Category: Trauma
Keywords: Head injury, BIG, pediatric (PubMed Search)
Posted: 6/23/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Brain injury guidelines were designed to decrease transfers and neurosurgical consults for adults with head injuries.
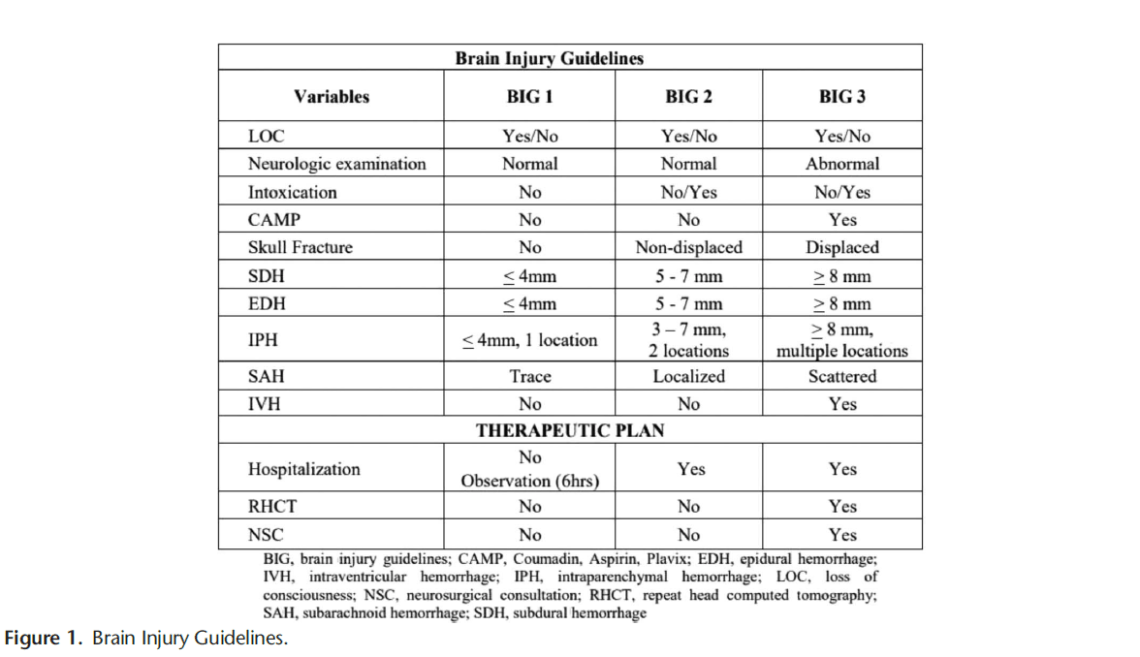
A new retrospective study suggests that modified guidelines may be feasible in the pediatric population as well. More data is needed but this is an important step in assuring safe resource utilization in pediatric head injury patients.
1. https://first10em.com/the-brain-injury-guidelines-can-we-avoid-talking-to-neurosurgeons/
2. Kay AB, Glasgow SL, Kahan AM, Swendiman RA, Kastenberg ZJ, Roach CM, Wan HY, Bollo RJ, Iyer RR, Ravindra VM, Morris DS, Yorkgitis BK, Joseph B, Russell KW. Small Change, BIG Impact: Proposal of the Brain Injury Guidelines for kids (kBIG). J Pediatr Surg. 2025 May 17;60(8):162372.
Category: Infectious Disease
Keywords: Abscess, brain, drainage, neurosurgery (PubMed Search)
Posted: 6/22/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In a Danish study of 558 patients with a brain abscess, those that had early surgical drainage did better than those treated conservatively with antibiotics only. Prompt neurosurgical consultation is warranted for these patients.
Category: Trauma
Keywords: Intubation, trauma, mortality, operating room, Ed (PubMed Search)
Posted: 6/15/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In this Israeli study comparing mortality for trauma patients intubated in the emergency department vs the operating room, in hospital mortality was higher for the ED group before controlling for injury severity score and shock. After controlling for injury severity and shock, there was no difference in In hospital mortality. Coupled with previous research, if intubation can wait until after resuscitation and in the OR, that is ideal. And sometimes it just has to happen in the ED and we should be prepared for rapid resuscitation.
Talmy T, Radomislensky I, Brzezinski Sinai I, Shaylor R, Katorza E, Gendler S; Israel Trauma Group Collaborators. Intubation Setting and Mortality in Trauma Patients Undergoing Hemorrhage Control Surgery: A Propensity Score-Matched Analysis. Anesth Analg. 2025 May 16. doi: 10.1213/ANE.0000000000007542. Epub ahead of print. PMID: 40378073.
Category: Trauma
Keywords: Hysterotomy (PubMed Search)
Posted: 6/8/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Another case series of 3 resuscitative hysterotomies, all performed by obstetricians, reported 33% maternal and 67% neonate survival.(1).
The mechanics of the procedure are:
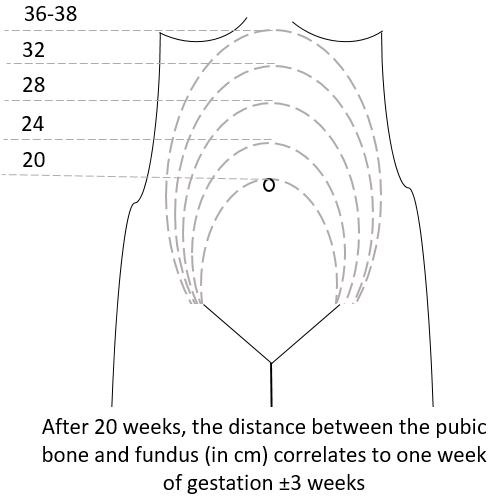
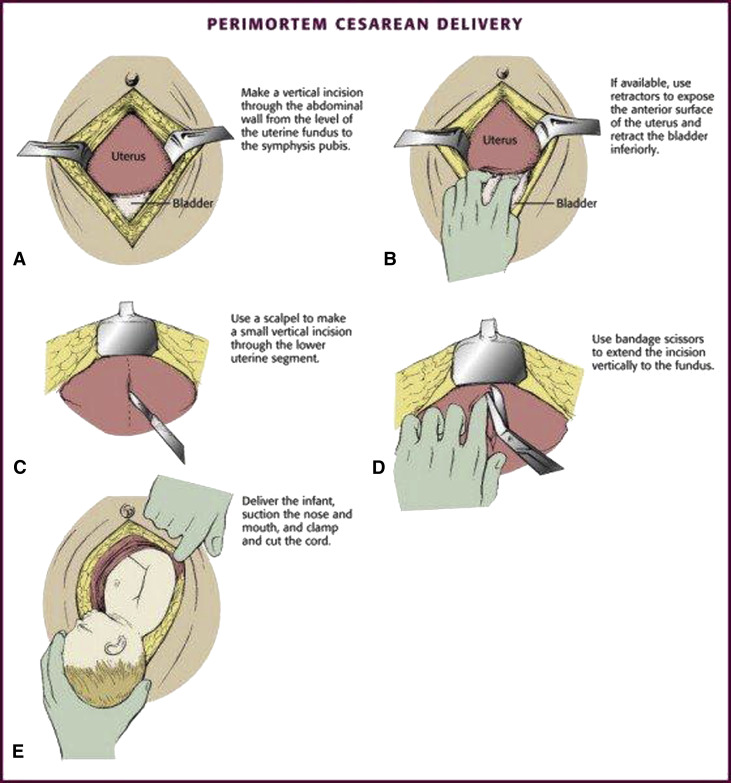
(3)
Category: Trauma
Posted: 6/7/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
A literature search revealed very little evidence, however in 66 women and 68 neonates who underwent resuscitative hysterotomy for out of hospital cardiac arrest 4.5% of women and 45% of neonates survived to discharge. The longest down time was 29 minutes and 47 minutes for women and neonates respectively. While more evidence is needed, it appears this procedure should be performed as early as possible and may lead to some survival benefit.
Leech C, Nutbeam T, Chu J, Knight M, Hinshaw K, Appleyard TL, Cowan S, Couper K, Yeung J. Maternal and neonatal outcomes following resuscitative hysterotomy for out of hospital cardiac arrest: A systematic review. Resuscitation. 2025 Feb;207:110479. doi: 10.1016/j.resuscitation.2024.110479. Epub 2024 Dec 29. PMID: 39736393.
Category: Trauma
Keywords: Femur fracture, splint (PubMed Search)
Posted: 6/6/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
The National Association of Emergency Medical Service Physicians reminds us that femur fractures rarely cause enough blood loss to cause hemodynamic instability (look for other sources), often have concomitant injuries in the pelvis or distal extremity, and can be effectively splinted either static or with traction (which has contraindications, complications, and technical hurdles).
John W. Lyng, Joshua G. Corsa, Philip S. Nawrocki, Brad D. Raetzke, Josh
Nackenson & Nichole Bosson (07 May 2025): Prehospital Trauma Compendium: Management
of Suspected Femoral Shaft Fractures – A position statement and resource document of
NAEMSP, Prehospital Emergency Care, DOI: 10.1080/10903127.2025.2493846
To link to this article: https://doi.org/10.1080/10903127.2025.2493846
Category: Trauma
Keywords: Nail gun injury, surgery, antibiotics (PubMed Search)
Posted: 5/31/2025 by Robert Flint, MD
(Updated: 6/1/2025)
Click here to contact Robert Flint, MD
An Australian retrospective study of 158 patients treated for nail gun injuries found those treated with operative debridement or with prophylactic antibiotics had no different 30 day infection rates compared to patients receiving no antibiotics.
Slater S, Vasudeva M, Mitra B, Sreedharan S. Penetrating nail gun injuries: Role of antibiotics and surgical management. Trauma. 2025;0(0). doi:10.1177/14604086251320524
Category: Trauma
Keywords: geriatric, trauma, CT scan (PubMed Search)
Posted: 5/29/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This literature search from 1946-2023 looking at comparing selective use of CT scans vs whole body scans in geriatric trauma found no benefit of whole body CT in mortality, hospital length of stay or ED discharge. This study only included 15,000 pts over that very long time line. More robust, current work needs to be done on this important topic.
Tang P, Elkington O, Stevens S. Whole body CT-scan vs. selective CT-scan in geriatric trauma: Systematic review and meta-analysis. Trauma. 2025;0(0). doi:10.1177/14604086241304629
Category: Infectious Disease
Keywords: Coccidioidomycosis, climate change (PubMed Search)
Posted: 5/26/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Typically Coccidioidomycosis is seen in the Southwestern US. The authors of this study, using climate modeling predict endemic areas will spread across the US to include Idaho, the Dakotas, Nebraska and Wyoming.
Clinically, “Patients with pulmonary Coccidioides infection frequently experience fever, cough, and shortness of breath. Chest radiographic imaging may demonstrate lobar, segmental, or multifocal consolidations; cavitary lesions; and lung nodules. Given these nonspecific findings, patients with coccidioidomycosis are often treated for community-acquired pneumonia. Coccidioidomycosis should be considered in patients not improving with antibiotic treatment or in those who have exposure to or reside in endemic areas. Up to 50% of patients with pulmonary coccidioidomycosis have erythema nodosum, approximately 25% to 30% have peripheral eosinophilia, and approximately 25% have arthralgias (particularly symmetric knee and ankle arthralgia). Up to 10% of patients diagnosed with coccidioidomycosis develop disseminated disease, including skin, central nervous system, and bone and joint infection.”
Lee PS, Swain DL, Johnson R. Climate Change and Coccidioidomycosis. JAMA. 2025;333(11):997–998. doi:10.1001/jama.2024.27274
Category: Neurology
Keywords: CVA, TIA, prediction, one year (PubMed Search)
Posted: 5/21/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
How likely is your TIA pt to go on to have a stroke? This study in JAMA gives us some answers. While EM providers aren’t as interested in 5 and 10 year prediction, it provides more evidence TIAs need to be evaluated and are risk factors for future events.
“In this systematic review and meta-analysis of 171?068 patients with TIA or minor stroke from 38 studies, the risk of subsequent stroke was 5.9% within 1 year, 12.8% within 5 years, and 19.8% within 10 years.”
Category: ENT
Keywords: Epistaxis prophylaxis (PubMed Search)
Posted: 5/18/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This large retrospective database study compared those receiving antibiotics after anterior nasal packing to those that did not. There was no difference in clinically significant infection between the groups leading the authors to conclude prophylactic antibiotics after anterior nasal packing is not required.
Tran QK, Vashee I, Vanga R, Camp S, Rallo MK, Najafali D, Bontempo LJ, Pourmand A. Is antibiotic prophylaxis necessary for anterior epistaxis with packing? Insights from a large database. Am J Emerg Med. 2025 Mar 19;93:64-72. doi: 10.1016/j.ajem.2025.03.040. Epub ahead of print. PMID: 40147155.
Category: Trauma
Keywords: Incarcerated, trauma, mortality, disparity (PubMed Search)
Posted: 5/11/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Looking at a year’s worth of data from the National Trauma Databank, the authors found incarcerated trauma patients were more likely to be stabbed, male, persons of color and have a higher adjusted mortality rate.
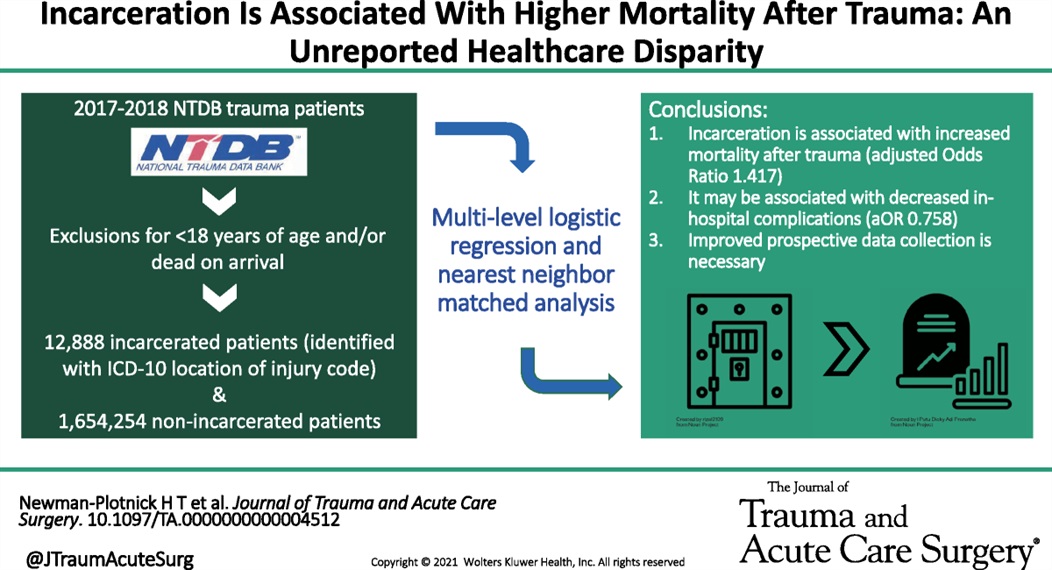
Newman-Plotnick, Harry MD, MPH; Byrne, James P. MD, PhD; Haut, Elliott Richard MD, PhD, FACS; Hultman, Charles Scott MD, MBA, FACS
Journal of Trauma and Acute Care Surgery 98(5):p 785-793, May 2025. | DOI: 10.1097/TA.0000000000004512
Category: Orthopedics
Keywords: Hip fractures, geriatrics, complications (PubMed Search)
Posted: 5/7/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This article reminds us that hip fractures have a one year mortality rate of 12-25% and 50% of hip fracture patients develop complications while in the hospital. “Almost half of individuals hospitalized with hip fractures experience complications, such as delirium, pneumonia, acute kidney injury, urinary tract infection, and deep vein thrombosis”
Because of these complications, multidisciplinary teams should be caring for these patients and great care should be exercised when evaluating these patients.
JAMA Insights
March 24, 2025
Yiju Teresa Liu, MD1,2; Eva Tovar Hirashima, MD, MPH3; Kabir Yadav, MDCM, MS, MSHS1,4
JAMA. Published online March 24, 2025. doi:10.1001/jama.2025.0999
Category: Cardiology
Keywords: aorta, dissection (PubMed Search)
Posted: 5/3/2025 by Robert Flint, MD
(Updated: 5/4/2025)
Click here to contact Robert Flint, MD
Aortic dissection remains a difficult diagnosis to make. This article is a nice review. The pathology behind this involves an intimal flap in the aortic wall. Death occurs due to aortic rupture or obstruction of branching artery.
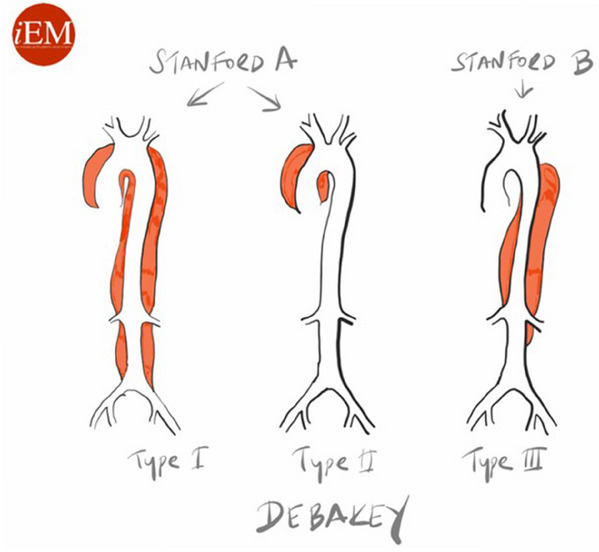
Risk factors: male 2:1 female, Marfan Syndrome, HTN, aortic aneurysm, cocaine and methamphetamine use, pregnancy
Pain is variable however tearing, ripping migrating, maximum at onset, and sharp are all associated with Aortic Dissection. Think about Dissection with atypical CP with ECG changes as well as in stroke like presentations along with chest pain.
Gold standard for diagnosis is CT angiogram. Decision rules with the use of D-Dimer have been proposed however there is still not sufficient evidence to use these. ACEP guidelines currently give use of decision rules a long with DDImer a level C recommendation.
Briggs, Blake et al.
JACEP Open, Volume 5, Issue 4, e13225
Category: Trauma
Keywords: Gun violence, mental health, suicide (PubMed Search)
Posted: 4/28/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This study looked at exposure to gun violence and found increased use of mental health resources, depression and suicide risk even with a single exposure. Repetitive exposure increased suicide risk as well as mental health service utilization, depression and overall health service utilization. While further work is needed, screening our patients for gun violence exposure could undercover mental health needs.
Daniel C. Semenza, Allison E. Bond, Devon Ziminski, Michael D. Anestis,
Frequency, recency, and variety of gun violence exposure: Implications for mental health and suicide among US adults,
Social Science & Medicine,
Volume 366,
2025,
117672,
ISSN 0277-9536,
https://doi.org/10.1016/j.socscimed.2025.117672.
(https://www.sciencedirect.com/science/article/pii/S0277953625000012
Category: Infectious Disease
Keywords: Necrotizing infection, antibiotic selection (PubMed Search)
Posted: 4/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
In the April edition of Annals of EM, there are opposing view points on the optimal antibiotic regiment for necrotizing soft tissue infection. One group proposes linezolid alone will cover all the worrisome pathogens namely group A Strep and Staph. There are less side effects including C. Diff infection with this medication. Another group suggests sticking to vancomycin plus/minus BLactam along with clindamycin. Their arguement centers around clindamycin is useful as an antitoxin more so than its antibacterial property.
Both offer reasonable evidence and neither is compelling enough to say one is superior to the other.
Optimal antibiotic Selevtion for Necrotizing soft tissue infections. Annals of Emergency Medicine. April 2025. Vol 8, No. 4 358-360
Category: Trauma
Keywords: Rural trauma care (PubMed Search)
Posted: 4/19/2025 by Robert Flint, MD
(Updated: 4/20/2025)
Click here to contact Robert Flint, MD
This study looking at the type of facility that cared for rural injured patients reminds us that the majority of trauma care for rural patients occurs in non-trauma centers. This included some of the most severely injured and for many definitive care was received at these centers.
This may lead to lack of inclusion in trauma registries and under valuing the care being delivered by non-trauma centers. Protocols to facilitate transfers, air medical protocols and availability along with tele-health all are important in rural trauma care. Non-trauma designated centers are a critical part of the trauma network for rural residents and their value can not be ignored.
Kaufman, Elinore J. MD, MSHP*; Prentice, Carter MD†; Williams, Devin BA‡; Song, Jamie MPH§; Haddad, Diane N. MD, MPH§; Brown, Joshua B. MD, MSc?; Chen, Xinwei MS¶; Colling, Kristin MD#; Chatterjee, Paula MD, MPH¶
Annals of Surgery 281(4):p 533-539, April 2025. | DOI: 10.1097/SLA.0000000000006540
Category: Trauma
Keywords: Mental health, trauma, intervention, blunt injury (PubMed Search)
Posted: 4/13/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study looked at pre-trauma mental health diagnosis (from medical records) and post-trauma mental health symptoms as assessed by survey. The majority of patients suffered blunt trauma and mean age was 67. Having pre/traumatic mental health diagnosis and particularly post-traumatic symptoms lead to worse health outcomes and financial conditions. Further work needs to be done to assess how to improve mental health symptoms post-traumatic injury.
Johnson, Patrick L. MD, MPH; Hemmila, Mark R. MD; Mullens, Cody L. MD, MPH; Oliphant, Bryant W. MD, MBA, MSc; Monahan, Janessa R. MS; Kelm, Julia D. BS; Jakubus, Jill L. PA-C, MHSA, MS; Curtiss, William J. MD; Mosher, Benjamin D. MD; Kieninger, Alicia N. MD; Scott, John W. MD, MPH
Journal of Trauma and Acute Care Surgery 98(3):p 425-434, March 2025. | DOI: 10.1097/TA.0000000000004521
Category: Gastrointestional
Keywords: Appendicitis, scoring, prediction, Alvarado Score (PubMed Search)
Posted: 4/6/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Missed appendicitis leading to rupture and peritonitis leads to morbidity, mortality, and malpractice claims. Part of a longer article looking at evaluation and management of appendicitis, these authors provide three scoring systems that can be used to identify appendicitis. Use of these scores can guide imaging and surgical consultation.
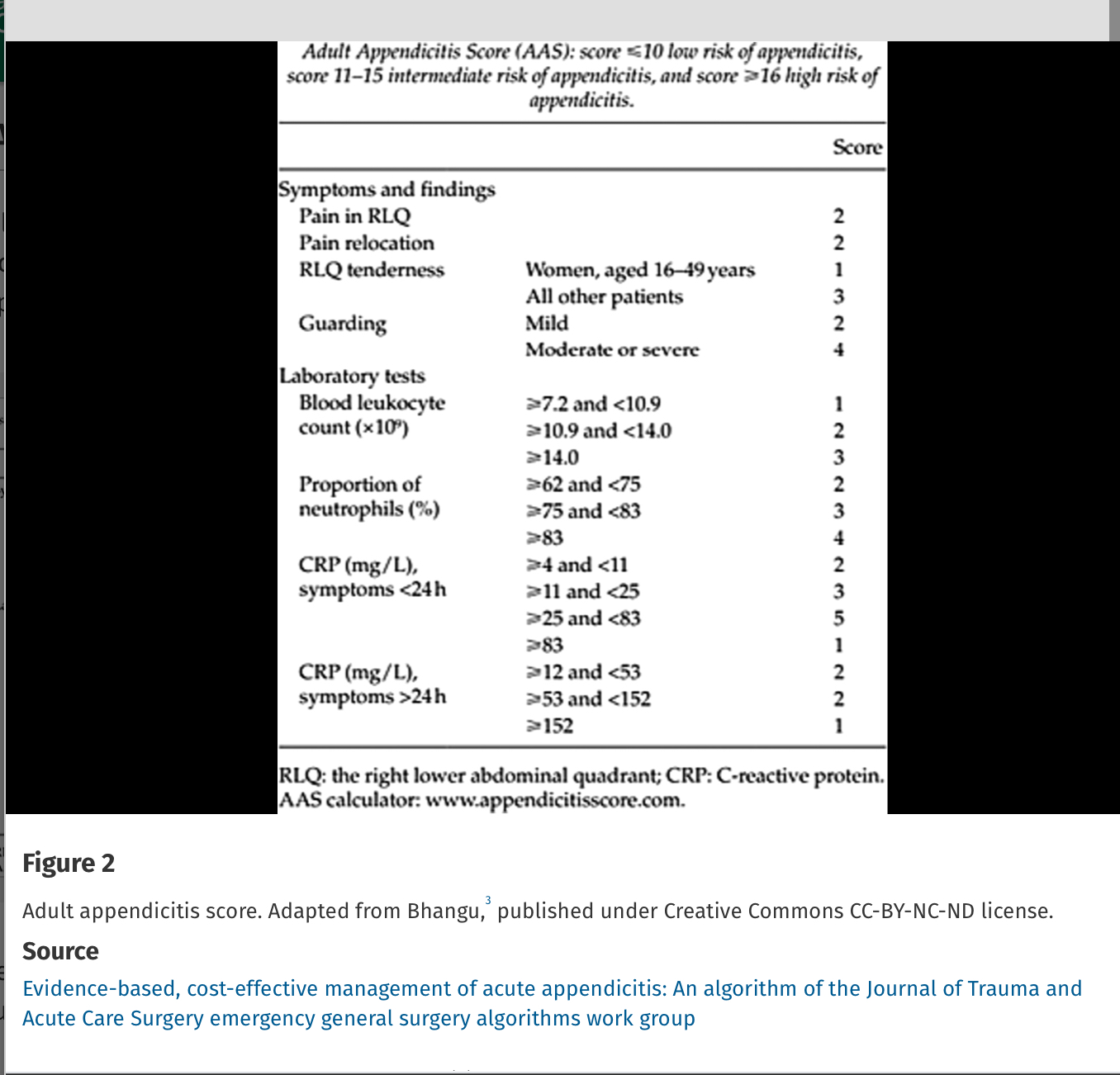
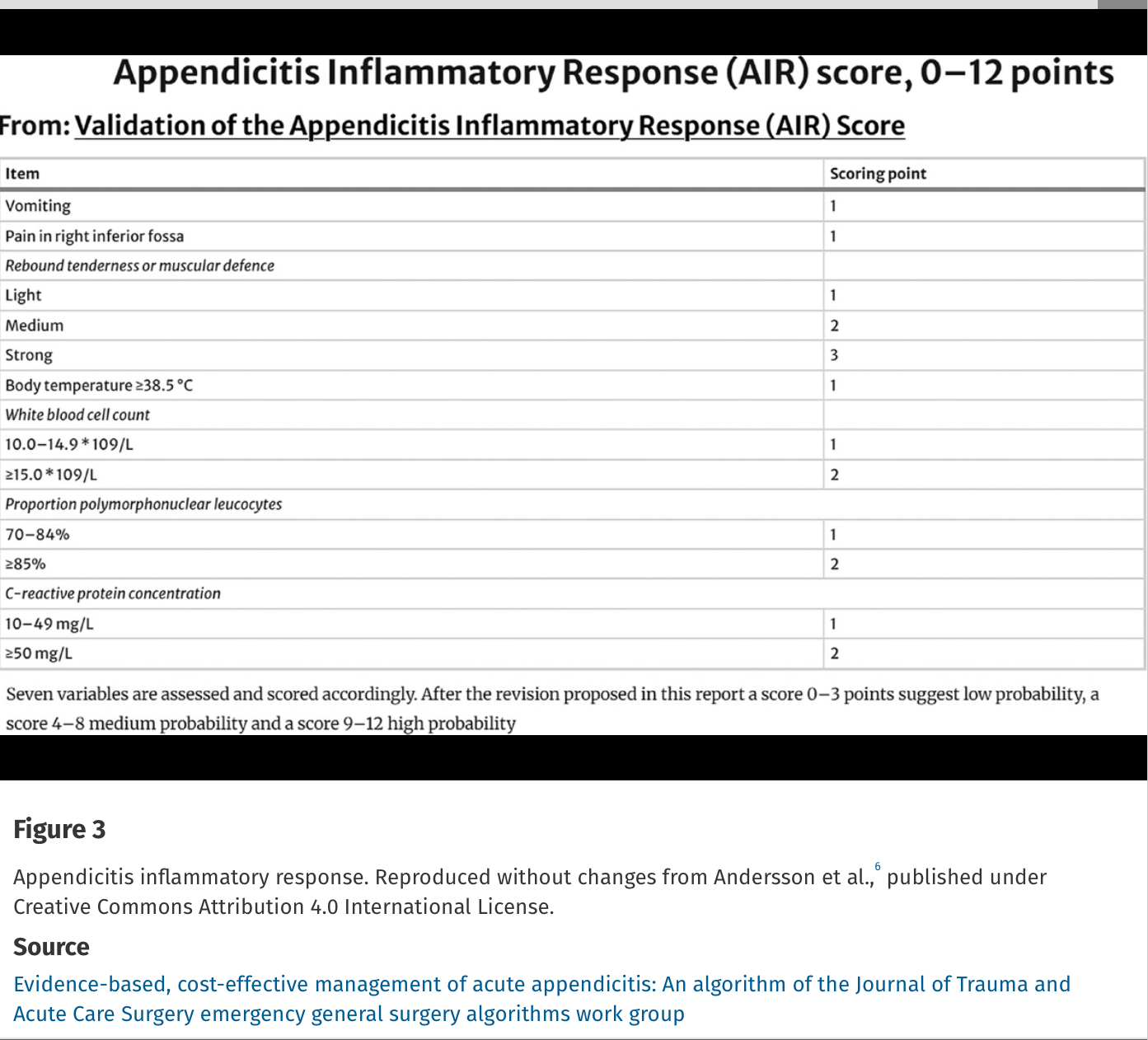
Alvarado Score: If a patient scores 1 to 4, the risk of appendicitis drops to 33%. If a patient scores >5, the risk of acute appendicitis is 66% or greater.
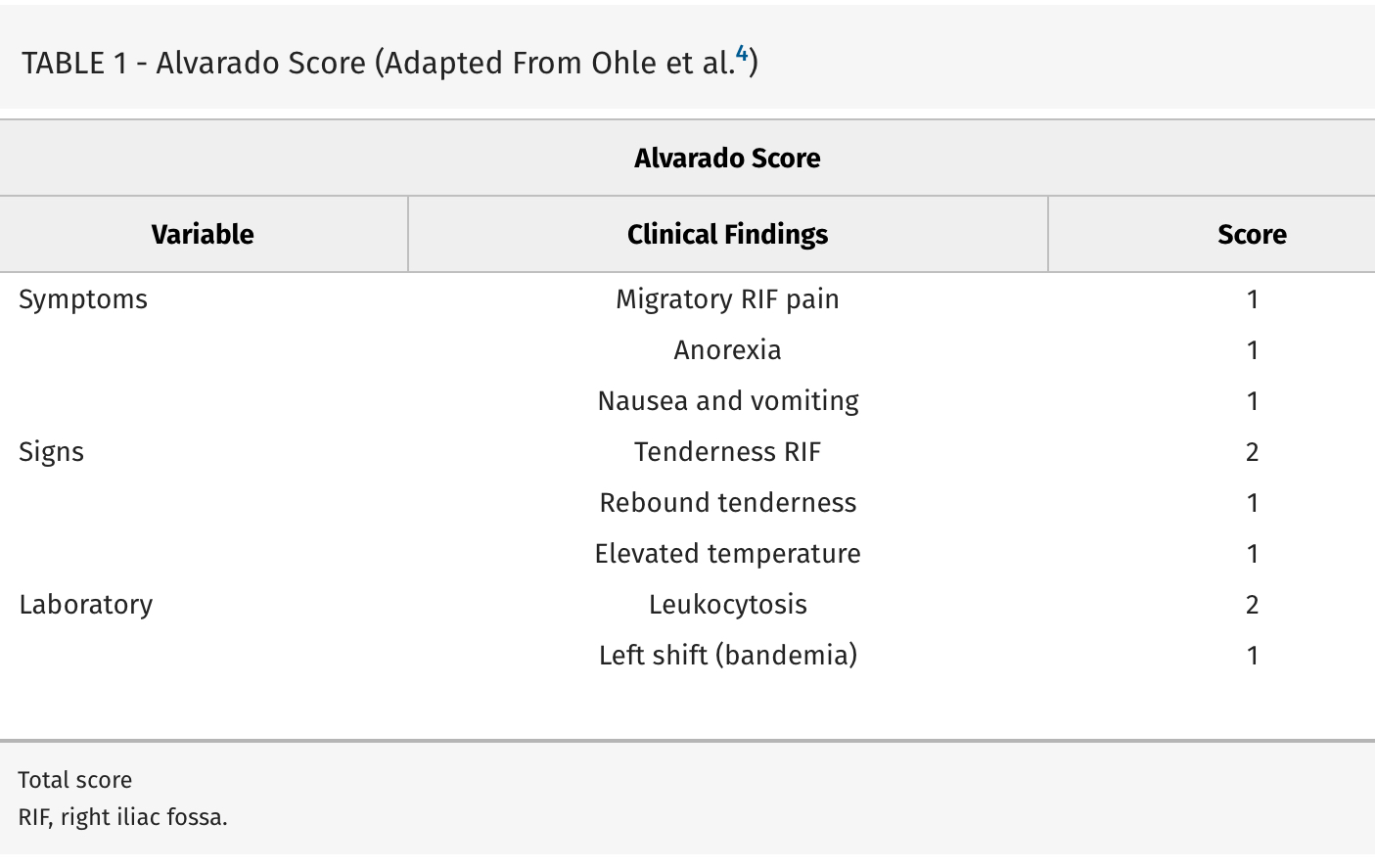
Evidence-based, cost-effective management of acute appendicitis: An algorithm of the Journal of Trauma and Acute Care Surgery emergency general surgery algorithms work group
Diaz, Jose J. MD, CPE, CNS, FACS, FCCM; Napolitano, Lena MD; Livingston, David H. MD; Costantini, Todd MD; Inaba, Kenji MD; Biffl, Walter L. MD; Winchell, Robert MD; Salim, Ali MD; Coimbra, Raul MD, PhD
Journal of Trauma and Acute Care Surgery 98(3):p 368-373, March 2025. | DOI: 10.1097/TA.0000000000004569
Category: Toxicology
Keywords: Toxicology, contaminate, opiate, stimulant (PubMed Search)
Posted: 4/5/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This study from Australia reminds us that what patients think they ingested isn’t always what they did ingest. A high percentage of “cocaine” and other stimulants was actually fentanyl or other opiates. The authors do a nice job referencing similar studies in the United States. Any overdose could be a mixed picture due to impure street drugs.
Emergency Medicine AustralasiaVolume 37, Issue 2 e70038
Original Research
Open Access
Peter Chisholm MBBS, B Med Sc, MPH, Jared Brown BPharm, MPH, Thanjira Jiranantakan MD, MPH, FAFPHM, FACOEM, Mary Ellen Harrod PhD, Catherine McDonald BSc, Una Cullinan BSc, Darren M Roberts MBBS, PhD, FRACP, FAChAM
First published: 03 April 2025
