Category: Gastrointestional
Keywords: PPI, Gi bleed (PubMed Search)
Posted: 7/22/2018 by Michael Bond, MD
Click here to contact Michael Bond, MD
Bottom Line:
Continuous vs intermittent dosing of PPIs in bleeding peptic ulcer disease
There continues to be debate as to the optimal dose, frequency, and route of proton pump inhibitors (PPIs) in bleeding ulcers, especially prior to endoscopy. Multiple guidelines including from the American Journal of Gastroenterology continue to recommend continuous dosing of PPIs.1,2,3 However, multiple studies appear to show at least non-inferiority when compared with intermittent dosing of PPIs.
The most frequently cited study for non-inferiority is a meta-analysis of 13 randomized control trials by Sachar et al. which evaluated PPI use in patients presenting with upper GI bleeds who were endoscopically found to have a bleeding gastric or duodenal ulcer with high risk features (active bleeding, non-bleeding visible vessel, or adherent clot)4. There was non-inferiority of intermittent dosing in rebleeding, need for repeat endoscopy/surgery, RBC transfusions, and mortality with a non-statistically significant trend towards superiority of intermittent dosing.
However, the patients were only randomized to continuous vs intermittent dosing AFTER endoscopic treatment. In addition, the dosing regimen of intermittent dosing was quite variable.
Continuous dosing:
Intermittent dosing:
Bottom Line:
References:
Category: Gastrointestional
Posted: 10/21/2017 by Michael Bond, MD
(Updated: 2/1/2026)
Click here to contact Michael Bond, MD
Infectious Diarrhea:
Have your wondered what you should do with patients that you suspect have infectious diarrhea. Well the IDSA has updated their 2001 guidelines for the management of infectious diarrhea. The TAKE HOME Points are:
You can find all the recommendations at https://academic.oup.com/cid/article/doi/10.1093/cid/cix669/4557073/2017-Infectious-Diseases-Society-of-America
Category: Gastrointestional
Keywords: Gastroparesis, haloperidol (PubMed Search)
Posted: 8/5/2017 by Ashley Martinelli
Click here to contact Ashley Martinelli
Take Home Point: In patients with diabetic gastroparesis, haloperidol may be an effective adjunctive treatment to prevent hospitalizations and reduce opioid requirements.
In Depth:
Study Design: single-center, retrospective review, case-matched to prior visit for gastroparesis
Patients:
52 patients with previously diagnosed diabetic gastroparesis by gastric motility study who presented to the ED for gastroparesis treatment
Groups:
Haloperidol administered visit
Haloperidol NOT administered visit (most recent visit, >7 days prior to haloperidol visit)
Results:
Baseline characteristics: median age 32 (21-57), 62% (32/52) female
Statistically significant reduction in hospital admissions for the haloperidol visit: (5/52 [10%] [CI 3-21%]) vs the non-haloperidol visit (14/52 [27%] [CI 16-41%]) p=0.02
Statistically significant reduction in opioid administration during the haloperidol visit: 6.75 ME (IQR 7.93) vs 10.75 ME (IQR 12) p=0.009
No difference in ED LOS, hospital LOS or need for additional antiemetics/prokinetics
No dystonic reactions, akathesia, excessive sedation, or cardiovascular complications in patients who received haloperidol
Limitations:
Small, single-center, retrospective study that only included patients with diabetic gastroparesis
Only intramuscular administration was studied
Baseline QT not reported
Young patient population, no description of comorbidities or home medications
Conclusions:
Haloperidol may be considered as an adjunctive therapy in patients with diabetic gastroparesis for its antiemetic and analgesic properties. Prospective studies are necessary to confirm findings.
Ramirez R, Salcup P, Croft B, Darracq MA. Am J Emerg Med 2017;35:1118-1120.
Category: Gastrointestional
Keywords: Diverticular, bleeding, gastrointestinal (PubMed Search)
Posted: 7/3/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Diverticular Bleeding
Category: Gastrointestional
Posted: 3/22/2010 by Rob Rogers, MD
(Updated: 2/1/2026)
Click here to contact Rob Rogers, MD
Complications of Liver Biopsy
Some considerations for the patient who presents with pain after a liver biopsy:
Consider getting a chest xray and a RUQ ultrasound to evaluate for these complications if they show up in the ED. CT scanning might also be required.
Also consider getting Interventional Radiology involved early in cases of bleeding as this is often the preferred treatment for biopsy site bleeding. In addition, a surgical consult is wise
in case the patient requires operative intervention.
Category: Gastrointestional
Keywords: PEG Tubes (PubMed Search)
Posted: 10/3/2009 by Michael Bond, MD
Click here to contact Michael Bond, MD
I am sure everybody has received a patient from a nursing home that had a malfunctioning PEG tube. Now if they would only crush the tablets before putting them down the tube, or better yet use liquid medications our life would be easier.
But what do you do if it is Friday and the GI lab is not open to Monday. The answer is that you can remove the PEG and replace it with another PEG tube or even a foley catheter will do for the weekend. The original PEG tube has a semi-rigid plastic ring (as shown in photo) and does not have a balloon that can be default. You can pull these out by placing counter traction on the abdominal wall and pulling with steady firm pressure. This may take a little more force than you are initially comfortable with.
Please see the attached photo of a PEG tube, and remember the other option is to admit these patients for IV fluids until the GI lab opens.
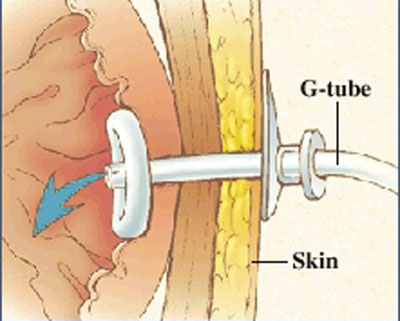
Photo taken from the Mount Littany Wellness library that can be accessed at http://www.mountnittany.org/wellness-library/healthsheets/documents?ID=6890
Category: Gastrointestional
Keywords: HIDA, narcotics, biliary colic (PubMed Search)
Posted: 8/30/2008 by Michael Bond, MD
(Updated: 2/1/2026)
Click here to contact Michael Bond, MD
Biliary Colic and Narcotics:
It is common to give patients with biliary colic narcotics inorder to relieve their pain. It was common teaching in the past that Morphine should be avoided due to the fact that it could cause spasm of the spincter of Oddi. It is now known that all narcotics, even meperidine, can cause spasm or irritation of the spincter of Oddi.
So this weeks pearls are:
Category: Gastrointestional
Keywords: Pancreatitis (PubMed Search)
Posted: 4/12/2008 by Michael Bond, MD
(Updated: 2/1/2026)
Click here to contact Michael Bond, MD
Some simple facts about Pancreatitis:
Category: Gastrointestional
Keywords: Variceal Bleed (PubMed Search)
Posted: 3/11/2008 by Rob Rogers, MD
(Updated: 2/1/2026)
Click here to contact Rob Rogers, MD
Medical Regimen for Suspected Variceal Bleed
To review what Dr. Bond and Dr. Winters have already posted:
Three medical therapies have been shown to be effective in patients with severe upper GI bleed thought to be due to esophageal varices:
Most of our gastroenterologists recommend this regimen (all three therapies)
Other things to consider:
Category: Gastrointestional
Keywords: Volvulus, Cause, (PubMed Search)
Posted: 11/17/2007 by Michael Bond, MD
(Updated: 2/1/2026)
Click here to contact Michael Bond, MD
Volvulus Quick Facts
Category: Gastrointestional
Keywords: Gi Bleed, Diveriticular, Bleed, (PubMed Search)
Posted: 9/22/2007 by Michael Bond, MD
(Updated: 2/1/2026)
Click here to contact Michael Bond, MD
Category: Gastrointestional
Keywords: Peptic Ulcer Disease, Omeprazole, Bleeding (PubMed Search)
Posted: 8/19/2007 by Michael Bond, MD
(Updated: 2/1/2026)
Click here to contact Michael Bond, MD
