Category: Administration
Keywords: Team building, belonging, team dynamics, emergency physicians, emergency nurses (PubMed Search)
Posted: 3/25/2025 by Mercedes Torres, MD
(Updated: 3/26/2025)
Click here to contact Mercedes Torres, MD
Better teamwork creates better outcomes in emergency medicine. This study investigated how communication practices between physicians and nurses in the ED influence team dynamics and the sense of belonging to the healthcare team.
Methods: 38 emergency physicians and emergency nurses from EDs within a single metropolitan area participated in focus groups.
Positive Influences on Team Belonging:
Negative Influences on Team Belonging:
The findings emphasize the importance of fostering positive communication practices to enhance team dynamics, cohesiveness, and overall well-being within ED healthcare teams.
Phillips J, Jones D. Qualitative Study of Dynamics, Camaraderie, and Belonging Among Emergency Physicians and Nurses. J Emerg Med. 202569doi:10.1016/j.jemermed.2024.08.011
Category: Administration
Keywords: Ramadan, fasting (PubMed Search)
Posted: 3/15/2025 by Hanna Hussein, MD
(Updated: 2/1/2026)
Click here to contact Hanna Hussein, MD
Ramadan is the holy month in the Islam faith, where observers will fast from sunrise to sunset. This includes food, water, some medications, smoking and sex. This can obviously have some impact on patients' health, especially when presenting to the ED. Here are some considerations to keep in mind:
As with everything, maintaining cultural awareness and compassion will help to
M Nadir Bhuiyan 1,?, Rayya A Saadiq 1, Michael R Mueller 1, Ahmed D Abdalrhim 1, Joshua Overgaard 1
PMCID: PMC11268016 PMID: 39050928
Category: Administration
Keywords: Nurse Practitioner, Physician Assistant, job satisfaction, burnout, longevity (PubMed Search)
Posted: 2/20/2025 by Steve Schenkel, MPP, MD
(Updated: 2/26/2025)
Click here to contact Steve Schenkel, MPP, MD
Nurse Practitioners and Physician Assistants practice alongside Physicians in Emergency Departments. In 2021, an estimated 17,679 NPs and PAs worked in EDs.
How long do NPs and PAs continue in Emergency Medicine practice?
An analysis of Medicare data reports that over the eight years of the study, the annual attrition rate averaged 13.8%, or almost 1 in 7 leaving Emergency Medicine practice every year. At the time of attrition, the median age for women was 40.2 years (IQR 33.8 to 49.9) and for men was 45.9 (IQR 37.8 to 56.3).
For additional breakdown and discussion of these numbers, see Gettel CJ, Chosh R, Rothenberg, et al. Workforce Attrition Among Emergency Medicine Non-Physician Practitioners. Ann Emerg Med, in press, https://www.annemergmed.com/article/S0196-0644(24)01294-0/fulltext.
Category: Administration
Keywords: Burnout, Wellbeing, Workforce (PubMed Search)
Posted: 1/22/2025 by Mercedes Torres, MD
(Updated: 2/1/2026)
Click here to contact Mercedes Torres, MD
On March 18, 2022, Congress passed the Dr. Lorna Breen Health Care Provider Protection Act, named after an emergency medicine physician who died by suicide during the pandemic. This landmark legislation allocated $103 million across 45 organizations to introduce evidence-based measures to mitigate and prevent burnout.
As a result, the Impact Wellbeing Guide was developed, outlining the six key evidence-based action steps for organization leaders to address health care workers’ professional well-being listed below:
The Guide is designed to help hospital leaders and executives accelerate or supplement professional wellbeing work in their hospitals at the operational level.
A PDF of the full guide is available from the CDC: https://www.cdc.gov/niosh/docs/2024-109/
https://www.cdc.gov/niosh/healthcare/impactwellbeingguide/
Bock A. To Fix Burnout, New Initiatives Go Beyond Worker Resilience and Put Onus on Health Systems. JAMA. 2024;331(24):2067–2069. doi:10.1001/jama.2024.6216
Category: Administration
Keywords: push notification, EMR, ED flow, results, radiology (PubMed Search)
Posted: 12/26/2024 by Steve Schenkel, MPP, MD
(Updated: 2/1/2026)
Click here to contact Steve Schenkel, MPP, MD
Clinical practice in the world of the Electronic Medical Record has made many a clinician question the value of electronic reminders.
Banners warn of sepsis, the need for repeat evaluation, vital signs outside expected limits, wait times, and risks for readmission.
Can they instead help ED flow?
Sayan Dutta and colleagues suggest that they can. When clinicians chose to receive notice of a lab or imaging result, push notification reduced time between final result and ED disposition by 18 minutes (95% CI: 15-21 minutes).
The likely key here? Clinicians actively chose when and about what to be notified.
See: Result Push Notifications Improve Time to Emergency Department Disposition: A Pragmatic Observational Study, Annals of Emergency Medicine, 85(1), 53-62. https://www.annemergmed.com/article/S0196-0644(24)00404-9/abstract.
Result Push Notifications Improve Time to Emergency Department Disposition: A Pragmatic Observational Study
Dutta, Sayon et al.
Annals of Emergency Medicine, Volume 85, Issue 1, 53 - 62
Category: Administration
Keywords: Thanksgiving (PubMed Search)
Posted: 11/27/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
From all of us at UMEM, Happy Thanksgiving!!
We are incredibly Thankful for each of you and all that you do to care for patients and their families.
We are Thankful for those legends who have blazed the path in EM like Greg Henry who the EM community lost yesterday. Our thoughts are with his family. Thank you Dr. Henry for inspiring so many of us. Our pearls today are two of his famous quotes:
“Medicine is show business for ugly people.”
“You don’t go to Disney and see Mickey taking a smoke break. You have to be on when you are on shift”
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/27/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Gooble, gooble,… gulp, some food for thought on the eve of Thanksgiving.
The development of artificial intelligence (AI) in emergency medicine is well under way. The schematic below and accompanying reference presents the anticipated stages in the process of AI development, including important features, considerations, and challenges as we move towards increased integration of AI in our practice of EM.
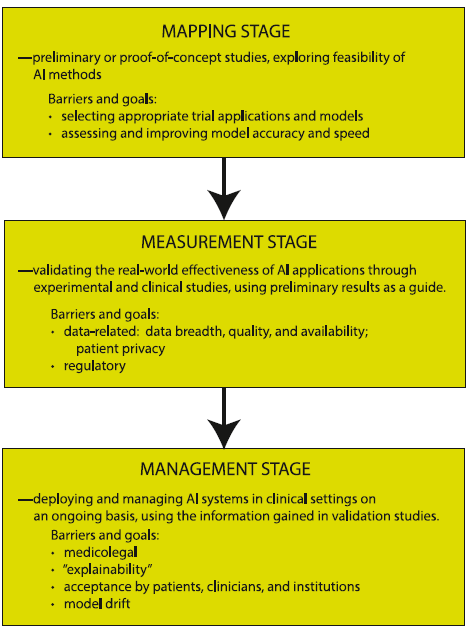
Petrella, R. The AI Future of Emergency Medicine. Ann Emerg Med. 2024;84:139-153. https://doi.org/10.1016/j.annemergmed.2024.01.031
Category: Administration
Keywords: physician practice, morality, altruism, professionalism (PubMed Search)
Posted: 10/17/2024 by Steve Schenkel, MPP, MD
(Updated: 10/23/2024)
Click here to contact Steve Schenkel, MPP, MD
Does physician altruism influence quality metrics? This study suggests yes.
45 physicians were defined as “altruistic” based on their willingness to share a $250 cash prize with a stranger in an on-line version of the dictator game, something you might have played in an economics class.
Of 250 physicians drawn from primary care and cardiology, 45 met the definition of altruistic and 205 did not.
Overall, patients of altruistic physicians:
The authors suggest that this difference may be on account of altruistic physicians being more willing to consider the appropriateness of tests or treatment or “devote more time and energy to their patients.”
They also note that while most physicians were categorized as not altruistic, at 18% this group of physicians exceeds the 5% of the general US population that would meet this definition.
Perhaps there is something quantitatively demonstrable to being a “good” doctor.
See https://jamanetwork.com/journals/jama-health-forum/fullarticle/2824419
Casalino LP, Kariv S, Markovits D, Fisman R, Li J. Physician Altruism and Spending, Hospital Admissions, and Emergency Department Visits. JAMA Health Forum. 2024;5(10):e243383. doi:10.1001/jamahealthforum.2024.3383
Category: Administration
Keywords: design, workspace, handoff, interruptions, collaboration (PubMed Search)
Posted: 9/21/2024 by Mercedes Torres, MD
(Updated: 9/25/2024)
Click here to contact Mercedes Torres, MD
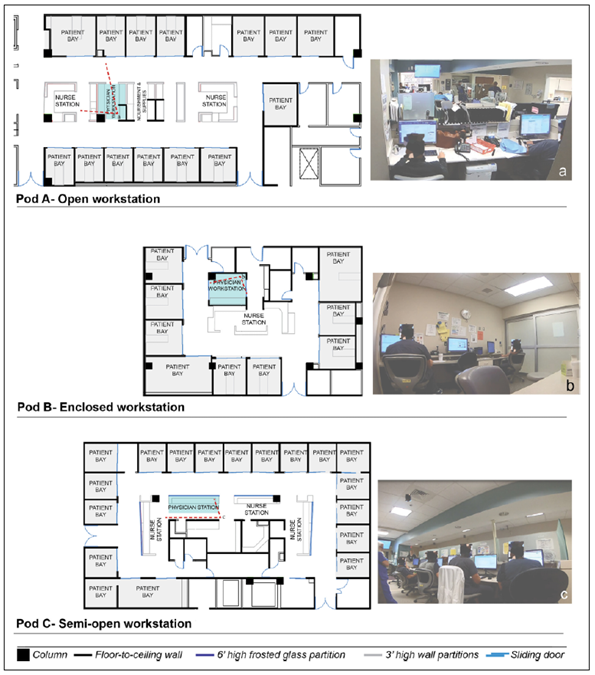
Joshi R, Joseph A, Ossmann M, et al. Emergency Physicians’ Workstation Design: An Observational Study of Interruptions and Perception of Collaboration During Shift-End Handoffs. HERD: Health Environments Research & Design Journal. 2021;14(4):174-193. doi:10.1177/19375867211001379
Category: Administration
Keywords: Medicare advantage, insurance, payor, fee-for-service (PubMed Search)
Posted: 8/28/2024 by Steve Schenkel, MPP, MD
(Updated: 2/1/2026)
Click here to contact Steve Schenkel, MPP, MD
Traditional Medicare now covers < 50% of Medicare beneficiaries. It reimburses on a fee-for-service basis. For beneficiaries, it includes deductibles and coinsurance requirements that yield average annual out-of-pocket expenses measured in the thousands of dollars.
Medicare Advantage, the new alternative, has grown quickly. Plans typically promise beneficiaries fewer co-pays and more services. It relies on private insurers (think United, Blue Cross, Kaiser Permanente) to coordinate care and rein in costs. Subsidies to Medicare Advantage have helped spur growth, subsidies that mean costs per beneficiary for Medicare Advantage exceed those for traditional Medicare.
Which means Medicare still needs to figure out how to save money and remain viable while the US population over 65 grows.
When listening to a lecture about Medicare or reading a study that uses Medicare data, take a moment to ask “Which Medicare? Fee-for-service? Or Advantage?”
For a take on the future of Medicare, see McWilliams JM, The Future of Medicare and the Role of Traditional Medicare as Competitor, NEJM, August 22/29, 763-769.
To understand why Medicare Advantage plans are popular, see https://www.kff.org/medicare/issue-brief/10-reasons-why-medicare-advantage-enrollment-is-growing-and-why-it-matters/.
Category: Administration
Keywords: confounding factors, epidemiologic (PubMed Search)
Posted: 8/21/2024 by Mike Witting, MS, MD
Click here to contact Mike Witting, MS, MD
“I’m not going to the hospital, my father died in a hospital.”
In planning a study it’s a good practice to consider what confounding variables you may need to look out for.
Confounding variables are associated with the predictor (independent) and outcome (dependent) variables, but they are not in the causal chain. In the above example, disease is likely the predictor variable, death is the outcome variable, and going to the hospital is a confounder. Of course, this assumes the death was not iatrogenic; then the hospital would be in the causal chain.
Patients may be selected for interventions based on severity of disease, functional status, education level, and other factors, and these may be confounders.
Confounding can be addressed at the design stage, by:
It can be addressed in the analysis stage by:
Adapted from Hulley SB, Cummings SR. Designing clinical research, 4th edition, Lippincott, Williams and Wilkins, 2013.
Category: Administration
Keywords: racial disparities, antibiotic prescribing (PubMed Search)
Posted: 8/14/2024 by Kevin Semelrath, MD
(Updated: 8/17/2024)
Click here to contact Kevin Semelrath, MD
This retrospective study found that while overall rates of antibiotic prescriptions for viral URIs were low (that's good!), patients identified as non Hispanic white were prescribed antibiotics, despite guidelines advising against them, at a higher rate than non white patients (that's bad). It also found that in areas of socioeconomic deprivation, the prescribing rates were lower across all races than in more affluent areas (that's good and bad!)
Open AccessPublished:January 23, 2024DOI:https://doi.org/10.1016/j.annemergmed.2023.12.003
Category: Administration
Keywords: Administration, Meetings, Workforce satisfaction (PubMed Search)
Posted: 7/24/2024 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Participation in meetings is an expected part of most (if not all) of our jobs. How many of these meetings are necessary? Could some of the “work” of meetings be accomplished with a few emails or other asynchronous forms of communication? Are meetings cluttering your schedule and making it impossible to get any real work done?
Some answers to these questions are offered in a Harvard Business Review article from March 2022.
Key points include:
Advantages to fewer meetings:
Authors recommend holding meetings only when “absolutely” necessary. That typically includes:
Laker B, Pereira V, Malik A, and Soga L. Meeting Management: Dear Manager, You’re Holding Too Many Meetings. Harvard Business Review. March 9, 2022.
Category: Administration
Keywords: osteomyelitis, antibiotics, golden hour, trauma, open fracture (PubMed Search)
Posted: 7/17/2024 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
Early administration of antibiotics for open fractures can reduce serious bone and soft tissue infections, with a common goal being antibiotic administration within one hour of injury.
In this study, there were 523 patients treated by EMS who had an open extremity fracture.
The median time from EMS dispatch until antibiotic administration was 31 minutes. 99% of the patients who received antibiotics received them within one hour of EMS dispatch. Prehospital times were on average 10 minutes longer for those patients who received antibiotics. The majority of these patients received cefazolin, followed by ceftriaxone, ampicillin, gentamicin and piperacillin/tazobactam. None of these patients required management for an allergic reaction or anaphylaxis. Five patients (1%) who received prehospital antibiotics and 159 patients who did not (1.4%) had a subsequent infection based on ICD codes.
Bottom line: In this small group, it was safe to administer antibiotics to a patient with an isolated open extremity fracture and the medication was able to be delivered earlier. Larger studies will be needed to see the impact of this practice on the development of osteomyelitis or soft tissue infections.
Muniz AD, Gregorio DJ, Studebaker SA, et al. Time Savings and Safety of EMS Administration of Antibiotics for Open Fractures. Prehosp Emerg Care. Published online April 25, 2024. doi:10.1080/10903127.2024.2347291
Category: Administration
Keywords: administrative harm, employee, adverse events (PubMed Search)
Posted: 6/26/2024 by Steve Schenkel, MPP, MD
(Updated: 2/1/2026)
Click here to contact Steve Schenkel, MPP, MD
“Administrative harm” (defined as “the adverse consequences of administrative decisions within health care”) is a relatively new term for challenges that arise in complex health care work environments.
41 mostly hospitalists participating in interviews and focus groups found that the concept resonated, and that administrative harms could arise at all levels of leadership, negatively impacted both workforce and patients, were challenging to measure, and pointed to a lack of leadership responsibility and accountability. The group also suggested many approaches and solutions for prevention.
The article is here, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2820266. If interested, take a look at the thematic tables 2 and 3.
There is a brief editorial comment here, https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2820275.
Category: Administration
Keywords: STI, prophylaxis (PubMed Search)
Posted: 6/24/2024 by Visiting Speaker
(Updated: 2/1/2026)
Click here to contact Visiting Speaker
Author:
Gabriella Miller (She/Her)
Clinical Instructor
Department of Emergency Medicine
University of Maryland School of Medicine
Doxycycline PEP for the prevention of bacterial STIs.
The CDC now recommends “doxy PEP” for high-risk individuals. Doxycycline post-exposure prophylaxis (doxy PEP) is a prescription for patients to self-administer 200 mg doxycycline by mouth within 72 hours after anal, oral, or vaginal sex to prevent the transmission of chlamydia, gonorrhea, and syphilis. The CDC defines “high-risk” as men who have sex with men (MSM) and transgender women (TGW) who have been diagnosed with a bacterial STI within the past 12 months. They summarize the findings of the French IPERGAY and ANRS DOXYVAC studies, as well as the US DoxyPEP study, which all show promising reductions in risk ratios or hazard ratios of decreasing bacterial STI transmission on high-risk populations, including those who are taking PrEP for HIV. No significant adverse events related to doxy PEP have been reported.
Conclusion:
Counsel patients at high risk for bacterial STIs regarding the prescription of doxy-PEP for patient self-administration within 72 hours after sex.
Bachmann LH, Barbee LA, Chan P, et al. CDC Clinical Guidelines on the Use of Doxycycline Postexposure Prophylaxis for Bacterial Sexually Transmitted Infection Prevention, United States, 2024. MMWR Recomm Rep. 2024;73(2):1-8. Published 2024 Jun 6. doi:10.15585/mmwr.rr7302a1
Category: Administration
Keywords: pulse oximetry, skin pigmentations (PubMed Search)
Posted: 6/15/2024 by Kevin Semelrath, MD
(Updated: 2/1/2026)
Click here to contact Kevin Semelrath, MD
This article shows us that even things we think of as objective measures in medicine may actually perpetuate systemic biases.
The study evaluated controlled hypoxemia in a group of volunteers. Traditional pulse ox devices measured falsely elevated pulse ox readings in participants with dark skin pigmentation and low tissue perfusion. It suggested different types of devices that may have improved accuracy in patients with darker skin pigmentation, but the underlying problem still exists.
Bottom line, this goes to prove what we have taught, never rely on a single value to reassure yourself of the patient's status, always take into account the bigger picture.
Low Perfusion and Missed Diagnosis of Hypoxemia by Pulse Oximetry in Darkly Pigmented Skin: A Prospective Study. Anesth Analg. 2024 Mar 1;138(3):552-561. doi: 10.1213/ANE.0000000000006755. Epub 2023 Dec 18. PMID: 38109495
Category: Administration
Keywords: POCUS, musculoskeletal, fingers, water baths (PubMed Search)
Posted: 6/3/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/1/2026)
Click here to contact Alexis Salerno Rubeling, MD
Do you have a patient with a finger injury or infection, or possibly a retained foreign body?
Try placing the hand in a water bath and use a linear ultrasound probe for evaluation. If there is an open wound, use a sterile ultrasound probe cover.
With ultrasound guidance, you can observe dynamic finger movements and identify areas that may require abscess drainage.
Category: Administration
Keywords: Specialty ED, Geriatric ED, Oncologic ED (PubMed Search)
Posted: 5/21/2024 by Mercedes Torres, MD
(Updated: 5/22/2024)
Click here to contact Mercedes Torres, MD
There is a growing trend toward the development of specialty-specific emergency services, such as Geriatric or Oncologic EDs.
Will this trend continue? Is the segmentation of emergency care in our future? The author of this article opines that the answer depends on future outcomes research in this area.
Brouillette M. Are Specialty Emergency Departments the Future of Emergency Care? Oncology- and Geriatric-Focused Emergency Departments Hope to Improve Care, Lower Costs. Annals of Emergency Medicine. May 2024, 83(5):9A-12A. https://doi.org/10.1016/j.annemergmed.2024.03.015
Category: Administration
Posted: 5/13/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This retrospective study looked at patients diagnosed with urinary tract infections receiving an IV dose of antibiotics prior to discharge and compared ED length of stay and return visit rate. They found:
“Parenteral antibiotic administration in the ED was associated with a 60-minute increase in ED LOS compared with those who received an oral antibiotic (P < 0.001) and a 30-minute increase in ED LOS compared with no antibiotic (P < 0.001). No differences were observed in revisits to the ED at 72 hours”
Appears no benefit to the practice of IV antibiotics prior to discharge in UTI patients.
Mohammed A. Alrashed Stephen J. Perona Mark C. Borgstrom Elias Ramirez-Moreno
JAPhA VOLUME 64, ISSUE 3, 102020, MAY 2024
Published:January 29, 2024DOI:https://doi.org/10.1016/j.japh.2024.01.016
