Category: Cardiology
Posted: 3/22/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Acute Pericarditis
- Pericarditis has numerous etiologies; in developed countries 80-90% of cases are idiopathic/viral & 10-20% of cases are most commonly post-cardiac injury syndromes, connective-tissue diseases, or cancer.
- Diagnosis requires at least two of the following symptoms or signs: chest pain, pericardial friction rub, typical electrocardiographic changes, and pericardial effusion.
- Since pleuritic chest pain has many possible causes, pericarditis should be diagnosed with caution in the absence of other clinical criteria, additionally a friction rub & ECG findings may be transient making the diagnosis even more challenging.
- Data from a recent RCT indicated that pericardial effusions are present in ~2/3 of patients; the vast majority are small and of no concern, nonetheless an echocardiogram is routinely indicated and if present should be carefully followed to assess for tamponade.
- Treatment for idiopathic/viral cases of pericarditis consistents of NSAIDs & colchicine.
LeWinter, MM. Acute Pericarditis. NEJM. Dec 18, 2014 Vol 371 No 25.
Category: Cardiology
Posted: 3/8/2015 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Afib Clinical Decision Aid: AFFORD
- Atrial fibrillation (AF) affects ~34 million people worldwide; the hospital admission rates vary with frequencies of 81%, 62%, and 24% in the US, Australia, and Canada respectively.
- Lack of a reproducible and accurate risk stratification/decision aid likely contributes to variability in ED disposition.
- AFFORD (Atrial fibrillation and flutter outcome risk determination) was the 1st clinical decision aid (contains 17 variables) to predict 30-day adverse events in a prospective ED patient cohort with acute symptomatic AF.
- Vanderbilt University Medical Center's ED (2010-2013) derived and internal validated an ED based clinical decision aid for prediction of MACE within 30 days utilizing the AFFORD decision aid in hemodynamically stable patients whose AF reverted to sinus rhythm, either spontaneously or after cardioversion (pharmacologic or electrical), and those who are adequately rate controlled and candidates for outpatient management.
- Incorporating AFFORD with a shared decision model into ED practice may help identify patients at low risk and potentially reduce rate of hospitalizations.
Barrett TW, Storrow AB, et al. The AFFORD Clinical Decision Aid to Identify Emergency Department Patients With Atrial Fibrillation at Low Risk for 30-Day Adverse Events. The American Journal of Cardiology Volume 115, Issue 6, Pages 763-770 (15 March 2015).
Barrett TW, Storrow AB, et al. Atrial fibrillation and flutter outcomes and risk determination (AFFORD): design and rationale. J Cardiol, 58 (2011), pp. 124–130.
Category: Cardiology
Posted: 3/1/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Safety Risk? Digoxin in Atrial Fibrillation
- Digoxin is commonly utilize for atrial fibrillation/flutter with rapid ventricular response, though beta blockers and/or calcium channel blockers are a better 1st line therapy given digoxin’s narrow therapeutic index and lack of mortality benefit.
- Digoxin in the acute setting is often favored given its ability to reduce the heart rate while maintaining or slightly augmenting blood pressure.
- 2014 AHA/ACC guidelines recommend digoxin, specifically for rate control in patients with heart failure and/or reduced ejection fraction.
- There have been 2 post hoc studies from the AFFIRM trial which showed conflicting results w/regards to digoxin and risk of mortality.
1. Increased risk of mortality associated w/digoxin (on-treatment analytic strategy)
2. No association w/mortality (intent-to-treat analytic strategy)
- A recent retrospective cohort examination of newly diagnosed afib patients without heart failure & no prior use of digoxin; digoxin was independently associated with a 71% higher risk of death & a 63% higher risk of hospitalization.
- Consistent and substantial increase in mortality and hospitalization risk was seen using both on-treatment and intent-to-treat analytic methods.
- Given other available rate control options, digoxin should be used with caution.
Freeman J, Reynolds K, et al. Digoxin and Risk of Death in Adults With Atrial Fibrillation The ATRIA-CVRN Study. Circ Arrhythm Electrophysiol. 2015;8:49-58.
Category: Cardiology
Posted: 2/15/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
The Unforgotten: ECG Utilization to Differentiate Athletic Heart vs. Brugada
- Highly trained athletes develop ECG changes as a physiologic consequence of increased vagal tone; The ECG manifestations of early repolarization (ER) can range from simple J–point elevation to anterior (V1 to V3) "domed" ST-segment elevation and negative T wave.
- The former raises problems of differential some forms of ER with the “ coved-type” pattern seen in Brugada Syndrome (BS).
- A recent study compared the ECG tracings of 61 athletes w/a “domed” ST-segment elevation & negative T wave and 92 age/sex-matched BS patients w/a “ coved-type” pattern to identify an ECG criteria for distinguishing benign athletic changes seen in ER from BS.
- ECG analysis focused on ST-segment elevation at J-point (STJ ) and at 80 milliseconds after J-point (ST80 ).
- Athletes had a lower maximum amplitude of STJ (p < 0.001) & lower STJ /ST80 (p < 0.001)
- All patients (100%) with BS showed a downsloping ST-segment configuration (STJ/ST80 > 1) versus only 2 (3%) athletes (p < 0.001)
- An upsloping ST-segment configuration (STJ /ST80 < 1) showed a sensitivity of 97%, a specificity of 100%, and a diagnostic accuracy of 98.7% for the diagnosis of ER.
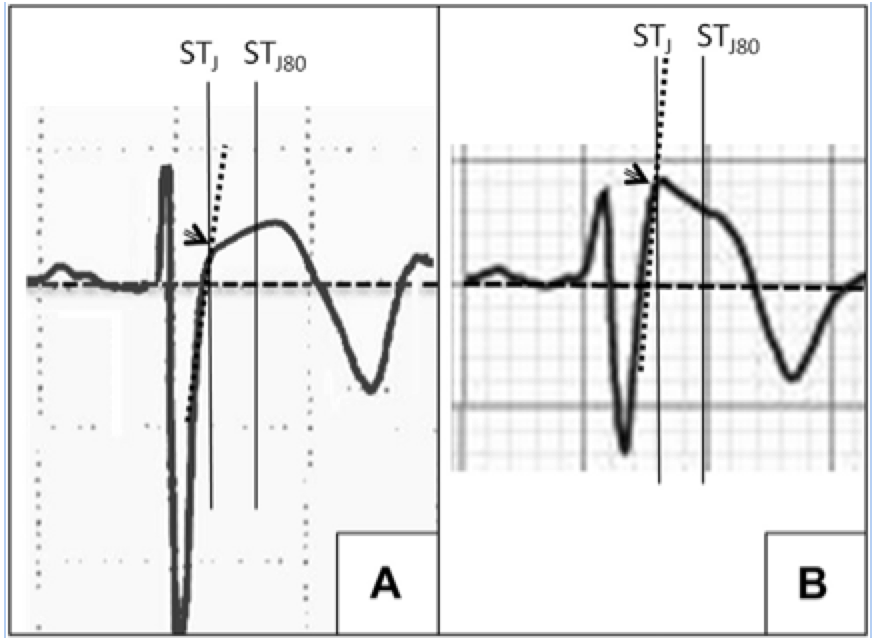
A: ER
B: Brugada
Zorzi A, Leoni L, et al. Differential Diagnosis Between Early Repolarization of Athlete’s Heart and Coved-Type Brugada Electrocardiogram. Am J Cardiol. 2015 Feb 15;115(4):529-32.
Category: Cardiology
Posted: 1/26/2015 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Posterior Myocardial Infarctions (PMI)
- Posterior myocardial infarctions (PMI) are different than typical ST-elevation MI; the ECG findings include: septal & anterior ST-segment depression, dominant tall/broad R waves, and upright T waves.
- In a study among 117,739 subjects with STEMI, 824 with PMI were more likely to present with cardiac arrest, cardiogenic shock, and congestive heart failure.
- The median time from arrival ECG to revascularization with PCI was longer among subjects with PMI.
- The median time from arrival ECG to systemic thrombolysis was also longer among subjects with a PMI.
- Increased awareness and recognition of PMI is needed to improve reperfusion times among this subpopulation with STEMI.
Waldo S, et al. Reperfusion times and in-hospital outcomes among patients with an isolated posterior myocardial infarction. Am Heart J 2014;167:350-354.
Category: Cardiology
Posted: 1/18/2015 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Left Ventricular Hypertrophy & Arrhythmias: Any Association?
Associations between left ventricular hypertrophy (LVH) and both supraventricular (SVT)/ventricular arrhythmias (VT/VF) have previously been reported.
A recent review & meta-analysis of 10 studies (27,141 patients) revealed the following:
- Incidence of SVT was 11% with LVH compared to 1% without (p <0.001)
- LVH patients had 3.4-fold greater odds of developing SVT
- Incidence of VT/VF was 5.5% with LVH compared to 1.2% without (p <0.001)
- LVH patients has 2.8 greater odds of developing VT/VF
The reason for increased arrhythmogenicity in LVH is not clearly understood.
A consistently observed abnormality in LVH is non-uniform propagation of the action potential throughout the myocardium, which sets the stage for arrhythmias based on early or delayed afterdepolarizations.
Given the heterogeneity in this meta-analysis further research between LVH & sustained arrhythmias is needed to infer true causality.
Saurav C, Chirag B, et al. Meta-Analysis of Left Ventricular Hypertrophy and Sustained Arrhythmias. The American Journal of Cardiology. Volume 114, Issue 7, Pages 1049-1052 (1 October 2014).
Category: Cardiology
Posted: 1/12/2015 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
APACHE-HF Scoring System
The Acute Physiology and Chronic Health Evaluation (APACHE) scoring system was established in the 1980's to predict critically ill patient prognosis (APACHE II, III, and IV have been published in last two decades).
The APACHE II scoring system involves combining 3 separate scores (acute physiology score, chronic health score, and age), which can be cumbersome to apply & thus is not often utilized in the emergency department (modified APACHE II doesn't include chronic health score & is less taxing).
No unique scoring system for acute heart failure (AHF) has been analyzed until present; the APACHE-HF score includes 8 criteria: mean arterial pressure (MAP), pulse, sodium, potassium, hematocrit, creatinine, age, and glasgow coma score (GCS).
AHF in-hospital mortality data was analyzed and compared using APACHE II, modified APACHE II, and APACHE- HF scores and the predictive value of the APACHE-HF score was found to be optimal when compared to the others.
Hirotake O, Akihiro S, et al. New scoring system (APACHE-HF) for predicting adverse outcomes in patients with acute heart failure: Evaluation of the APACHE II and Modified APACHE II scoring systems. Journal of Cardiology. Volume 64, Issue 6, Pages 421-510 (December 2014)
Category: Cardiology
Posted: 12/28/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Holiday Heart
- Holiday heart commonly refers to alcohol use and rhythm disturbances, particularly supraventricular tachydysrhythmias.
- The most common rhythm disorder is atrial fibrillation (AF), which usually converts to normal sinus rhythm within 24 hours and antiarrhythmic therapy is typically not indicated.
- Analyses of ECGs in patients who have consumed a large quantity of alcohol show prolongation of the PR, QRS, and QT intervals.
- 2014 AHA/ACC/HRS updated guidelines for nonvalvular AF utilize the CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75 years [doubled], diabetes mellitus, prior stroke or TIA or thromboembolism [doubled], vascular disease, age 65 to 74 years, and sex category) score for assessment of stroke risk.
Tonelo D, Providência R, Gonçalves L. Holiday heart syndrome revisited after 34 years. Arq Bras Cardiol. Aug 2013;101(2):183-9.
2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: Executive Summary. JACC Vol 64, Issue 21, Dec 2014.
Category: Cardiology
Keywords: Brugada (PubMed Search)
Posted: 12/21/2014 by Semhar Tewelde, MD
(Updated: 1/19/2015)
Click here to contact Semhar Tewelde, MD
Brugada Syndrome
Brugada syndrome is an inherited arrhythmogenic channelopathy described by ST-segment elevation in the right precordial leads and an increased risk of sudden cardiac death.
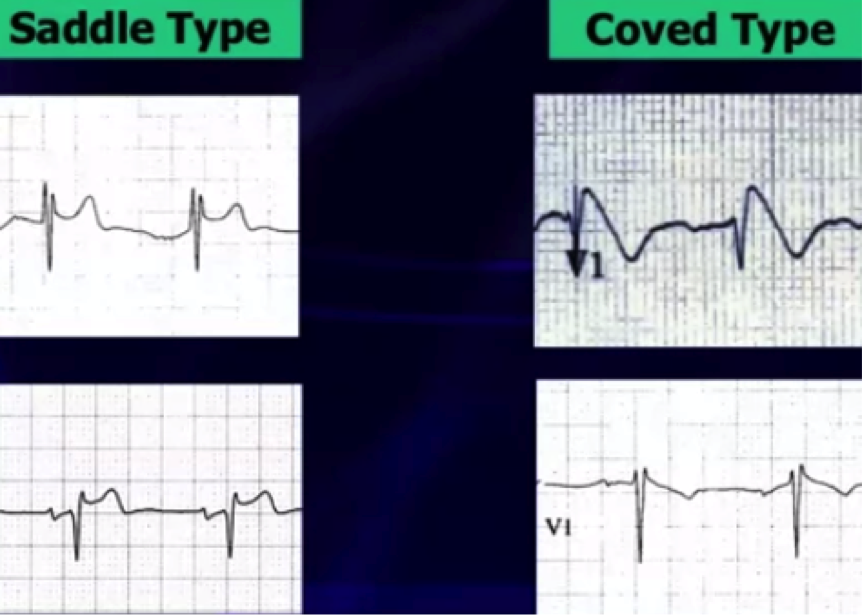
There are 3 electrocardiographic patterns:
Type 1 – Coved morphology w/ST-elevation >2 mm, followed by a negative T wave in at least 1 right precordial lead
Type 2 - Saddleback morphology w/ST-elevation >2mm, with a positive or biphasic T wave
Type 3 - Either coved, or saddleback morphology with <2mm ST-elevation
Type 1 pattern is often underestimated because of its sporadic/fluctuating appearance on ECG, which can be either spontaneously occurring or drug-induced (drug-induced variant has a more favorable prognosis).
Fever has been a well-documented culprit in unmasking Brugada pattern by increasing the sodium channel dysfunction & accelerating the late sodium current inactivation.
A recent study in a large population of patients with type 1 Brugada attempted to identify other patterns unmasking Brugada using 24-hour holter monitoring. * There is now evidence that there is a higher prevalence of type 1 Brugada pattern from 12pm-6pm & unmasking by fast and a large meal, showing influence by glucose intake and insulin levels.
Cerrato N, Giustetto C, et al. Prevalence of Type 1 Brugada Electrocardiographic Pattern Evaluated by Twelve-Lead Twenty-Four-Hour Holter Monitoring. The American Journal of Cardiology.Vol 115, Issue 1, 1 Jan. 2015, pgs. 52-56.
Category: Cardiology
Posted: 12/14/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Not So Benign: Benign early repolarization (BER) effects in STEMI
- Benign early repolarization (BER) has been associated with increased risk of sudden cardiac death and ventricular fibrillation (VF) in patients with and without structural heart disease.
- Acute STEMI is associated with high incidence of ventricular arrhythmias and the most frequent cause of sudden cardiac death in the adult population.
- BER has been associated with arrhythmogenicity, however the prognostic importance of this ECG finding in patients with STEMI has not been well elucidated.
- In a recent prospective study of STEMI patients, BER was associated with higher rates of in-hospital ventricular arrhythmias and mortality; It is an independent predictor of long-term mortality beyond well-known other parameters.
Ozcan K, et al. Presence of early repolarization on admission electrocardiography is associated with long-term mortality and MACE in patients with STEMI undergoing primary percutaneous intervention. Journal of Cardiology, Volume 64, Issue 3, September 2014, Pages 162-163.
Category: Cardiology
Posted: 12/7/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Predictors of Cardiac Rupture After AMI
- In the era of revascularization and aggressive cardiac care there has been a continual decline in acute myocardial infarction (AMI) mortality rates; however one of the most deadly complications, cardiac rupture (left ventricular free wall, ventricular septum, or papillary muscle rupture), still remains relatively stable.
- Cardiac rupture is an increasingly more frequent cause of death during AMI, thus a recent study retrospectively assessed the clinical and morphologic variables in those with and without cardiac rupture that were hospitalized for AMI.
- Cardiac rupture overwhelmingly complicates a first AMI.
- Cardiac rupture occurs most often in patients with an immense quantity of cardiac adipose tissue, the size of the left ventricular cavity is typically normal, and the area of the infarct is small.
- Heart failure patients with prior AMI have healed scar tissue and are at nominal risk of complications such as rupture if a subsequent AMI occurs.
Roberts W, et al. Commonalities of Cardiac Rupture (Left Ventricular Free Wall or Ventricular Septum or Papillary Muscle) During Acute Myocardial Infarction Secondary to Atherosclerotic Coronary Artery Disease. The American Journal of Cardiology. Volume 115, Issue 1, Pages 125-140 (1 January 2015).
Category: Cardiology
Keywords: Patent Foramen Ovale (PubMed Search)
Posted: 11/23/2014 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Patent Foramen Ovale: To Close or Not to Close
- Patent foramen ovale (PFO) is associated with a 3-fold increased risk for recurrent stroke, yet current guidelines only recommends “consideration” of PFO closure after a second cryptogenic stroke.
- Studies have demonstrated reductions in recurrent neurologic events with transcatheter PFO closure compared with medical therapy alone.
- Until recently the cost-effectiveness of PFO closure has not been described.
- Although PFO closure was found to be immediately more costly per patient closure, it reached cost-effectiveness at ~2.5 years of follow-up.
- Closure of PFO is both beneficial in terms of risk-benefit and cost-effectiveness strategy, especially as cryptogenic stroke typically affects the young.
Pickett C, Villines T, Ferguson M, et al. Cost Effectiveness of Percutaneous Closure Versus Medical Therapy for Cryptogenic Stroke in Patients With a Patent Foramen Ovale. The American Journal of Cardiology. Volume 114, Issue 10, Pages 1584-89 (15 November 2014)
Category: Cardiology
Posted: 11/9/2014 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Coronary Subclavian Steal Syndrome
Coronary subclavian steal syndrome (CSSS) is defined as coronary ischemia resulting from the reversal of flow in an internal mammary arterial graft usually secondary to subclavian stenosis.
Angiographic subclavian stenosis is defined as greater than 50% narrowing or greater than 20mmHg pressure difference across a lesion.
CSSS occurs in up to 4.5% of patients with prior CABG & common in older individuals with existing peripheral vascular disease.
CSSS most commonly manifests as stable angina, but frequently presents as unstable angina, acute myocardial infarction, acute systolic heart failure or even cardiogenic shock.
Screening for subclavian stenosis prior to CABG w/bilateral noninvasive blood pressure assessment, and a 15 mmHg or greater discordance should elicit further imaging.
Percutaneous revascularization is the first-line therapy for CSSS and has excellent long-term outcomes.
Sintek M, Coverstone E, Singh J. Coronary Sunclavian Steal Syndrome. Current Opinion in Cardiology. Issue: Volume 29(6) pgs. 506-513 November 2014.
Category: Cardiology
Posted: 11/2/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Heart Failure & Pulmonary Hypertension (Part II)
- HFpEF-PH management guidelines recommend the treatment of symptoms of congestion and volume overload, targeting LV relaxation and co-morbidities; including the management of pulmonary congestion, ischemia, sleep apnea, atrial fibrillation, and diabetes.
- Both atrial/ventricular dysrhythmias contribute to the mortality associated with HF & control of particularly atrial fibrillation, is an essential part of the early pulmonary vascular remodeling process.
- Both endothelin receptor antagonists (ERA) and prostanoids have been effective for PAH & clinical trials utilizing these agents have also been attempted in treatment of PH due to left heart disease, but have proven to be either neutral or even detrimental.
- Selective dilation of the pulmonary vessels in patients with postcapillary PH, without simultaneously ensuring the unloading of the LV, can cause profound pulmonary venous congestion resulting in sudden pulmonary edema, which greatly increases the morbidity in patients with this form of PH.
- Currently, the most compelling published data for pharmacological treatment targeting PH in HFpEF involves phosphodiesterase (PDE) inhibitor sildenafil.
Kanwar M, Tedford R, et al. Management of Pulmonary Hypertension due to Heart Failure with Preserved Ejection Fraction. Current Hypertension Reports. October 16, 2014.
Category: Cardiology
Posted: 10/26/2014 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Heart Failure & Pulmonary Hypertension (Part I)
~50% of patients with heart failure & preserved ejection fraction (HFpEF) develop pulmonary hypertension (PH)
HFpEF with PH portends reduced survival and increased hospitalization rates compared to those without PH
HFpEF-PH is often confused with idiopathic pulmonary hypertension (IPAH) given the similar hemodynamics; differentiating them is challenging and requires careful consideration of clinical, radiologic, and hemodynamic data
|
| PAH | HFpEF |
| Clinical parameters: | ||
| Age | Typically 3rd–5th decade | Typically 6th–8th decade |
| Comorbidities (HTN, HLD, DM, CAD) | Rare | Common |
| Atrial arrhythmias | Rare | Common |
| Obstructive sleep apnea | Rare | Common |
| Echocardiographic parameters: | ||
| LA size/volume | Normal | Increased |
| LV diastolic function | Normal to mildly abnormal | Moderate to severely abnormal |
| Hemodynamic parameters: | ||
| Resting PAWP | Always <15 mmHg | May be < or >15 mmHg |
| Response to volume | PAWP <15 mmHg (increase ≤5 mmHg) | PAWP >15 mmHg (increase >5 mmHg) |
| Response to exercise | PAWP <15 mmHg (increase ≤5 mmHg) | PAWP >15 mmHg (increase >5 mmHg) |
(Table reproduced from article)
Kanwar M, Tedford R, et al. Management of Pulmonary Hypertension due to Heart Failure with Preserved Ejection Fraction. Current Hypertension Reports. October 16, 2014
Category: Cardiology
Posted: 10/19/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Cardiovascular Morbidity & Sleep Apnea
Obstructive sleep apnea (OSA) is characterized by sleep-related periodic breathing, upper-airway obstruction, sleep disruption, and hemodynamic perturbations
Epidemiological data shows a strong association between untreated OSA & cardiovascular morbidity/mortality
Two recent studies by Gottlieb et al. (1) & Chirinos et al. (2) elucidated two important explicit and complicit treatment considerations for OSA
(1) In moderate-to-severe obstructive sleep apnea, the use of CPAP alone during sleep may ameliorate systemic hypertension and cardiovascular risk, even in patients who do not have "subjective" sleepiness
(2) Weight loss combined with CPAP use may further decrease cardiovascular morbidity
Basner R. Cardiovascular Morbidity and Obstructive Sleep Apnea. N Engl J Med 2014; 370:2339-2341 June 12, 2014
Category: Cardiology
Posted: 10/12/2014 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Kounis Syndrome (Part II)
- KS can develop from multiple etiologies: hymenoptera, proteins, vasoactive amines, histamine, acetylcholine, multiple antibiotics, and various medical conditions (angioedema, serum sickness, asthma, stress-induced cardiomyopathy).
- Hypersensitivity myocarditis and KS are two cardiac entities of allergic etiology affecting the myocardium and coronary arteries, respectively. These two entities can mimic each other and can be clinical indistinguishable.
- Presence of eosinophil’s, atypical lymphocytes, and giant cells on myocardial biopsy suggests hypersensitivity myocarditis.
- There is evidence showing use of corticosteroids with vasospastic angina with evidence of allergy or the presence of symptoms refractory to high-dose vasodilators has been reported to resolve symptoms.
Kounis GN, Soufras GD, Kouni SA, et al. Hypersensitivity myocarditis and hypersensitivity coronary syndrome (Kounis syndrome). Am J Emerg Med 2009;27:506–508.
Vivas D, Rubira JC, Ortiz AF, et al. Coronary spasm and hypersensitivity to amoxicillin: Kounis or not Kounis syndrome? Int J Cardiol 2008;128:279–281.
Category: Cardiology
Posted: 10/4/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Kounis Syndrome (Part I)
- Kounis & Zavras (1991) described the syndrome of allergic angina and allergic myocardial infarction, currently known as Kounis syndrome (KS). Braunwald (1998) noted vasospastic angina can be induced by allergic reactions, with mediators such as histamine and leukotrienes acting on coronary vascular smooth muscle.
- Two subtypes have been described: type I, occurring in patients without predisposing factors for CAD often caused by coronary artery spasm and type II, occurring with angiographic evidence of coronary disease when the allergic events induce plaque erosion or rupture.
- This syndrome has been reported in association with a variety of medical conditions, environmental exposures, and medication exposures. Entities such as Takotsubo cardiomyopathy, drug-eluted stent thrombosis, and coronary allograft vasculopathy also appear to be associated with this syndrome.
- Clinical presentation includes: symptoms and signs of an allergic reaction and acute coronary syndrome: chest pain, dyspnea, faintness, nausea, vomiting, syncope, pruritus, urticaria, diaphoresis, pallor, palpitations, hypotension, and bradycardia.
Kounis GN, Kounis SA, Hahalis G, et al. Coronary artery spasm associated with eosinophilia: another manifestation of Kounis syndrome? Heart Lung Circ 2009;18:163–164.
Mytas DZ, Stougiannos PN, Zairis MN, et al. Acute anterior myocardial infarction after multiple bee stings. A case of Kounis syndrome. Int J Cardiol 2009;134:e129–e131.
Category: Cardiology
Posted: 9/28/2014 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Ventricular Arrhythmias Originating from the Moderator Band
- Ventricular arrhythmias originating from the moderator band (MB) often have a distinct morphology
- Typically MB arrhythmias have a left bundle branch block pattern, QRS with a late precordial transition (>V4), a rapid down stroke of the QRS in the precordial leads, and a left superior frontal plane axis
- MB arrhythmias are often associated with PVC-induced ventricular fibrillation
- Catheter ablation is quite effective at termination of the arrhythmias and facilitated with intracardiac echocardiography (ICE)
Sadek M, Benhayon D, et al. Idiopathic ventricular arrhythmias originating from the moderator band: Electrocardiographic characteristics and treatment by catheter ablation. Heart Rhythm. Aug 2014
Category: Cardiology
Posted: 9/14/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Optimal Revascularization in Complex Coronary Artery Disease
- A multicenter trial 4,566 patients with NSTEMI, unstable angina, and multi-vessel coronary artery disease were enrolled comparing outcomes of cardiac stenting versus coronary artery bypass.
- Cardiac stenting was associated with improved outcomes and lower mortality in the following subgroups: age >65 years, women, unstable angina, TIMI score >4, and 2 vessel disease.
- Despite high clinical risk patients who underwent cardiac stenting compared to surgical revascularization did better in this prospective registry.
Buszman P, Buszman P, Bochenek A, et al. Comparison of Stenting and Surgical Revascularization Strategy in Non-ST Elevation Acute Coronary Syndromes and Complex Coronary Artery Disease (from the Milestone Registry). JACC Oct 2014 Vol 114, Issue 7, pages 979-987.
