Category: Critical Care
Keywords: DKA (PubMed Search)
Posted: 8/13/2024 by Jordan Parker, MD
Click here to contact Jordan Parker, MD
Diabetic ketoacidosis (DKA) is a serious condition that carries the risk of significant morbidity and mortality if not managed appropriately. Typically managed with an infusion of regular insulin, IV fluids, and electrolytes, there is evidence to support treatment of mild to moderate DKA with a subcutaneous (SQ) regimen using a combo of fast-acting and long-acting insulin instead, decreasing the need for ICU admission without increasing adverse events [1].
What patients?
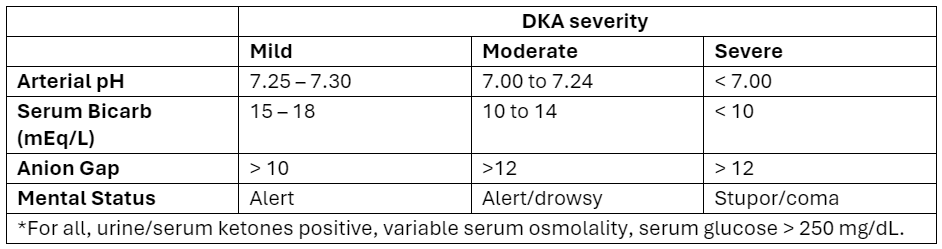
Adapted from Abbas et al.
How to manage?
Initial dose
Subsequent dosing:
If serum glucose is > 250 mg/dL
If serum glucose is < 250 mg/dL
Bottom Line
DKA management with a SQ insulin protocol is a reasonable approach for patients with mild to moderate DKA, is supported by the American Diabetes Association [5], and can be particularly helpful in this era of ED boarding and bed shortages. Give a long-acting insulin dose every 24 hours (or restart the patient’s home long-acting regimen) and short-acting insulin every 2 to 4 hours. Aggressive IV fluid resuscitation, electrolyte repletion, and treatment of underlying precipitating cause remain additional cornerstones of DKA management.
