The disease is most prevalent in rural areas of Africa. Untreated, it is usually fatal. Infection with the genus Trypanosoma brucei gambiense may lead to chronic asymptomatic illness.
· Travelers to endemic areas in Africa are risk becoming infected.
· Symptoms resemble a viral illness; headaches, fever, weakness, pain in the joints, and stiffness. The parasite is able to crosses the blood-brain barrier and causes neurological symptoms, mainly psychiatric disorders, seizures, coma and ultimately death.
· Diagnosis is by serological tests (Card Agglutination Trypanosomiasis Test or CATT). Confirmation of infection requires the performance of parasitological tests to demonstrate the presence of trypanosomes in the patient.
· Treatment: four drugs are registered for the treatment of HAT: pentamidine, suramin, melarsoprol and eflornithine.
World Health Organization. (2010). Working to overcome the global impact of neglected tropical diseases. First WHO report on neglected tropical diseases. Available: http://whqlibdoc.who.int/publications/2010/9789241564090_eng.pdf. Last accessed 12/17/2012
Category: Airway Management
Posted: 12/5/2012 by Walid Hammad, MD, MBChB
(Updated: 2/1/2026)
Click here to contact Walid Hammad, MD, MBChB
40 yo previously healthy male in China who presents with prolonged “seizure” after receiving a cut on his foot while fishing 5 days ago.
Dx: Tetanus
Clinical features:
· Incubation period 4-14 days
· 3 clinical forms:
1. Local spasm
2. Cephalic (rare) - cranial nerve involvement
3. Generalized (most common) - Descending spasm: facial sneer (risus sardonicus), “locked jaw” trismus, neck stiffness, laryngeal spasm, abdominal muscle spasm.
· Spasms continue to 3-4 weeks and can take months to fully recover
Complications: apnea, rhabodymyolysis, fracture/dislocations
Treatment: supportive, benzodiazepines, RSI, Tetanus IG (3000-5000 units IM), wound debridement
University of Maryland Section for Global Emergency Health
Author: Veronica Pei, MD
Category: International EM
Posted: 11/14/2012 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
· Explosions can cause a complex series of injuries, which may include subtle or delayed findings. Repeated evaluations, such as serial abdominal exams, may be required.
· Blast injuries are divided into 4 categories:
o Primary blast injuries: Injury from blast wave over-pressure. Found in gas filled structures (ear, lung, hollow organs)
o Secondary blast injuries: Injury from thrown objects (primarily penetrating trauma, but may blunt)
o Tertiary blast injuries: Injuries from patient being thrown by blast wave (blunt trauma)
o Miscellaneous (quaternary) blast injuries: Injuries from other causes, such as burns, crush injuries, rhabdomyolysis, and toxic chemicals.
· The most common primary blast injury is tympanic membrane rupture.
University of Maryland Section for Global Emergency Health
Author: Jon Mark Hirshon
