Category: Trauma
Keywords: collision, extrication, trauma, motor vehicle, extraction, rapid, spinal immobilization (PubMed Search)
Posted: 11/24/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
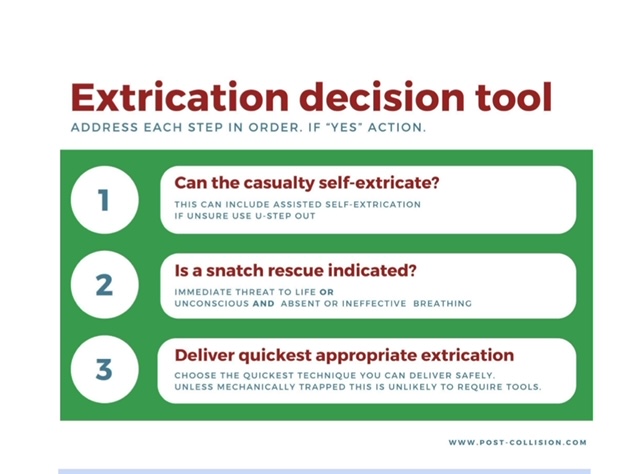
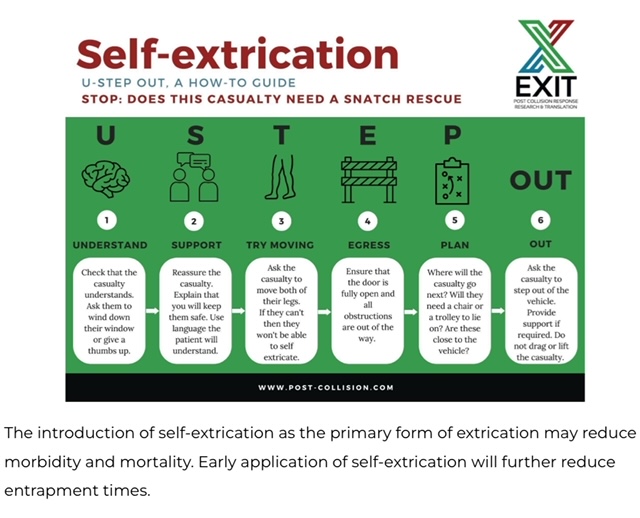
It is important for trauma and emergency care providers to understand what our patients experience prior to arrival in our clean, safe, and structured emergency department. It is also vitally important that we are involved in training and education in the pre-hospital environment. A group in the United Kingdom is challenging the age old “wisdom” that post-motor vehicle crash extrication should be slow, methodical, and work to have absolutely no movement in the spinal canal. Spinal immobilization and slow extrication instead of rapid resuscitation appears to be bad for patients. Based on several of their ground breaking papers they have published a 14 point recommendation of patient extrication post motor vehicle collision. Here are two important tenets they propose. For an in-depth discussion check out November 14, 2024 / CPD, Podcasts, Roadside to Resus.
Category: Trauma
Keywords: Immobilization cervical spine, intubation (PubMed Search)
Posted: 11/21/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
The authors looked at 51 patients intubated with both anterior and posterior cervical collar in place and measured the degree of movement within the spine during intubation. They repeated this process in 51 additional patients with just the posterior portion of the collar in place. They found there was one degree of difference in movement between the two groups. This adds evidence that removing the anterior portion of the collar is safe when intubating trauma patients.
Jo, WY., Choi, JH., Kim, J. et al. Cervical spine motion during videolaryngoscopic intubation using a Macintosh-style blade with and without the anterior piece of a cervical collar: a randomized controlled trial. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02849-4
Category: Trauma
Keywords: Trauma, CT scan, gunshot wound (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 11/17/2024)
Click here to contact Robert Flint, MD
This retrospective study illustrates that the use of CT scanning to identify injury in gun shot wounds to the abdomen is not sensitive or specific enough to obviate the need for laparotomy. “Admission hypotension, abdominal pain and/or peritonitis, evisceration, and a transabdominal trajectory were considered clear indications for laparotomy.” If there is clear indication to go to the OR, stopping in CT does not add any benefit.
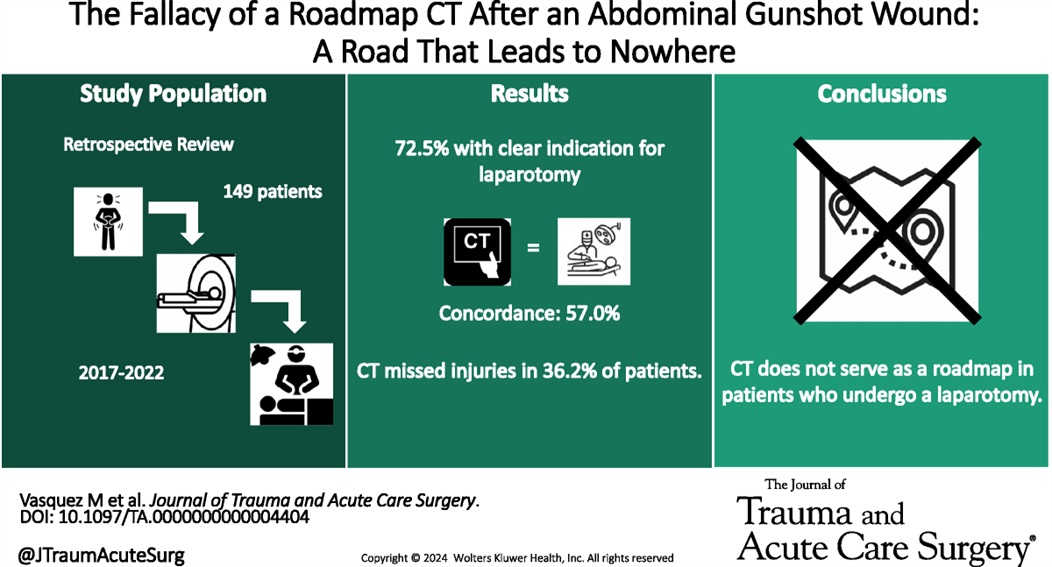
Vasquez, Matthew MD; Dhillon, Navpreet K. MD; Feliciano, David V. MD, FACS, MAMSE†; Scalea, Thomas M. MD, FACS, MCCM
Journal of Trauma and Acute Care Surgery 97(5):p 785-790, November 2024. | DOI: 10.1097/TA.0000000000004404
Category: Trauma
Keywords: ketamine, trauma (PubMed Search)
Posted: 11/14/2024 by Ashley Martinelli
Click here to contact Ashley Martinelli
An out-of-hospital, randomized, placebo-controlled, blinded, parallel group study was conducted in adult patients under the care of the city fire-based emergency medical services and the local level one trauma center. Adult male patients experiencing moderate to severe pain due to traumatic injuries received either 50mg of intranasal ketamine or placebo in addition to fentanyl after randomization in the field by the paramedic (a novel approach). The primary outcome was reduction of pain by 2 points 30 minutes after study drug administration.
199 patients were randomized with 107 receiving ketamine and 92 with placebo. Patients were young (30-40), and had a median weight of 83 kg. Pretreatment pain scores were 10/10 and patients presented to the ED 14 minutes after receiving study medication. The most common injuries were falls, MVC, and GSW. Half of the patients received IV fentanyl but others had IM or IN routes.
Ketamine receipt did not lead to a 2 point reduction in pain scores (36% vs 44.7% p = 0.22). There was no difference in pain at 3 hours, additional medications received, or total amount of analgesia received. Notably, there were no differences in adverse events.
McMullan JT, Droege CA, Chard KM, Otten EJ, Hart KW, Lindsell CJ, Strilka RJ. Out-of-Hospital Intranasal Ketamine as an Adjunct to Fentanyl for the Treatment of Acute Traumatic Pain: A Randomized Clinical Trial. Ann Emerg Med. 2024 Oct;84(4):363-373. doi: 10.1016/j.annemergmed.2024.04.018. Epub 2024 Jun 12. PMID: 38864781.
Category: Trauma
Keywords: Trauma,blood, TXA, prehospital (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 11/11/2024)
Click here to contact Robert Flint, MD
Administration of prehospital TXA was found to improve 28 day mortality and decrease the amount of blood required to be transfused without any increased risk of thromboembolism or seizure. Two grams of TXA was superior to one gram and no TXA.
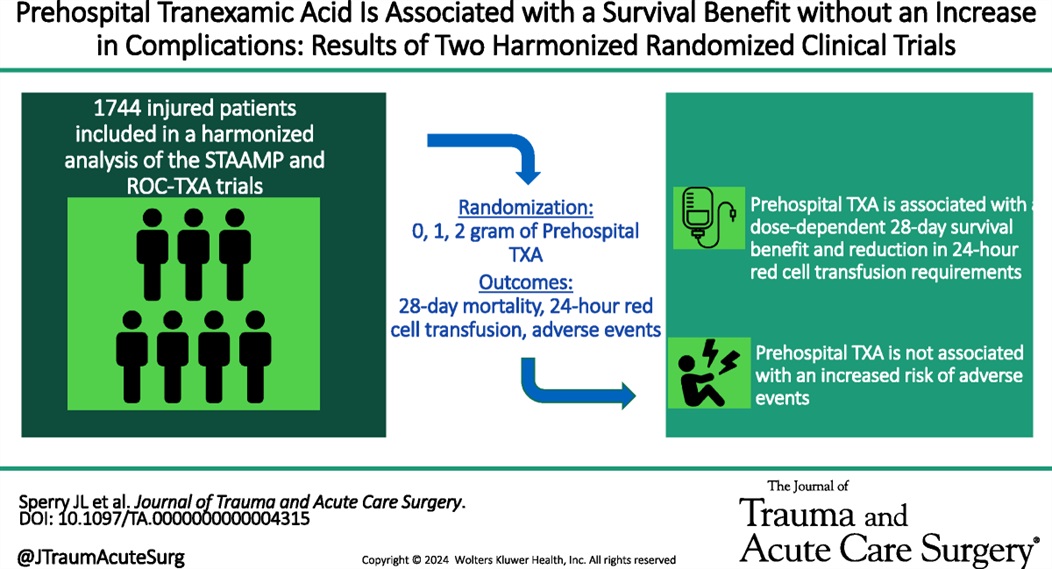
Mazzei, Michael MD, MPH?; Donohue, Jack K. BA?; Schreiber, Martin MD; Rowell, Susan MD, MBA; Guyette, Francis X. MD; Cotton, Bryan MD; Eastridge, Brian J. MD; Nirula, Raminder MD; Vercruysse, Gary A. MD; O'Keeffe, Terence MD; Joseph, Bellal MD; Brown, Joshua B. MD, MSc; Neal, Matthew D. MD; Sperry, Jason L. MD, MPH
Journal of Trauma and Acute Care Surgery 97(5):p 697-702, November 2024. | DOI: 10.1097/TA.0000000000004315
Category: Trauma
Keywords: Trauma, blood, Txa, prehospital (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In this small retrospective study comparing outcomes before and after a prehospital blood administration protocol for penetrating trauma was initiated, the authors found improved survival in those receiving prehospital blood despite a five minute longer on scene time in those receiving blood. Also note TXA was part of the blood protocol but not the control group.
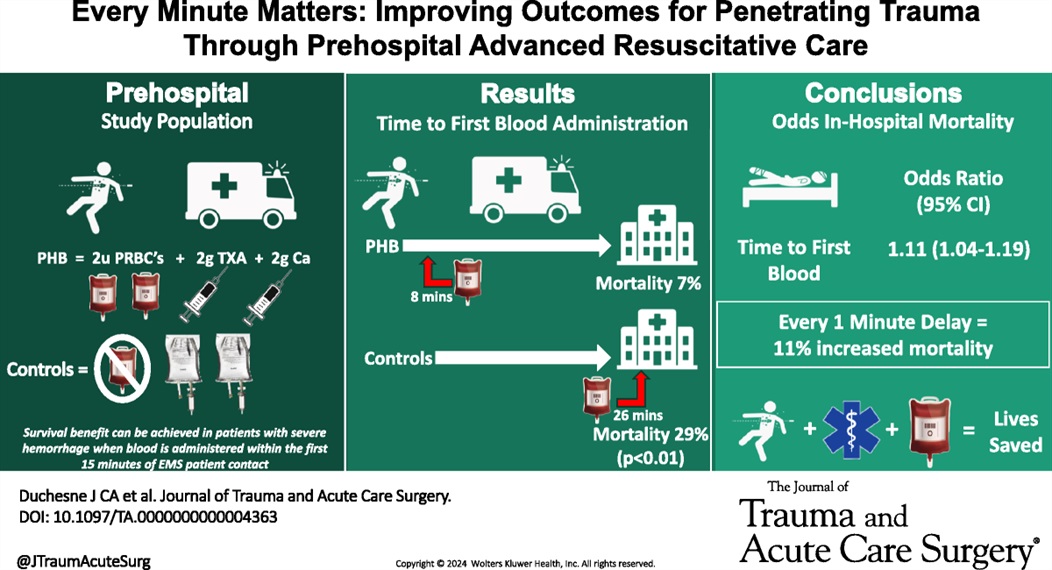
Duchesne, Juan MD; McLafferty, Bryant J. BS; Broome, Jacob M. MD; Caputo, Sydney BS; Ritondale, Joseph P. BS; Tatum, Danielle PhD; Taghavi, Sharven MD, MPH; Jackson-Weaver, Olan PhD; Tran, Sherman MS; McGrew, Patrick MD; Harrell, Kevin N. MD; Smith, Alison MD, PhD; Nichols, Emily MD; Dransfield, Thomas NRP; Marino, Megan MD; Piehl, Mark MD, MPH
Journal of Trauma and Acute Care Surgery 97(5):p 710-715, November 2024. | DOI: 10.1097/TA.0000000000004363
Category: Trauma
Keywords: Repeat, gun violence, Black, revictimization (PubMed Search)
Posted: 11/2/2024 by Robert Flint, MD
(Updated: 11/3/2024)
Click here to contact Robert Flint, MD
This study used the New York State hospital discharge database to look for factors associated with being the victim of repeat gun violence.
Unanswered questions include: is it similar in other areas, what interventions at the patient level could prevent this, what other patient level factors (substance use, etc) are involved, however, this is a good start in looking at this preventable disease.
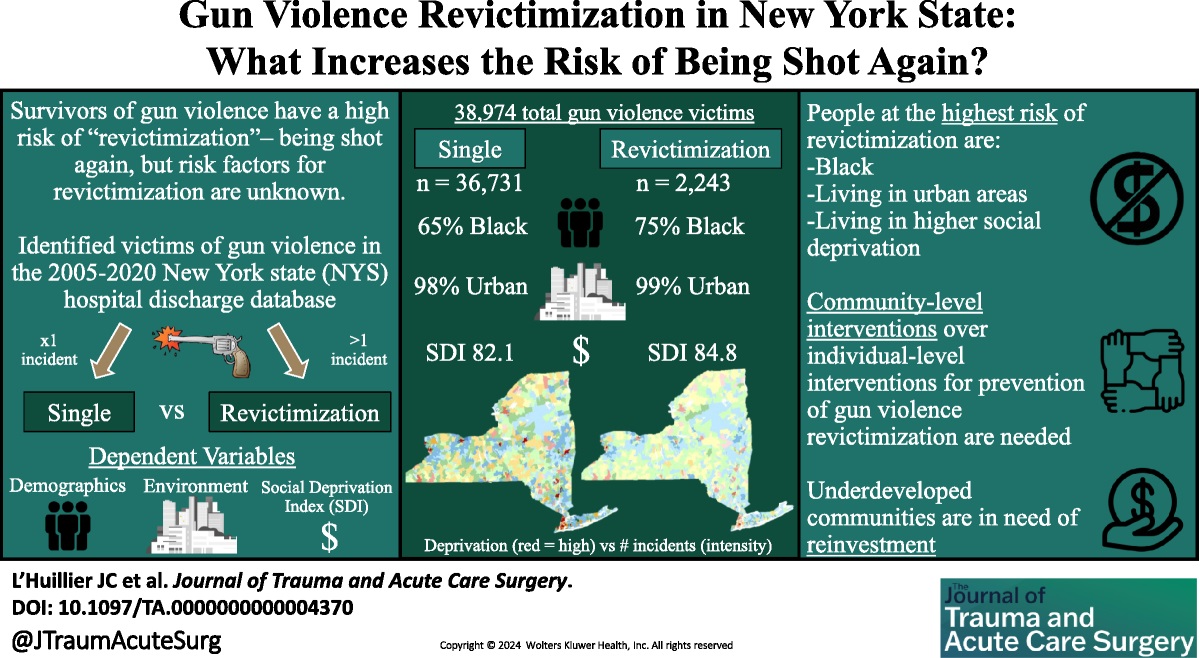
L’Huillier, Joseph C. MD; Boccardo, Joseph D. MS; Stewart, Morgan MUP; Wang, Suiyuan MS; Myneni, Ajay A. MBBS, PhD, MPH; Bari, ASM Abdul MUP; Nitsche, Lindsay J. BS; Taylor, Henry L. Jr PhD; Lukan, James MD, FACS; Noyes, Katia PhD, MPH
Journal of Trauma and Acute Care Surgery 97(4):p 604-613, October 2024. | DOI: 10.1097/TA.0000000000004370
Category: Trauma
Keywords: Adolescent, screening, alcohol, substance use (PubMed Search)
Posted: 11/2/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Recent studies continue to highlight that Black, Native American, female, uninsured and Medicaid patients receive disproportionately more substance use screening when they are trauma patients. The authors of this paper point out that this inappropriate application of screening leads to missed opportunities.
“Screening patients for drug and alcohol use following injury is an evidence-based practice that can trigger wraparound care, such as brief substance use interventions, to prevent reinjury. Adolescents who consume alcohol but are not screened for alcohol use have 2- to 3- fold greater likelihood of reinjury compared with those who were screened and received a brief intervention.”
Sanchez JE, Stey AM. Persistent Inequity Plaguing Pediatric Trauma—An Opportunity for Health Equity Framework. _JAMA Netw Open._2024;7(10):e2436308. doi:10.1001/jamanetworkopen.2024.36308
Category: Trauma
Keywords: Cryopercipitate, mass transfusion hemorrhage (PubMed Search)
Posted: 10/27/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
There is uncertainty if adding cryopercipitate empirically to all mass hemorrhage protocols has any benefit to mortality, need for transfusion, or any other meaningful outcome. This small study suggests it does not and that we should save the addition of cryopercipitate to those with lab proven low fibrinogen levels.
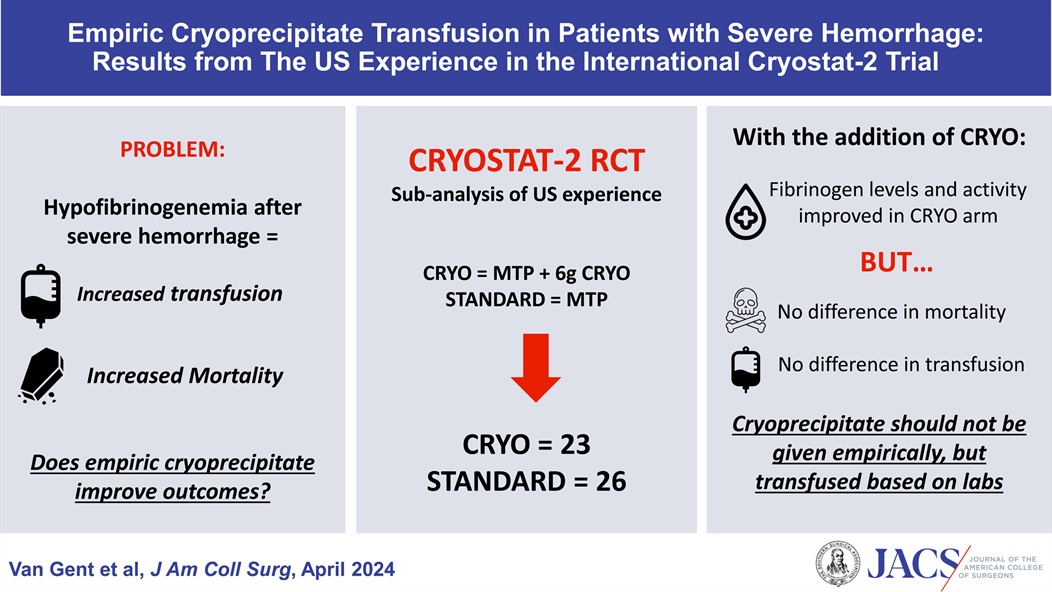
Van Gent, Jan-Michael DO, FACS; Kaminski, Carter W DO; Praestholm, Caroline BS; Pivalizza, Evan G MD; Clements, Thomas W MD; Kao, Lillian S MD, MS, FACS; Stanworth, Simon MD; Brohi, Karim MD; Cotton, Bryan A MD, MPH, FACS
Journal of the American College of Surgeons 238(4):p 636-643, April 2024. | DOI: 10.1097/XCS.0000000000000938
Category: Trauma
Keywords: Neck trauma (PubMed Search)
Posted: 10/24/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
For penetrating neck trauma:
Does it violate the platysma if no, close wound and discharge
If yes, are there any hard signs of injury like enlarging hematoma, air from the wound, difficulty swallowing, blood in the airway, respiratory distress then to the OR
If no, Ct angio of the neck. If negative and no other findings admit for observation or discharge. If positive, to the OR. If equivocal, endoscopy and broncoscopy.
No longer think about the zones of the neck. Treat them all the same.

Category: Trauma
Keywords: Trauma, adrenal crisis, steroids, refractory hypotension. (PubMed Search)
Posted: 10/20/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This article serves as a reminder that trauma can and will precipitate adrenal insufficiency and crisis in those trauma patients who are on steroids pre-injury. Look for prednisone or hydrocortisone as well as autoimmune or rheumatologic diseases on pre-injury medication list and history. Consider the diagnosis in trauma patients with refractory hypotension not responsive to vasopressors. Replacement therapy with hydrocortisone is the therapy.
Volume 62, Issue 6, November–December 2005, Pages 633-637
Brian R. Beeman MD ?, Thomas J. Veverka MD †, Phillip Lambert MD ‡, Dennis M. Boysen Md
Category: Trauma
Keywords: Rectal injury (PubMed Search)
Posted: 10/17/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Rectal injuries are rare and are usually associated with penetrating trauma or significant pelvic fracture from blunt injury. Diagnosis starts with physical exam including inspection for signs of trauma as well as a digital rectal exam looking for blood, bony protuberance and abnormal sphincter tone. Normal digital rectal exam does not exclude injury.
Imagining is important in making the diagnosis.
“Findings on CT associated with rectal injury include a wound tract extending to the rectum, a full-thickness wall defect, perirectal fat stranding, extraluminal free air, intraperitoneal free fluid, and hemorrhage within the bowel wall….A CT with any suggestion of rectal injury should therefore be followed up with rigid proctoscopy to confirm the diagnosis and location of injury, as a combination of CT and endoscopy has a sensitivity of 97% in the diagnosis of rectal injury.”
Fields, Adam MD, MPH; Salim, Ali MD, FACS
Journal of Trauma and Acute Care Surgery 97(4):p 497-504, October 2024. | DOI: 10.1097/TA.0000000000004352
Category: Trauma
Keywords: Rectal injury trauma (PubMed Search)
Posted: 10/13/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Rectal injuries are rare. The majority are secondary to penetrating injuries. Trauma care providers “should have a high clinical suspicion of rectal injury with any missile with a trajectory near the rectum; transpelvic gunshot wounds; stab injuries near the perineum, buttocks, groin, or proximal thighs; or open pelvic fractures. A digital rectal examination with a focus on sphincter tone, presence of blood, palpable defect, or bony protrusion should be carried out. Of note, a normal digital rectal examination does not exclude rectal injury.”
Ct scan with IV contrast (not PO or rectal) is used to identify rectal injuries but will be diagnostic in only 33% of injuries.
Rectal Injury Grading Scale
| Grade | Injury Type | Description of Injury |
|---|---|---|
| I | Hematoma laceration | Hematoma or hematoma without devascularization Partial-thickness laceration |
| II | Laceration | Laceration <50% of circumference |
| III | Laceration | Laceration ?50% of circumference |
| IV | Laceration | Full-thickness laceration with extension into perineum |
| V | Vascular | Devascularized segment |
Fields, Adam MD, MPH; Salim, Ali MD, FACS
Journal of Trauma and Acute Care Surgery 97(4):p 497-504, October 2024. | DOI: 10.1097/TA.0000000000004352
Category: Trauma
Keywords: chest tube, hemothorax, pigtail (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/7/2024)
Click here to contact Robert Flint, MD
The authors reviewed the literature surrounding use of pigtail catheters for traumatic hemothorax and found:
“these data support using percutaneous thoracostomy as a safe and reliable treatment option for hemodynamically stable adult patients with traumatic hemothorax and are backed by major trauma society guidelines including the Eastern Society for the Surgery of Trauma and the Western Trauma Association.1,3 It has the added benefit of the insertion being less painful with the understanding that the percutaneous thoracostomy can always be upsized to a thoracostomy tube.”
Owodunni, Oluwafemi P.Moore, Sarah A.Hynes, Allyson M. et al.
Annals of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: Pigtail (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/6/2024)
Click here to contact Robert Flint, MD
Emergency Medicine Cases offers these excellent tips on pigtail catheters placement. Their video/website is worth a look.
PEARL # 1 – LOCATION/LANDMARK: Minimize skin to pleural distance.
PEARL # 2 – ADEQUATE LOCAL ANESTHESIA: This can obviate the need for sedation.
PEARL #3 – DILATING: Do it in a controlled manner.
PEARL #4 – USING THE OBTURATOR: Needless to say, it is there for a reason.
PEARL #5 – INTERPLEURAL BLOCK: Provide your patient with ongoing analgesia.
PEARL #6 – STOPCOCK AND ONE-WAY VALVE IN THE CORRECT POSITIONS
PEARL #7 – USE A GOOD SUTURE: Don’t let that chest tube come out.
Category: Trauma
Keywords: EMS, c-spine, clearance, (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/5/2024)
Click here to contact Robert Flint, MD
This Canadian study looked at the safety of paramedics using the modified Canadian C-Spine Rule to determine which pre-hospital blunt trauma patients required immobilization. These were MVC and fall patients predominately. Bottom line: appropriately trained paramedics can use the modified Canadian C-Spine rule to clinically clear cervical spines in the field.

| Result of Application | Paramedics’ Interpretation | Investigators’ Interpretation |
|---|---|---|
| Injury | No Injury | Injury |
| --- | --- | --- |
| Immobilization required (N) | 10 | 1,342 |
| Immobilization not required (N) | 1 | 2,668 |
| Sensitivity, % (95% CI) | 90.9 (58.7–99.8) | 90.9 (58.7 to 99.8) |
| Specificity, % (95% CI) | 66.5 (65.1–68.0) | 68.2 (66.7 to 69.7) |
| Positive likelihood ratio, (95% CI) | 2.7 (2.2–3.4) | 2.9 (2.4 to 3.5) |
| Negative likelihood ratio (95% CI) | 0.1 (0.0–0.9) | 0.1 (0.0–0.9) |
Vaillancourt, Christian et al.
Annals of Emergency Medicine, Volume 81, Issue 2, 187 - 196
Category: Trauma
Keywords: Fall, EMS, injury prevention (PubMed Search)
Posted: 9/30/2024 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This meta analysis looked for studies involving community EMS (CEMS) interventions trying to reduce falls. The authors found:
“CEMS fall prevention interventions reduced all-cause and fall-related emergency department encounters, subsequent falls and EMS calls for lift assist. These interventions also improved patient health-related quality of life, independence with activities of daily living, and secondary health outcomes.”
Further, prospective work needs to be done to look at this on a larger scale. We know falls in elderly patients lead to significant morbidity and mortality. This could be one way to improve fall mortality.
Friend TH, Thomas HM, Ordoobadi AJ_, et al_
Community emergency medical services approaches to fall prevention: a systematic review
Injury Prevention Published Online First:22 July 2024. doi: 10.1136/ip-2023-045110
Category: Trauma
Keywords: seizure, head trauma, levetiracetam (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/19/2024)
Click here to contact Robert Flint, MD
The use of seizure prophylaxes in moderate to severe head injury has been recommended for 7 days post-injury. In general, levetiracetam is used for seizure prophylaxes in this group of patients. This study looked retrospectively at high (over 500 mg BID) vs. low (500 mg bid) dosing and found there was no difference in seizure events in either group. Overall 6% of patients had a seizure in this seven day window even with medication given.
Mann A, Livers K, Frick CD, et al. Evaluation of levetiracetam dosing for seizure prophylaxis in traumatic brain injury. Trauma. 2024;0(0). doi:10.1177/14604086241230598
Category: Trauma
Keywords: c-spine, fracture, Burst (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/16/2024)
Click here to contact Robert Flint, MD
Identify this radiographic finding:
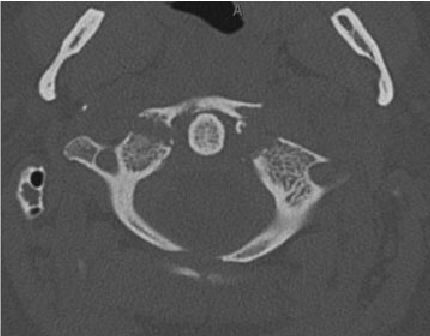
"Jefferson fracture is the eponymous name given to a burst fracture of the atlas. It was originally described as a four-part fracture with double fractures through the anterior and posterior arches, but three-part and two-part fractures have also been described.
50% are associated with other cervical spine injuries
33% are associated with a C2 fracture
25-50% of young children have a concurrent head injury
blunt cerebrovascular injury (BCVI): vertebral artery injury
extracranial cranial nerve injury" 1.
Category: Trauma
Keywords: fracture, spine, x-ray (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/9/2024)
Click here to contact Robert Flint, MD
Identify this injury and other associated injuries:
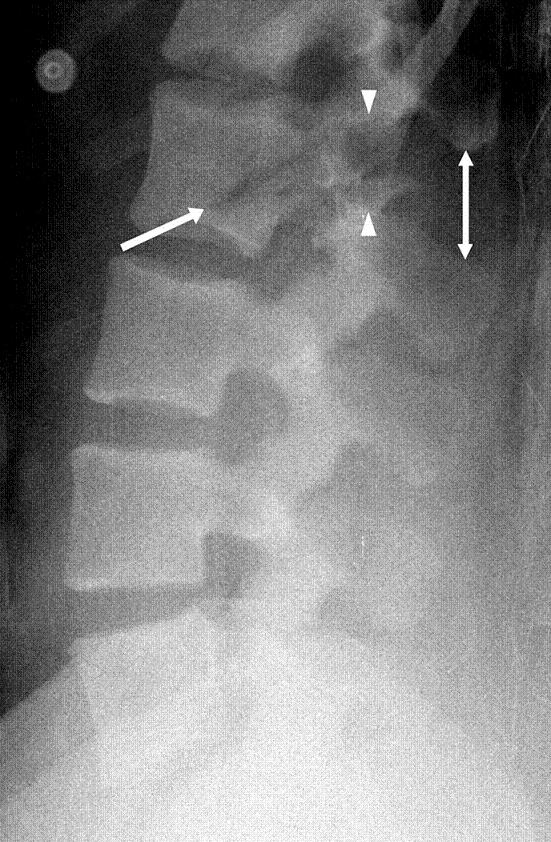
“Chance fractures also referred to as seatbelt fractures, are flexion-distraction type injuries of the spine that extend to involve all three spinal columns. These are unstable injuries and have a high association with intra-abdominal injuries. There is a high incidence of associated intra-abdominal injuries (especially the pancreas, duodenum, and abdominal aorta) that can result in increased morbidity and mortality. Associated intra-abdominal injuries appear to be more common in the pediatric age group with an incidence approaching 50%.” 2.
1.Chance Fracture - Medicalopedia
2. Jones J, Kogan J, Vadera S, et al. Chance fracture. Reference article, Radiopaedia.org (Accessed on 06 Sep 2024) https://doi.org/10.53347/rID-10186
