Category: Trauma
Keywords: brain injury, intubation, best practice, hypoxia, hypotension (PubMed Search)
Posted: 9/6/2025 by Robert Flint, MD
(Updated: 9/7/2025)
Click here to contact Robert Flint, MD
These authors reiterate principles that have been discussed previously regarding intubation in head/brain injured patients.
-Avoid hypoxia with preoxygenation
-Avoid hypotension by fluid resuscitation/vasopressors/blood in the correct clinical setting
-Use hemodynamically neutral induction agents such as Etomidate or Ketamine (it is ok use this in head injured patients!)
-Video laryngoscope gives best first pass success which minimizes hypoxia/raised ICP
-Post-Intubation aim for eucapnia (avoid hyperventilation)
-Use adequate post-intubation sedation to avoid raised ICP
Category: Cardiology
Keywords: Hypertension, treatment, (PubMed Search)
Posted: 9/6/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
From this position statement on management of HTN key points are beta blockers are a second line medication choice, dual therapy in a combination pill is often warranted and primary medications should be thiazides, long acting calcium channel blockers, ACE or Arbs.
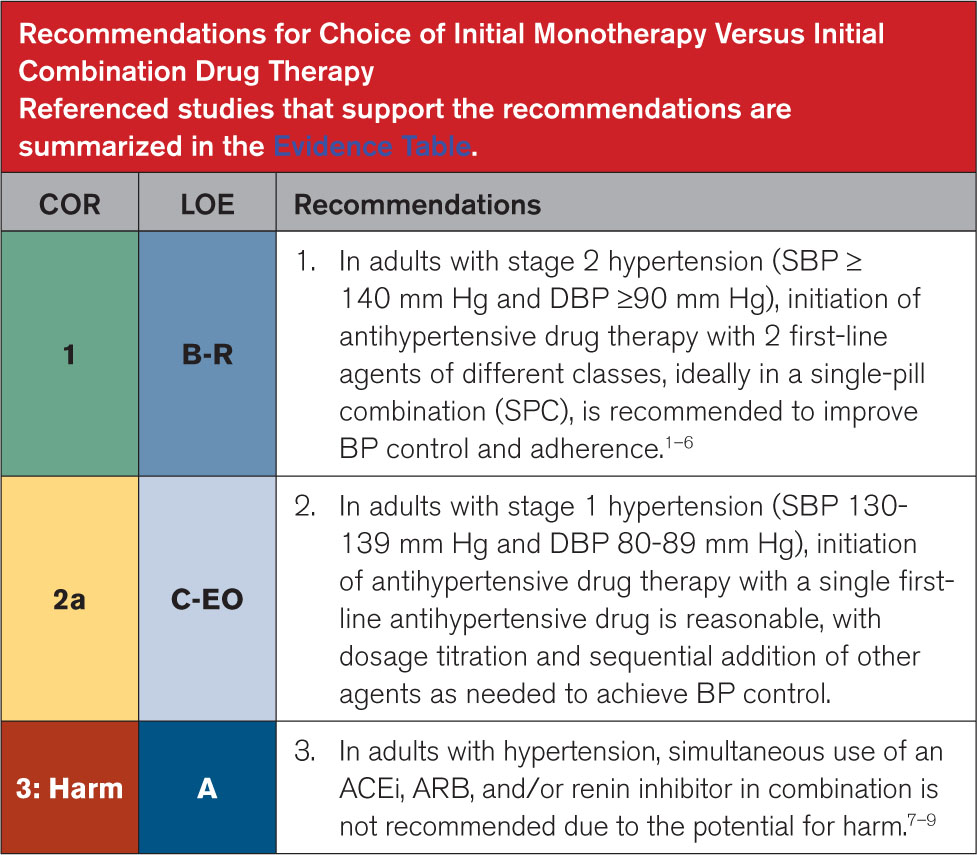
Circulation August 14,2025 https://doi.org/10.1161/CIR.0000000000001356
Category: Neurology
Keywords: CVA, blood pressure management, aggressive, edema (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 8/30/2025)
Click here to contact Robert Flint, MD
While this study is imperfect and may not be measuring patient important outcomes, it does fit with other literature on the topic of intensive blood pressure control in patients with acute ischemic stroke. These patients were randomized to aggressive blood pressure control (SBP 130-140 within 1 hour of TPA administration continued for 72 hours) or the standard SBP <180. Repeat imaging was performed to assess the degree of cerebral swelling that each group developed. There was no difference in swelling between the two groups.
Take away is aggressive blood pressure management in this group of ischemic stroke patients does not seem to be beneficial.
Zhang G, Chen C, Ren X, Zhao Y, Ouyang M, Billot L, Li Q, Wang X, Zhang L, Ong S, Liu L, You S, Lindley RI, Robinson TG, Li G, Chen X, Sui Y, Anderson CS, Song L; ENCHANTED Investigators. Effects of Intensive Blood Pressure Lowering on Brain Swelling in Thrombolyzed Acute Ischemic Stroke: The ENCHANTED Results. Stroke. 2025 Jun;56(6):1388-1395. doi: 10.1161/STROKEAHA.124.049938. Epub 2025 Apr 3. PMID: 40177745.
Category: Geriatrics
Keywords: frailty, geriatrics, troponin, syndrome (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 8/27/2025)
Click here to contact Robert Flint, MD
This editorial reminds us about the use of frailty measures in the geriatric population.
The authors write that frailty “describes a state of vulnerability causing an impaired ability to maintain homeostasis due to reduced physiologic reserve. Frailty is associated with disability, multimorbidity, cognitive impairment, institutionalization, and mortality. **Analogous to troponin testing, frailty assessment has been used to risk stratify older adults.**”
They also remind us that frailty is a syndrome not a disease in and of itself. It impacts how disease affects the patient and should inform our care, but not generate ageism or therapeutic nihilism.
Once frailty is identified, it allows for further assessment looking at the “Geriatric 5M's framework: Mind, Mobility, Medications, Multicomplexity, and Matters Most.”
Is Frailty the Geriatric Troponin?
Jacqueline M. McMillan, Julian Falutz Journal of the American Geriatrics Society
First published: 12 March 2025 https://doi.org/10.1111/jgs.19423
Category: Trauma
Keywords: head injury, geriatric, antithrombotic, CT imaging (PubMed Search)
Posted: 8/25/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
In this retrospective study at 103 hospitals of patients over age 65 who received a head CT:
5948 total patients
3177 (53%) were on at least one anti-thrombotic (warfarin, direct oral anticoag, or anti-platelet agent)
781 (13%) had inter cranial hemorrhage. (ICH)
No form of AC showed an increased risk of ICH.
Risk factors for ICH were: “a high-level fall, a Glasgow coma scale of 14, a cutaneous head impact , vomiting, amnesia, a suspected skull vault fracture or of facial bones fracture”
To me this really begs the question are we ordering head CTs on the right patients? Was there any indication of head injury in these patients or did the mere presence of a patient on AC prompt the imaging order? More work should be done to prevent needless imaging cost, patient time in the emergency department and radiologist work load/turn around time.
Benhamed A, Crombé A, Seux M, Frassin L, L'Huillier R, Mercier E, Émond M, Millon D, Desmeules F, Tazarourte K, Gorincour G. Association between antithrombotic medications and intracranial hemorrhage among older patients with mild traumatic brain injury: a multicenter cohort study. Eur J Emerg Med. 2025 Jul 1. doi: 10.1097/MEJ.0000000000001246. Epub ahead of print. PMID: 40590793.
Category: Trauma
Keywords: chest tube, tube thoracostomy, hemothorax, volume (PubMed Search)
Posted: 8/23/2025 by Robert Flint, MD
(Updated: 8/24/2025)
Click here to contact Robert Flint, MD
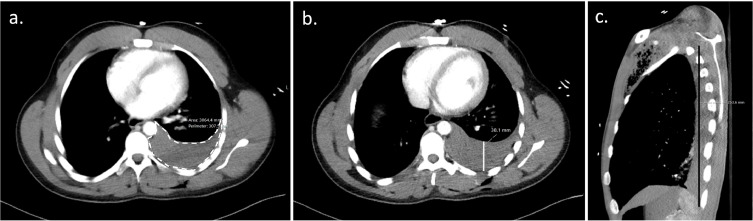
Over 300 ml of blood on a chest CT in a traumatically injured patient requires a tube thoracostomy. How do you calculate 300 ml of blood on a chest CT?
You use Mergo's formula.
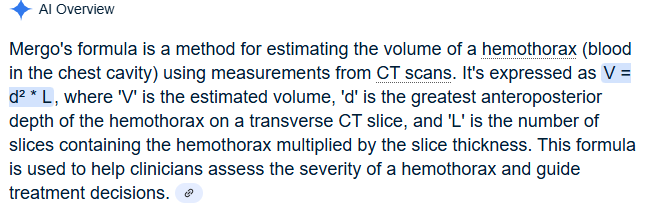
Image B the AP line is what would represent d
1. Blank JJ, de Moya MA. Traumatic pneumothorax and hemothorax: What you need to know. J Trauma Acute Care Surg. 2025 Jul 3. doi: 10.1097/TA.0000000000004692. Epub ahead of print. PMID: 40604368.
2. CT-based pleural effusion volume estimation formula demonstrates low accuracy and reproducibility for traumatic hemothorax
Tewkesbury, Grace et al. Injury, Volume 55, Issue 1, 111112
Category: Trauma
Keywords: Pneumothorax, cheat tube, indication (PubMed Search)
Posted: 8/17/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This review article answers the basic question: when does a traumatic pneumothorax require tube thoracostomy?
“A pneumothorax greater than 20% of the thoracic volume on chest x-ray or greater than 35 mm on CT, measured radially from the chest wall to the lung parenchyma, should be treated with tube thoracostomy. Pneumothoraces smaller than this may be observed; approximately 10% of these will fail observation and require tube thoracostomy treatment.”
Blank JJ, de Moya MA. Traumatic pneumothorax and hemothorax: What you need to know. J Trauma Acute Care Surg. 2025 Jul 3. doi: 10.1097/TA.0000000000004692. Epub ahead of print. PMID: 40604368.
Category: Trauma
Keywords: Gunshot, ptsd, reinjury (PubMed Search)
Posted: 8/10/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This paper outlines the long term effects of surviving a gunshot wound. The authors conclude:
“Firearm injury survivors frequently experience chronic pain, nerve injury, retained bullet fragments that may cause lead toxicity, physical limitations, and PTSD and are at risk for reinjury. In addition to supportive medical and psychiatric care, survivors of firearm injury may benefit from health care–based violence intervention programs.”
Strong BL, Lauerman MH, Scalea TM. Sequelae and Care After Firearm Injury. JAMA. Published online July 23, 2025. doi:10.1001/jama.2025.10498
Category: Trauma
Keywords: Hypothermia, trauma, mortality (PubMed Search)
Posted: 8/3/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Looking at a trauma database of over 3 million patients, 1% presented with prehospital hypothermia (<35 degrees C). These patients had longer hospital stays, higher resource utilization and higher mortality. Even isolated head injury patients with hypothermia had worse outcomes. Rewarming did increase survival slightly for all patients.
Take away: rewarm hypothermic trauma patients as soon as possible to improve mortality.
Anna Mary Jose, Aryan Rafieezadeh, Muhammad Zeeshan, Jordan Kirsch, Gabriel Froula, Kartik Prabhakaran, Bardiya Zangbar,
Hypothermia on admission predicts poor outcomes in adult trauma patients,
Injury,
Volume 56, Issue 5,
2025,
112076,
ISSN 0020-1383,
https://doi.org/10.1016/j.injury.2024.112076
Category: Geriatrics
Keywords: Anxiety, older, risk (PubMed Search)
Posted: 8/2/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
A scoping review of the literature regarding anxiety in older patients found the follow areas had the biggest impact on anxiety level:
“The variables most strongly associated with anxiety—either as risk or protective factors—are age, female gender, physical activity, physical health conditions, depression, perceived and family support, and social participation. New variables linked to anxiety include body mass index (BMI) and dietary habits.”
Asking questions related to these areas can give you a better picture of your patient’s risk for anxiety.
Geriatrics 2025, 10(4), 83; https://doi.org/10.3390/geriatrics10040083
Category: Trauma
Keywords: Gun shot, antibiotics, prophylaxis, fracture (PubMed Search)
Posted: 7/31/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Looking at 140 patients retrospectively who had abdominal gunshot wounds with associated fractures, prophylactic antibiotics longer than three days did not offer any benefit in preventing fracture infection. Only two patients experienced fracture related infections and 65 total experienced any infection related complications.
From and ED standpoint, it appears reasonable to give a dose of antibiotics in this very rare subset of gunshot wound patients.
Kahler D, DeWitte N, Thompson M, Rehman S, Anderson J. Prophylactic antibiotics in gunshot fractures with concomitant bowel injury to prevent fracture-related infections and other infectious complications. Injury. 2025 Jun;56(6):112304. doi: 10.1016/j.injury.2025.112304. Epub 2025 Apr 8. PMID: 40279804.
Category: Geriatrics
Keywords: Geriatric l, trauma, triage (PubMed Search)
Posted: 7/30/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This prospective cohort study from Germany found an under triage rate of 58% of trauma patients over 70 years presenting to 12 trauma centers. One area that consistently lead to undertriage was not using a systolic blood pressure under 110 as a criteria for trauma team activation.
The older cohort had 3 times the mortality than younger, were more likely not to arrive by helicopter and mechanism was more commonly ground level fall. This study echos many others in USA and Australia. Better trauma triage criteria are needed for older patients.
Koch, D.A., Becker, L., Schweigkofler, U. _et al._Undertriage in geriatric trauma: insights from a multicentre cohort study. Scand J Trauma Resusc Emerg Med 33, 123 (2025). https://doi.org/10.1186/s13049-025-01432-0
Category: Trauma
Keywords: Bcvi, stroke, CVA (PubMed Search)
Posted: 7/28/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
A retrospective, single Australian center review of 300 patients who had blunt cerebral vascular injuries found:
-9.8% had an inpatient CVA
-Most occurred in first 72 hours
-Those receiving no anti coagulation or antiplatelets had 28% CVA incidence.
-Those treated had a 3.6% CVA incidence (anti platelets were better than anti coagulation)
-Carotid artery injury was less common than vertebral artery but had higher frequency of CVA
-associated factors: low GCS, rib fractures, severe trauma
Take away: non-treatment of blunt cerebral vascular injuries had higher inpatient stroke risk. Antiplatelet agents such as aspirin and Clopidogrel performed better than anticoagulants
Stanislaus V, Zhang WW, Chen Z, et al. Inpatient stroke outcomes in patients with blunt cerebrovascular injuries according to risk factors and treatment. Trauma. 2025;0(0). doi:10.1177/14604086251333569
Category: Trauma
Keywords: Mussed injuries, trauma, tertiary survey, (PubMed Search)
Posted: 7/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This paper looked at the literature regarding missed injuries in trauma patients. Missed injuries was defined as an injury discovered after the patient was discharged. Most of the missed injuries and causes are not novel but are worthy of remembering.
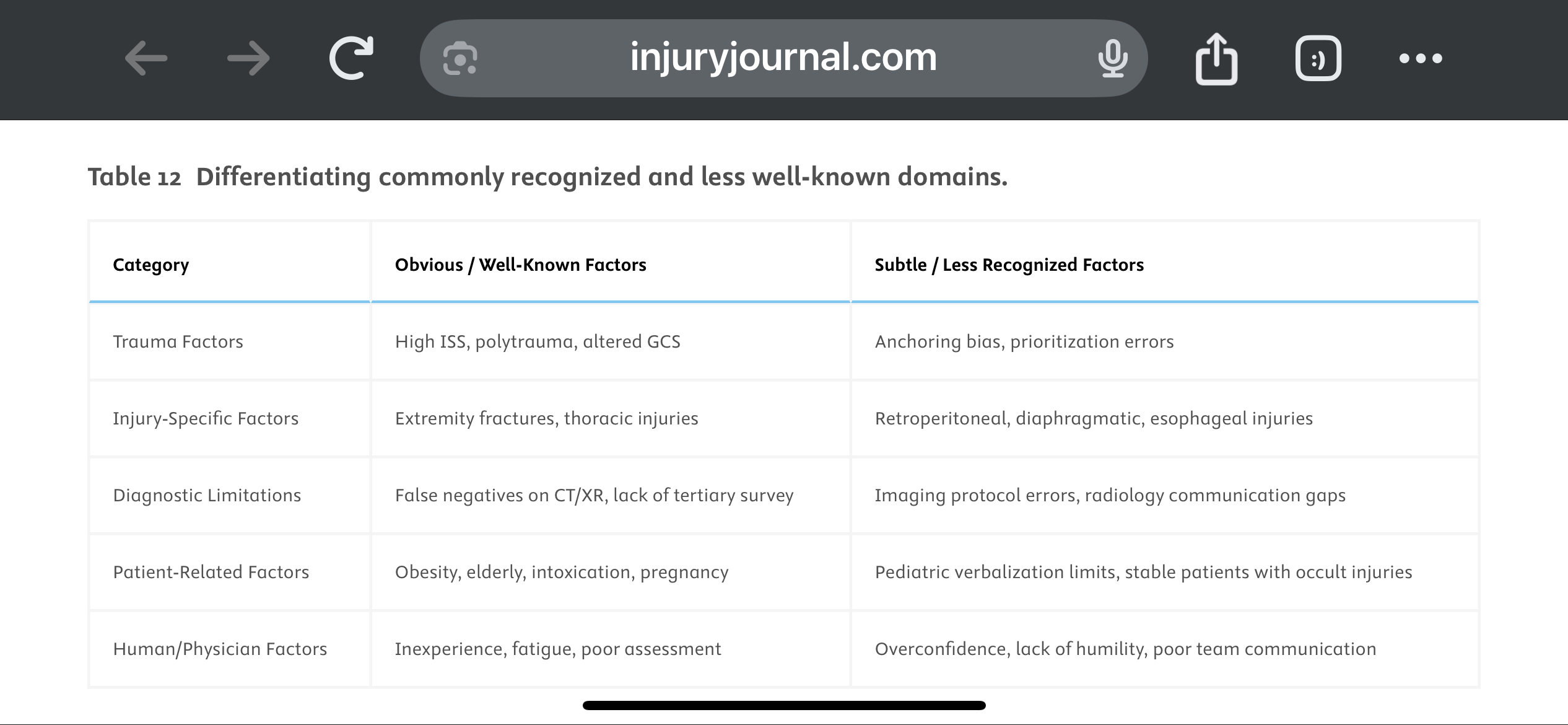
They suggest a Trauma Tertiary Survey helps prevent missed injury. “Tertiary Survey (TTS), which includes a thorough in-hospital re-examination and a review of diagnostic investigations within the first 24 h, has been shown to significantly reduce the occurrence of missed injuries (1–9 %) in severe trauma patients found after a primary and secondary survey.” This concept is similar to a discharge time out in emergency medicine where all data is reviewed, viral signals are confirmed normal and a team discharge is performed.
The paper offers these suggestions to avoid missed injuries:
1.
Standardize Tertiary Trauma Surveys (TTS).
2.
Be Cognizant of Cognitive Biases (e.g., Anchoring Bias).
3.
Repeat Imaging When Clinically Indicated.
4.
Use Protocolized Imaging Techniques (CT/MRI).
5.
Ensure Radiology-Trauma Communication.
6.
Prioritize High-Risk Populations.
7.
Implement Peer Review or Double-Check Systems.
8.
Encourage a Culture of Collaboration and Humility.
9.
Limit Provider Fatigue and Overload.
10.
Create Tailored Checklists for Subtle Injuries.
Vieira, Lucas Fontenelle et al.
Injury, Volume 56, Issue 8, 112600
Category: Trauma
Keywords: TBI, management, parameters (PubMed Search)
Posted: 7/20/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Outcomes in traumatic brain injury are improved when physiologic homeostasis is achieved as soon as possible after injury. Here are the American College of Surgeons’ recommendations. Note SBP over 110 and a hemoglobin over 7. A study looking at a more liberal transfusion target showed worse ARDS and no mortality benefit.
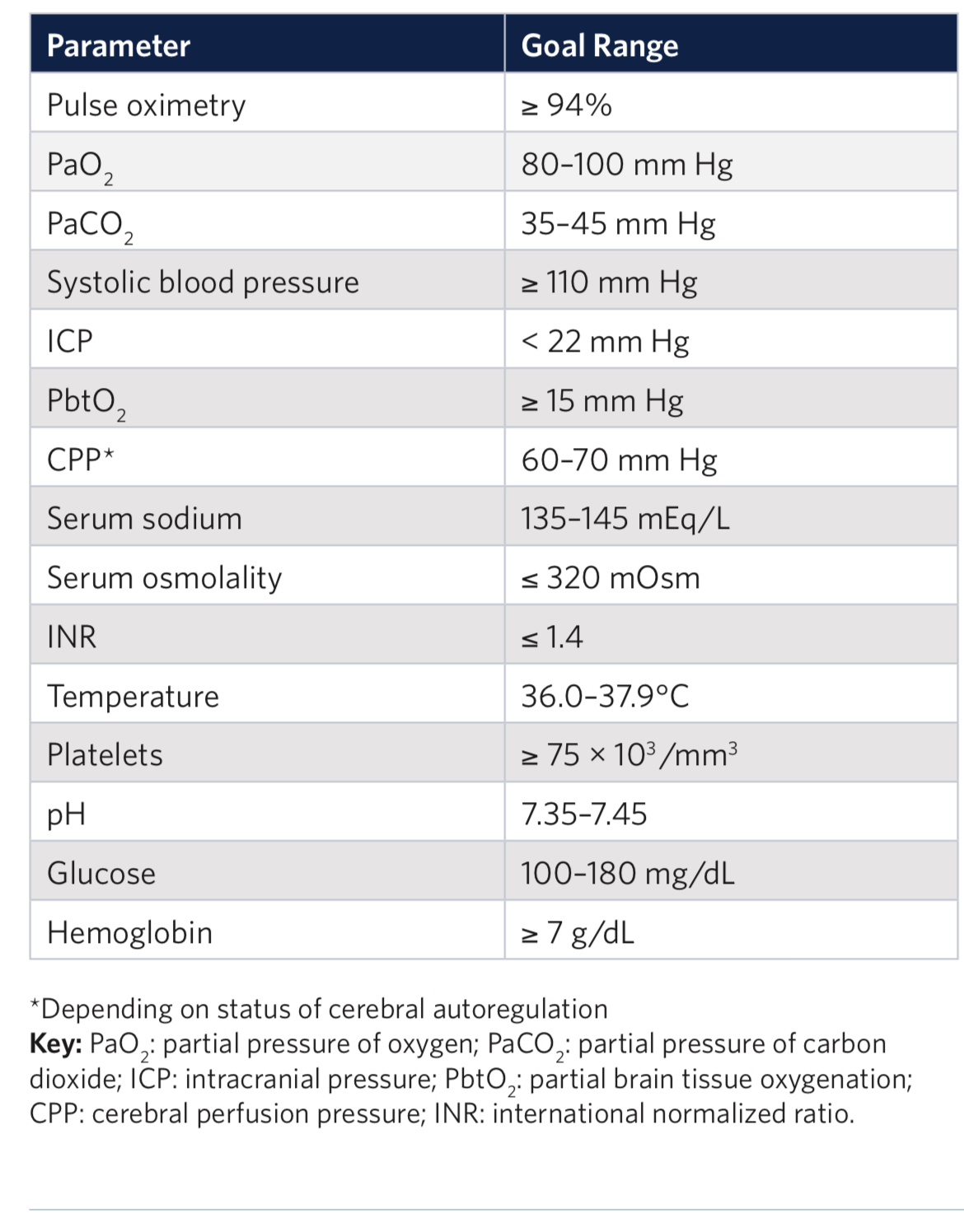
2. Liberal or Restrictive Transfusion Strategy in Patients with Traumatic Brain Injury
Authors: Alexis F. Turgeon, M.D. https://orcid.org/0000-0001-5675-8791, Dean A.Fergusson, Ph.D., Lucy Clayton, M.Sc., Marie-Pier Patton, M.Sc., Xavier Neveu, M.Sc., Timothy S. Walsh, M.D., Annemarie Docherty, M.D., Ph.D., +48 , for the HEMOTION Trial Investigators on behalf of the Canadian Critical Care Trials Group, the Canadian Perioperative Anesthesia Clinical Trials Group, and the Canadian Traumatic Brain Injury Research Consortium*
June 13, 2024N Engl J Med 2024;391:722-735DOI: 10.1056/NEJMoa2404360VOL. 391 NO. 8
Category: Geriatrics
Keywords: Geriatric, critical care, vasopressors. (PubMed Search)
Posted: 7/12/2025 by Robert Flint, MD
(Updated: 7/14/2025)
Click here to contact Robert Flint, MD
An open label pragmatic study in 29 Japanese hospitals randomized septic shock patients over age 65 to either a high (MAP 80-85) or control (65-70) group. They then looked at all cause 90 day mortality. The study was stopped early due to a significantly higher percentage of mortality in the higher MAP group.
The study isn’t blinded and is only done in one country, however it does raise the question of what is the ideal MAP for older septic shock patients.
Endo A, Yamakawa K, Tagami T, Umemura Y, Wada T, Yamamoto R, Nagasawa H, Takayama W, Yagi M, Takahashi K, Kojima M, Narita C, Kazuma S, Takahashi J, Shiraishi A, Todani M, Nakane M, Nagata T, Tanaka S, Yokokawa Y, Takahashi K, Ishikita H, Hisamune R, Sasaki J, Muramatsu KI, Sonobe H, Minami K, Hoshi H, Otomo Y; OPTPRESS trial investigators. Efficacy of targeting high mean arterial pressure for older patients with septic shock (OPTPRESS): a multicentre, pragmatic, open-label, randomised controlled trial. Intensive Care Med. 2025 May;51(5):883-892. doi: 10.1007/s00134-025-07910-4. Epub 2025 May 13. PMID: 40358717; PMCID: PMC12130109.
Category: Trauma
Keywords: Pedestrian, fatality, injury, cyclist (PubMed Search)
Posted: 7/12/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study from Great Britain compared fatalities for pedestrians and cyclist struck by motor vehicles based on vehicle body type. They found :
“We conclude that in Great Britain, being hit by an SUV as opposed to a passenger car increases injury severity among pedestrians and cyclists, with the strongest effect in children.“
Goodman, Anna, Phil Edwards, and Anthony A. Laverty. 2025. “Do Sports Utility Vehicles (SUVs) Cause More Severe Injuries to Pedestrians and Cyclists than Passenger Cars, in the Case of a Crash? Findings from Great Britain, 2004-2023.” Findings, July. https:/?/?doi.org/?10.32866/?001c.141647.
Category: Geriatrics
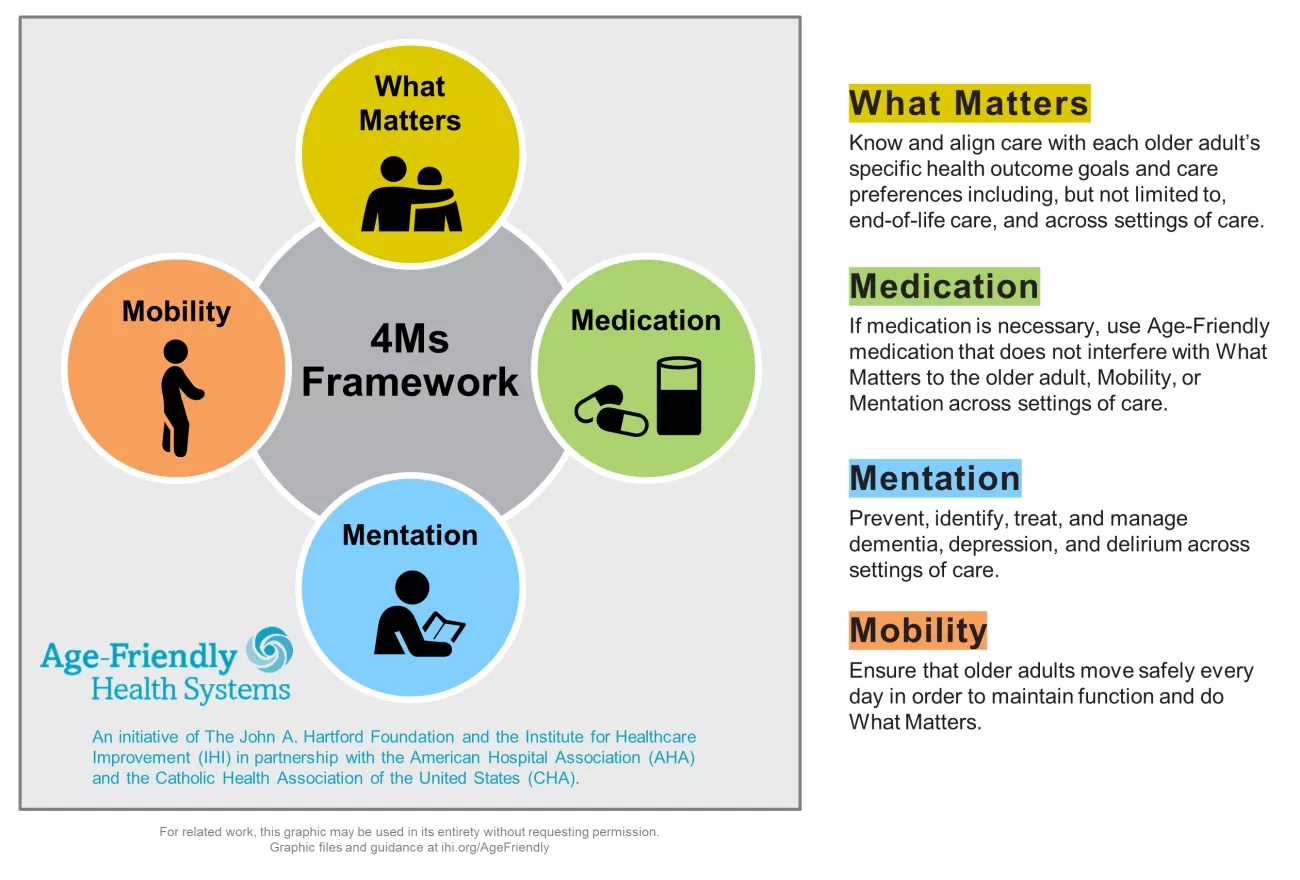
Keywords: Age friendly, geriatric, healthcare, quality improvement (PubMed Search)
Posted: 7/6/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
In mid-2024 the Center for Medicare and Medicaid Services introduced a new quality measure entitled Age Friendly Hospital Measure. The initial phase went into effect 1/1/25. It is built around programs from the American College of Surgeons, the American College of Emergency Physicians as well as the Institute for Healthcare Improvement (IHI). It is modeled around the IHI’s 4M Framework.
Category: Trauma
Keywords: Shock index, transfusion, hypotension (PubMed Search)
Posted: 7/5/2025 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
These authors looked at 5958 trauma patients arriving at their trauma center with a systolic blood pressure greater than 90. They calculated shock index (heart rate /sbp) for all of these and then looked at who received a blood transfusion within one hour of arrival. 211 patients received blood in that time frame. “Patients were stratified by SI using the following thresholds: ? 0.7, > 0.7 to 0.9, > 0.9 to 1.1, > 1.1 to 1.3, and > 1.3.”
“A main effect was observed for shock index with increased risk for required transfusion for patients with admission shock index >0.7 (P < 0.001). In comparison to shock index of ? 0.7, odds ratios were 2.5(1.7 - 3.8), 8.2(5.4 - 12.2), 24.9(15.1 - 41.1), 59.0(32.0 - 108.6) for each categorical increase in SI.”
Lin TM, Memon AM, Reeson EA, Tolan GC, Low TM, Kupanoff KM, Huang DD, Jones MD, Czarkowski BR, Soe-Lin H, Bogert JN, Weinberg JA. Shock index identifies compensated shock in the 'Normotensive' trauma patient. Injury. 2025 May 8:112419. doi: 10.1016/j.injury.2025.112419. Epub ahead of print. PMID: 40379507.
Category: Trauma
Keywords: facial fracture, transfer, guidelines (PubMed Search)
Posted: 6/29/2025 by Robert Flint, MD
(Updated: 7/2/2025)
Click here to contact Robert Flint, MD
Based on a review of 511 patients transferred to a level one trauma center for evaluation of facial fractures, this group developed the Facial Fracture Transfer Guidelines. they found that over half of the patients transferred to them did not require intervention and were discharged within 6 hours. These guidelines are meant to decrease unneeded transfers yet provide appropriate care to those with traumatic facial injuries.
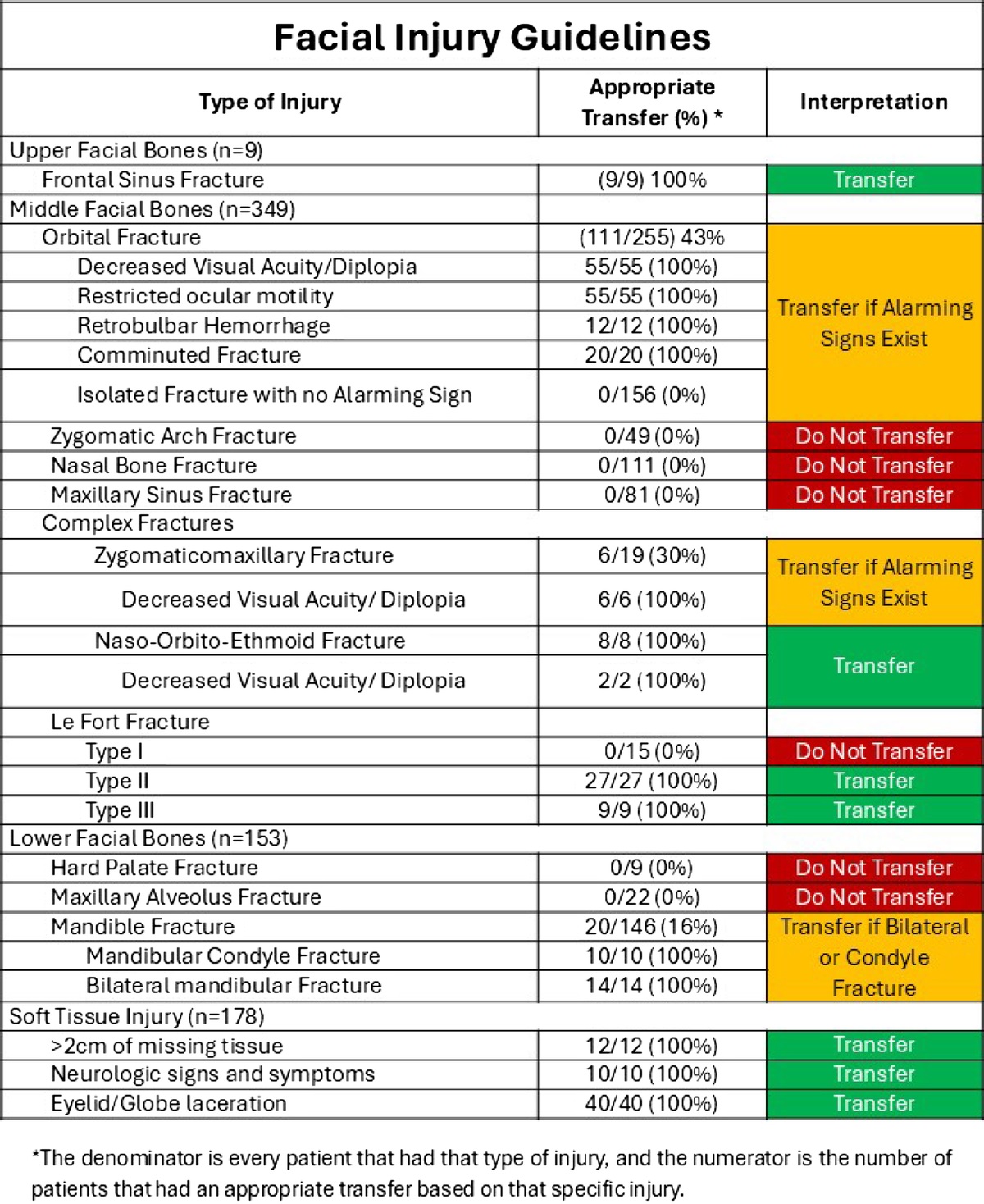
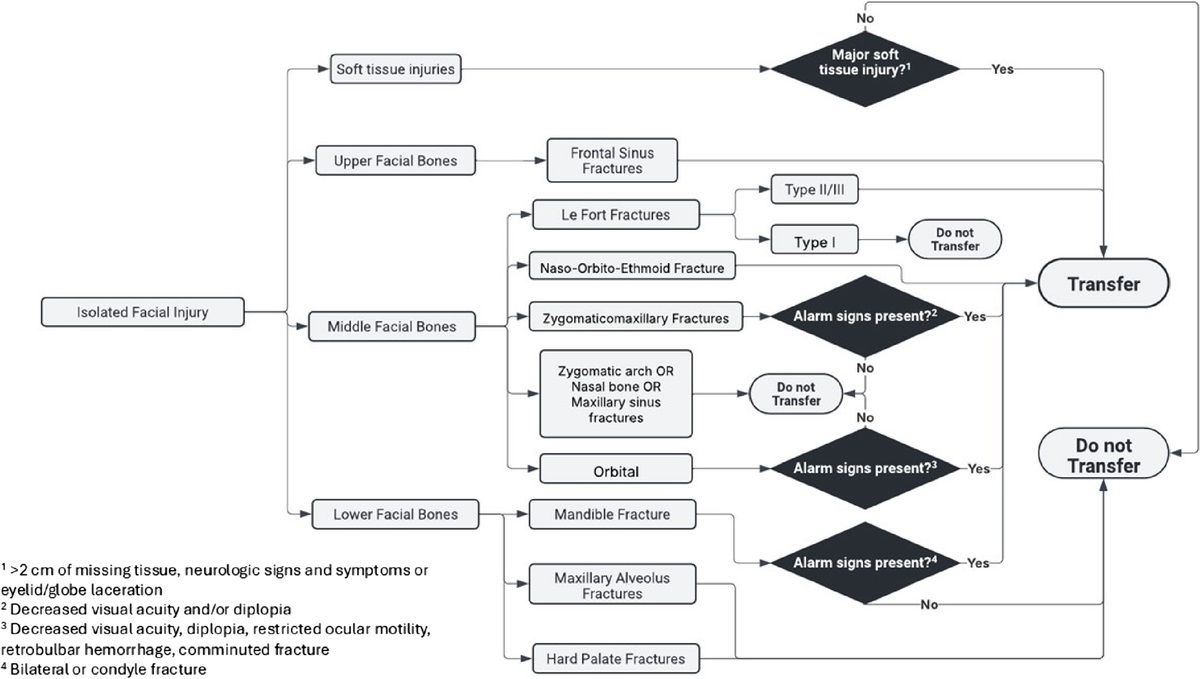
Castillo Diaz, Francisco MD; Anand, Tanya MD, MPH, FACS; Khurshid, Muhammad Haris MD; Kunac, Anastasia MD, FACS; Al Ma'ani, Mohammad MD; Colosimo, Christina DO, MS, FACS; Hejazi, Omar MD; Ditillo, Michael DO, FACS; Magnotti, Louis J. MD, MS, FACS; Joseph, Bellal MD, FACS. Look me in the face and tell me that I needed to be transferred: Defining the criteria for transferring patients with isolated facial injuries. Journal of Trauma and Acute Care Surgery ():10.1097/TA.0000000000004651, May 9, 2025. | DOI: 10.1097/TA.0000000000004651
