Category: Critical Care
Posted: 9/30/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
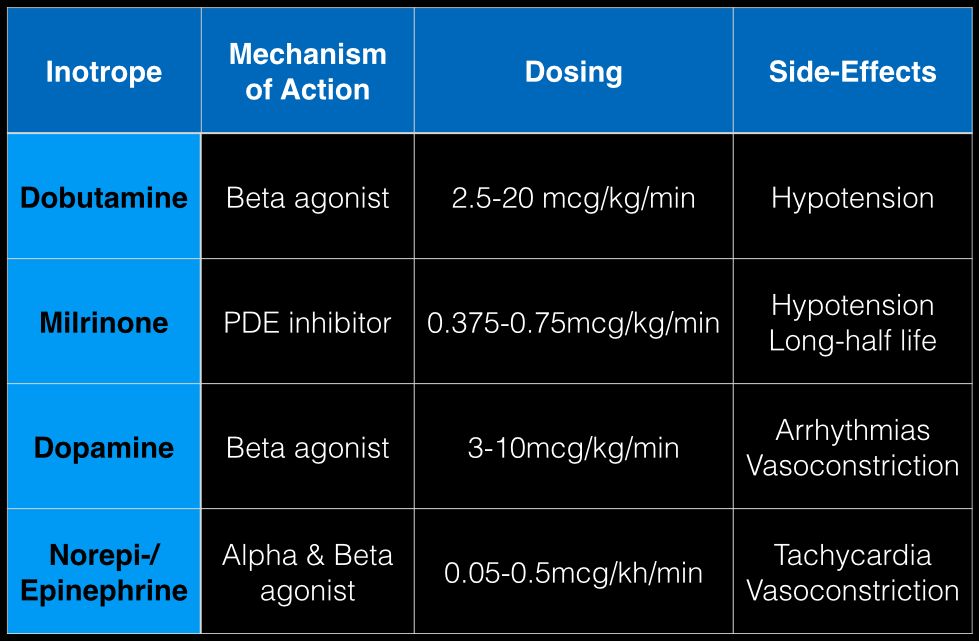
The last Back to the Basics post discussed the use of vasopressors to improve hemodynamics by increasing arterial (and venous) tone. This time we’ll discuss the use of agents to increase inotropy for patients with severe systolic dysfunction / failure.
Dobutamine: a direct b1 and b2-receptors agonist. It has no peripheral vasoconstrictor properties, so if blood pressure increases it occurs secondary to increased cardiac output. Unfortunately, blood pressure may be decreased in some patients due to its peripheral vasodilatory effects; in these cases it may need to be used with a vasopressor.
Milrinone: augments contractility by increasing intracellular Ca levels via cellular phosphodiesterase inhibition. Because it does not work on beta-receptors, it might be preferred for patients taking beta-blockers requiring inotropic support. It may cause peripheral vasodilation and hypotension, but this may be a benefit if pulmonary artery pressure is elevated as reductions in pulmonary artery pressure lead to improvements in right ventricular function. It has a long-half life and should be avoided in patients with renal impairment.
Dopamine: chemical precursor to norepinephrine and technically a vasopressor. At moderate doses (3-10 mcg/kg/min) it works on beta-receptors to increase myocyte contractility. At higher doses works primarily as a vasopressor, which may reduce cardiac output due to higher afterload.
Norepinephrine/epinephrine: has alpha and beta properties that lead to increased peripheral vasoconstriction, but also increases inotropy and chronotropy (faster heart rate)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)a
