Category: Administration
Keywords: trauma, EMS, hemorrhagic shock (PubMed Search)
Posted: 5/3/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
Prehospital administration of whole blood involves some areas of controversy. Though theoretical benefits are clear, concerns about logistics and timing of blood often dominates the discussion. This study was a retrospective analysis of prehospital blood administration within an urban EMS system from 2021-2023. Primary endpoints included: time to administration and in hospital mortality.
PATIENTS/METHODS:
The study population included patients presenting to the EMS system with signs and symptoms of hemorrhagic shock (SBP<70 or SBP<90 + HR> 100, n=61) and who received at least 1 unit of prehospital blood (PHB). The EMS system administered blood in conjunction with an advanced resuscitative bundle (calcium, TXA, blood). Isolated head injuries and blunt trauma patients were excluded from the analysis. The control group (n=82) was comprised of patients in the system's trauma registry presenting to EMS PRIOR to the initiation of whole blood and who exhibited similar clinical crtieria.
RESULTS:
BOTTOM LINE:
In this prospective study conducted within an urban EMS system, patients receiving prehospital whole blood demonstrated improved vital signs and reduced mortality when compared to a control group. Slightly extended prehospital time intervals for patients receiving PHB may be offset by the measured benefits of whole blood therapy.
Duchesne, J. , McLafferty, B. , Broome, J. , Caputo, S. , Ritondale, J. , Tatum, D. , Taghavi, S. , Jackson-Weaver, O. , Tran, S. , McGrew, P. , Harrell, K. , Smith, A. , Nichols, E. , Dransfield, T. , Marino, M. & Piehl, M. (9900). Every minute matters: Improving outcomes for penetrating trauma through prehospital advanced resuscitative care. Journal of Trauma and Acute Care Surgery, Publish Ahead of Print , doi: 10.1097/TA.0000000000004363.
Category: Administration
Keywords: staffing, employment, Teamhealth, Medstar, Edelman (PubMed Search)
Posted: 3/16/2024 by Steve Schenkel, MPP, MD
(Updated: 4/17/2024)
Click here to contact Steve Schenkel, MPP, MD
Emergency Medicine staffing groups can be organized in any number of ways. Here’s Leon Adelman’s take:
Read more at https://emworkforce.substack.com/p/state-of-the-us-emergency-medicine-677. Read closely and you’ll find a reference to Maryland.
Category: Administration
Keywords: Administration, Patient Experience, Microaggression, Discrimination (PubMed Search)
Posted: 3/27/2024 by Mercedes Torres, MD
(Updated: 2/1/2026)
Click here to contact Mercedes Torres, MD
Do microaggressions and discrimination impact the patient experience in your ED? How can we address this?
This article is one of few studies to address this topic specifically in the ED. Authors used quantitative (discrimination scale) and qualitative (follow-up interviews) methods to answer this question in two urban academic EDs.
Common themes from patient responses provide food for thought and action in this regard:
Punches BE, Osuji E, Bischof JJ, et al. Patient perceptions of microaggressions and discrimination toward patients during emergency department care. Acad Emerg Med. 2023; 30: 1192-1200. doi:10.1111/acem.14767
Category: Administration
Keywords: Ramadan, fasting (PubMed Search)
Posted: 3/16/2024 by Kevin Semelrath, MD
(Updated: 2/1/2026)
Click here to contact Kevin Semelrath, MD
This study is out of the American University of Beirut, Lebanon, and courtesy of our own Mazen El Sayed!
Many patients of Muslim faith will observe fasting during the month of Ramadan, with no food, water, oral of IV medication taken from sunrise to sunset
This study showed a lower daily ED volume than during non Ramadan months, however did show a higher length of stay during Ramadan.
It also found an increase in mortality rates during Ramadan (OR 2.88) and 72 hour ED bounce-backs (OR 1.34)
Be sensitive and aware of the needs of your patients of Muslim faith during this holy month of fasting.
Ramadan Kareem
Impact of Ramadan on emergency department visits and on medical emergencies. Reem G Al Assaad, Rana Bachir, Mazen J. El Sayed. Europena Journal of Emergency Medicine. 2018, 25:440-444.
Category: Administration
Keywords: employee, independent contractor, employment, job market (PubMed Search)
Posted: 1/12/2024 by Steve Schenkel, MPP, MD
(Updated: 2/28/2024)
Click here to contact Steve Schenkel, MPP, MD
The relationship between an Emergency Physician and the hiring group (whether large or small) may be one of employer-employee or contactor-independent contractor. There are legal job protections for employees that don’t exist for independent contractors. There are also regulations that define an independent contractor. Enforcement of these regulations varies but may be increasing. This has implications for the Emergency Medicine job market. We have the highest percentage of independent contractors of any medical specialty.
See more at Leon Adelman’s Emergency Medicine Workforce Newsletter, here https://emworkforce.substack.com/p/thousands-of-employed-emergency-physicians
Category: Administration
Posted: 2/22/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This research letter notes: “The Rural Emergency Hospital is a new Medicare payment model available to hospitals with 50 or fewer beds in rural areas. Rural hospitals converting to this model will have emergency department (ED), observation, and outpatient services.”. Their study concludes that the majority of these hospitals already transfer the vast majority of their admissions to larger hospitals and this designation is a recognition of already established practices.
https://doi.org/10.1016/j.annemergmed.2023.08.492
RESEARCH LETTER| VOLUME 83, ISSUE 2, P177-180, FEBRUARY 2024
Category: Administration
Keywords: Transfer, surgery, scoping review, further research (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/11/2024)
Click here to contact Robert Flint, MD
These authors performed a scoping review of English language studies involving United States general surgery patients that required transfer to another facility looking at timing of transfer, triage guidelines, and mode of transport . They concluded: “There were mixed results for the impact of transfer timing on outcomes with heterogeneous definitions of delay and populations. Triage guidelines for EGS transfer were consensus or expert opinion. No studies were identified addressing the mode of interfacility EGS transfer.” More research is needed in the area concerning timing, triage and mode of transport for these patients.
Silver, David S. MD, MPH; Teng, Cindy MD; Brown, Joshua B. MD, MSc. Timing, triage, and mode of emergency general surgery interfacility transfers in the United States: A scoping review. Journal of Trauma and Acute Care Surgery 95(6):p 969-974, December 2023. | DOI: 10.1097/TA.0000000000004011
Category: Administration
Keywords: Medicare advantage, insurance, payor (PubMed Search)
Posted: 1/12/2024 by Steve Schenkel, MPP, MD
(Updated: 1/30/2024)
Click here to contact Steve Schenkel, MPP, MD
Approximately half of all Medicare beneficiaries are now enrolled in Medicare Advantage plans. Why does this matter?
Intrigued? Learn more at https://www.nejm.org/doi/full/10.1056/NEJMhpr2302315 or https://www.kff.org/medicare/issue-brief/medicare-advantage-2024-spotlight-first-look/.
Category: Administration
Keywords: Risk, diagnostic error (PubMed Search)
Posted: 1/21/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
From the Canadian Medical Protective Association looking at 5 years of closed medical legal cases. This fits with previous risk management data and should give us pause when treating these conditions.
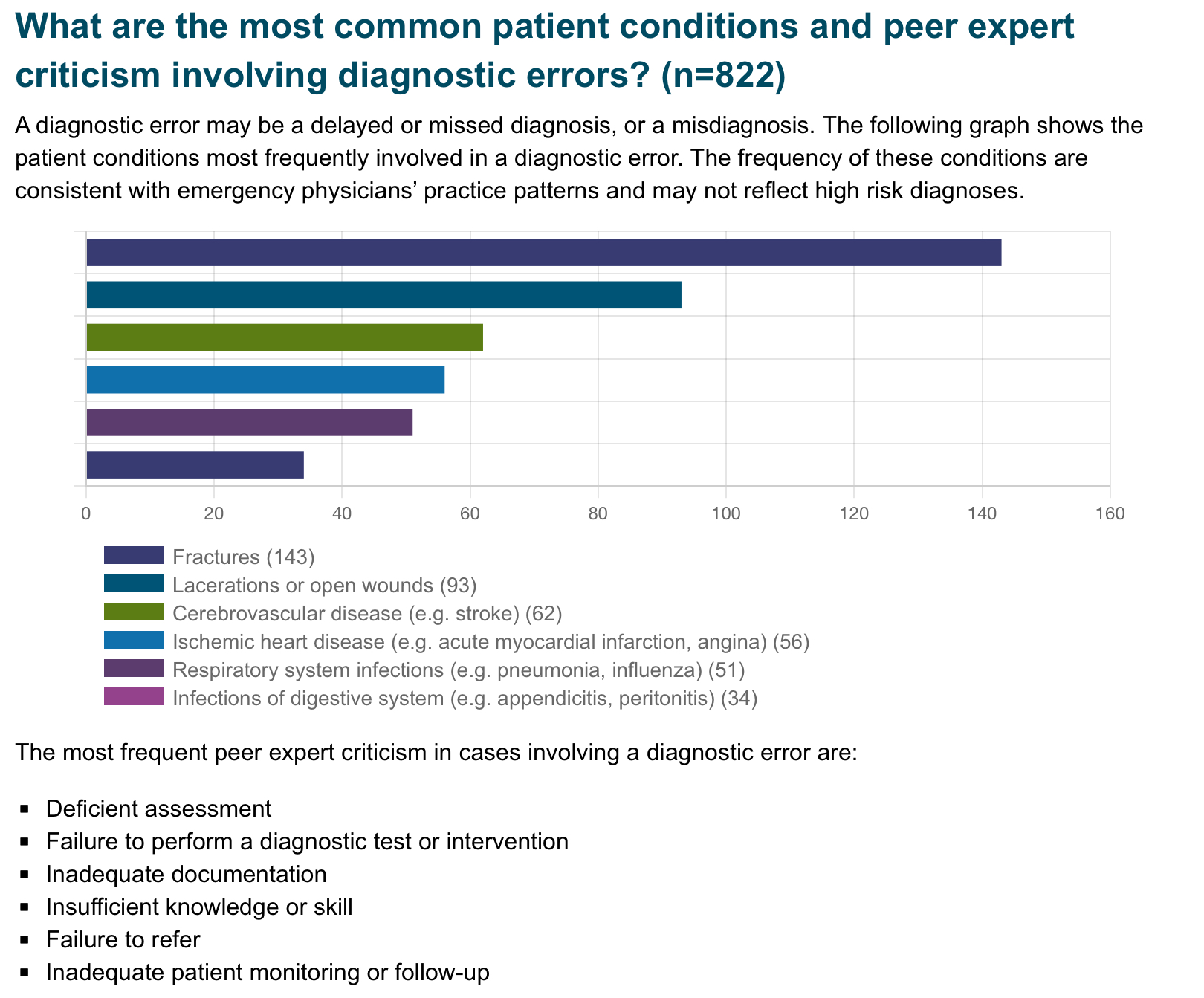
Published November 2023
Category: Administration
Keywords: restraint use (PubMed Search)
Posted: 1/21/2024 by Kevin Semelrath, MD
(Updated: 2/1/2026)
Click here to contact Kevin Semelrath, MD
This study was a retrospective review of restraint use at a level 1 trauma center in the Midwest.
It found the following were factors in a patient encounter associated with an increased risk of restraint usage:
This study found a decreased OR of restraint use with Black or Hispanic race, which was in contrast to other studies
This was a single center, retrospective study, so it was already limited in what it could tell us. In addition, they didn't see the reason for the restraints being ordered in the first place. Nonetheless, it does show that people in certain marginalized groups have a higher likelihood of ending up in restraints. Please think twice when ordering restraints in the ED, especially for behavioral reasons
Published:September 19, 2023DOI:https://doi.org/10.1016/j.annemergmed.2023.08.009
Category: Administration
Posted: 1/6/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Since 2014, Medicare has payed for inpatient services for Medicare patients who’s admitting physician noted that hospital stay required at least 48 hours (measured as 2 midnights) or required specialty care that could not be performed as an out patient. This rule now will apply to Medicare Advantage insurance patients as well. Physicians will need to document their reasoning why a patient’s stay will likely require two midnights.
Jakob Emerson - Updated Friday, December 29th, 2023 Becker’s Payer Issues
Category: Administration
Keywords: Personal growth. (PubMed Search)
Posted: 12/31/2023 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
As the calendar flips to a new year, consider not setting goals or resolutions. Studies show unmet goals or having too many half finished projects leads to increased stress, anxiety and depression. Instead, consider approaching the new year looking for growth, introspection, and striving to achieve excellence. Understanding the why and what motivates you will lead to the correct what and how. Here are some questions to get you thinking about the why. May your New Year be filled with growth and excellence!
Category: Administration
Keywords: boarding, administration, crowding (PubMed Search)
Posted: 11/22/2023 by Mercedes Torres, MD
(Updated: 2/1/2026)
Click here to contact Mercedes Torres, MD
A recently published study of ED APPs, residents, attendings, and nurses attempted to assess clinician's perspectives on how ED boarding impacts ED staff and patients. Authors performed a survey followed by focus group sessions to obtain qualitative insignts from participants.
All respondents associated boarding with feelings of burnout and self-reported poor satisfaction with communication and the process of boarding care.
Several key themes emerged which are outlined below:
This publication highlights the negative workforce and patient safety effects of ED boarding. It amplifies the voices of our colleagues who work towards change to improve both the health of our wrokforce as well as that of our patients and the communities that we serve.
Loke D, et al. Clinicians’ Insights on Emergency Department Boarding: An Explanatory Mixed Methods Study Evaluating Patient Care and Clinician Well-Being. The Joint Commission Journal on Quality and Patient Safety 2023; 000:1-8.
Category: Administration
Keywords: Boarding, Mortality, Crowding (PubMed Search)
Posted: 9/22/2023 by Brent King, MD
(Updated: 2/3/2024)
Click here to contact Brent King, MD
Takeaway Points - A 10 percent reduction in ED volume reduces an ED patient's chance of dying by 24% at 30 days and by 17% at six months
The author of this study conducted a unique natural experiment. They identified cases in which a new emergency department opened near one or more existing departments. Then, they confirmed that the opening of the new department was the only substantial change that occurred (e.g. the staff in the existing EDs were unchanged, the types of complaints were unchanged etc.). The author then determined the impact of the new ED on the existing ED's patient volume and compared death records from the existing EDs before and after the new ED opened.
Simply offloading 10 percent of patients from the existing ED to the new ED, significantly reduced the 30 day and six month risk of death for the existing ED's patients.
The Bottom Line: Many studies have attempted to determine the impact of boarding and to tie boarding to morbitiy and mortality. This author's unique approach to the problem serves to reinforce the need for comprehensive solutions to the problem of patient boarding. Even a modest reduction in emergency department volume has a measureable impact on patient outcomes
Woodworth L. Swamped: Emergency department crowding and patient mortality. Journal of Health Economics, 2020; 70: 102279
Category: Administration
Keywords: Workforce, Diversity, Under-represented minorities (PubMed Search)
Posted: 9/27/2023 by Mercedes Torres, MD
(Updated: 2/1/2026)
Click here to contact Mercedes Torres, MD
Physician Workforce Diversity in EM
Health inequities along racial, ethnic, and socioeconomic lines are a brutal reality of the current state of health care in the US. One way to attempt to address these inequities is to make a concerted effort to diversify our physician workforce. As authors have noted, “Having physicians from diverse backgrounds as colleagues and role models can promote understanding and tolerance in nonminority physicians, ultimately improving medical care for patients who are part of these racial and ethnic groups. Increasing the population of underrepresented minority (URM) physicians in the workforce also directly improves health care for medically underserved populations from all racial and ethnic backgrounds, as studies have shown that physicians from URM backgrounds are more likely to work with these patients.”
Administrators are often tasked with the difficult job of creating a cohesive group of emergency physicians to meet the needs of the community they serve. Strategies to diversify that workforce would benefit from a multi-level approach, including the following:
Small steps can create big changes.
Category: Administration
Keywords: social Z codes (PubMed Search)
Posted: 9/23/2023 by Kevin Semelrath, MD
(Updated: 2/1/2026)
Click here to contact Kevin Semelrath, MD
Since the switch from fee for service to value based care in the US, there has been a marked push to improve our documentation to expand our MDM and differential considerations. We are all here becoming adept at the medical documentation (thanks Dr. Adler!), but may not be adequately documenting our patients' social determinants of health using the social Z codes, a subset of ICD-10 coding language
This study wanted to look at the overall prevelance of social Z code utilization. They used the Nationwide Emergency Department Sample (NEDS), a nationwide database of ED visits, to look at this particular documentation. They examined 35 million (!) ED visits and found that only 1.2% had any social Z code included in the documentation. Given how many resources are linked to a verified (eg documented) need, this raises the idea that if Z codes are better documented, this may lead to increased funding for things like food, housing and transportation insecurities.
Limitations- the authors only examined the ED visits for ICD-10 codes, they didn't specifically look at the notes themselves which may have contained SDOH information. They also found that the social Z codes were more often documented in visits coded for mental health diagnoses, potentially indicating bias. There is also the concern that patients may not want the social z codes included, given the stigma around things like homelessness.
Overall, social Z code documentation could potentially unlock better resources for our patients by documenting a specific need in a population. More will come as documentation continues to evolve.
Molina, MF, et al. Social Risk Factor Documentation in Emergency Departments. Annals of Emergency Medicine, Vol 81, No. 1; January 2023. p38-46
Category: Administration
Keywords: Exercise, health, cardiovascular mortality (PubMed Search)
Posted: 8/12/2023 by Brian Corwell, MD
(Updated: 2/1/2026)
Click here to contact Brian Corwell, MD
The WHO and the US Department of Health and Human Services, among other groups, recommend between 150-300 minutes of moderate intensity or 75 to 150 minutes of vigorous intensity physical activity per week.
This could add up to almost 45 minutes a day!
Who has the time for that?
This is an extremely challenging goal with work and other life responsibilities.
Some recent studies asked whether routinely cramming the recommended weeks’ worth of physical activity into a couple of days, weekend warriors (WW), leads to the same life-extending benefits as distributing the exercise load throughout the week.
In a retrospective analysis of almost 90,000 individuals (56% women), providing a week of accelerometer-based physical activity data: Three activity patterns were compared: active weekend warrior (active WW, ≥150 minutes with ≥50% of total achieved in 1-2 days), active regular (≥150 minutes and not meeting active WW status), and inactive (<150 minutes).
A weekend warrior (WW) pattern of physical activity was associated with similarly lower risks of cardiovascular outcomes (incident atrial fibrillation, myocardial infarction, heart failure, and stroke) compared with more evenly distributed physical activity.
Another large prospective cohort study of over 350,000 US adults (51% women) did not find any significant difference in mortality rates between weekend warriors and regularly active participants. Compared with physically inactive participants, active participants (both weekend warrior and regularly active) had lower all-cause and cause-specific mortality rates.
Take home: Any exercise is better than none. Adults who perform 150 minutes or more of moderate to vigorous physical activity (or 75 minutes of vigorous activity) per week may experience similar health benefits whether the sessions are spread throughout the week or concentrated in a weekend.
Note: Being a weekend warrior can increase the risk of MSK complications and injury..
Future studies should include the use of wearable devices and not rely on self-reporting exercise behavior.
1. Khurshid S, Al-Alusi MA, Churchill TW, Guseh JS, Ellinor PT. Accelerometer-Derived “Weekend Warrior” Physical Activity and Incident Cardiovascular Disease. JAMA. 2023;330(3):247–252.
2. dos Santos M, Ferrari G, Lee DH, et al. Association of the “Weekend Warrior” and Other Leisure-time Physical Activity Patterns With All-Cause and Cause-Specific Mortality: A Nationwide Cohort Study. JAMA Intern Med. 2022;182(8):840–848.
Category: Administration
Keywords: age, attrition, gender, workforce (PubMed Search)
Posted: 7/26/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
In a recent study of emergency physicians (EPs) who left the workforce between 2013 and 2020, authors sought to investigate their age and number of years since residency graduation for males and females.
A total of 25,839 (70.2%) male and 10,954 (29.8%) female EPs were included.
Female gender (adjusted odds ratio 2.30) was significantly associated with attrition from the workforce.
Of those who left the workforce, the median number of years after residency that males left was 17.5, as compared with only 10.5 years for females.
Furthermore, among those who exhibited attrition, one in 13 males and one in 10 females exited clinical practice within 5 years of residency graduation.
As authors emphasize, these data identify widespread gender-based disparities regarding EM workforce attrition that are critical to address to ensure stability, longevity, and diversity in the EP workforce.
Gettel CJ, Courtney DM, Agrawal P, et al. Emergency medicine physician workforce attrition
differences by age and gender. Acad Emerg Med. 2023;00:1- 9. doi:10.1111/acem.14764
Category: Administration
Keywords: racial disparity, substance use disorder (PubMed Search)
Posted: 7/22/2023 by Kevin Semelrath, MD
(Updated: 2/1/2026)
Click here to contact Kevin Semelrath, MD
Substance use disorder is now known to be a function of brain disease and not a moral failure. Patients with substance use disorder are highly complex and often use the ED at a higher frequency than those without the disorder. However, these patients are also frequently the target of implicit bias and stigmatizing behavior from the healthcare team that can lead to worsened outcomes. Add on top of that a racial disparity, and we can see how this group of patients can have really bad health outcomes.
This study looked at the length of time to treatment of patients with SUD, to see if there was a difference within this group based on racial or ethnic differences. It did find that black patients with SUD did wait on average 35% longer in the ED before being seen or treated. This difference was statistically significant.
While this study wasn't designed to identify the causes of such a disparity, it does raise concern for implicit bias being in effect among not only the healthcare workers, but ingrained into the healthcare systems themselves.
Patient's with SUD are a vulnerable group of patients, and black patients with SUD are experiencing a disparity in time to treatment. This should remind us all to seek out ways to remove these biases and disparities from the systems where we work.
Category: Administration
Keywords: predictive rule, EHR, utilization, AI (PubMed Search)
Posted: 6/16/2023 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Author- Steve Schenkel, MD MPP Professor of Emergency Mediciner at UMEM:
A recent Annals of Emergency Medicine Publication (here https://www.annemergmed.com/article/S0196-0644(22)01276-8/fulltext) tested a predictive rule for Likelihood to Occupy an Inpatient Bed associated with a common Electronic Health Record.
At the individual patient level, the score performed ok. Depending on the chosen threshold, it traded off sensitivity and specificity and generally became more accurate the longer the patient was in the ED.
The authors and the associated editorial (here https://www.annemergmed.com/article/S0196-0644(22)01401-9/fulltext) suggest a different, potentially more beneficial use: to allow aggregate prediction of admissions across an entire department and therefore prompt earlier planning to prevent crowding on account of boarding.
The takeaway: Administrative prediction rules oriented toward individual patients may be more meaningfully used to predict resource needs, including in-patient beds, across the ED population.
