Category: Cardiology
Posted: 2/16/2014 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Early Atherosclerosis Detection
50 middle-aged asymptomatic subjects free of vascular disease underwent carotid ultrasound (CUS) for risk stratification were also invited to undergo coronary computed tomography angiography (CCTA) or coronary artery calcium score (CAC) to identify which of the 3 imaging modalities was best at identification of early atherosclerosis
Atherosclerosis was observed in 28%, 78%, and 90% of subjects using CAC, CCTA, and CUS, respectively
36 patients with a CAC score = 0, 69% and 86% had atherosclerosis on CCTA and CUS, respectively
Concordance between modalities was highly variable
CUS and CCTA detection of plaque were significantly more sensitive than CAC
Considering the prevalence of subclinical disease on CUS and CCTA, the threshold at which to treat warrants further research
Schroeder B, Francis G, et al. Early Atherosclerosis Detection in Asymptomatic Patients: A Comparison of Carotid Ultrasound, Coronary Artery Calcium Score, and Coronary Computed Tomography Angiography. Canadian Journal of Cardiology, 2013-12-01, Volume 29, Issue 12, Pages 1687-1694
Category: Cardiology
Keywords: ECG, STEMI, aVL (PubMed Search)
Posted: 2/9/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
The importance of new ST-segment depressions (STD) and/or T wave inversions (TWI) in lead aVL have not been emphasized or well recognized across specialties. Computer-assisted ECG readings typically report these findings as normal or nonspecific.
There is growing evidence that changes in lead aVL are abnormal, and that paying attention to that lead can be clinically useful. Reciprocal changes presenting as STD or TWI in lead aVL may be indicative of a significant coronary artery lesion and can sometimes be the only ECG manifestation of acute MI.
STD in lead aVL is considered a sensitive marker for early inferior STEMI, and has been shown to help differentiate STEMI from pericarditis. Another recent retrospective study suggests that TWI in aVL might be associated with significant LAD lesions.
Bottom Line: Paying close attention to subtle changes and abnormalities in lead aVL may help in early identification and initiation of therapy for patients who are having an acute MI.
Hassen GW, Costea A, Smith T, et al. The Neglected Lead on Electrocardiogram: T Wave Inversion in Lead aVL, Nonspecific Finding or a Sign for Left Anterior Descending Artery Lesion?. Journal of Emergency Medicine. 2014;46(2):165–170.
Category: Cardiology
Posted: 2/2/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Myocardial Infarction in Women After Childbirth
World Health Organization reports that obesity is the 5th leading cause of global death with the highest impact on women <65 years of age
The association of obesity and cardiovascular risk in young women is currently being researched
A recent nationwide cohort looking at obesity and future cardiovascular risk looked at Danish women giving birth (2004-2009) and followed them a median time of 4.5 years
This study grouped women via pre-pregnancy body mass index (BMI)
1. Underweight (BMI <18.5)
2. Normal weight (BMI <25)
3. Overweight (BMI <30)
4. Obese (BMI >30)
Data revealed that healthy women of fertile age, pre-pregnancy obesity alone was associated with increased risk of myocardial infarction in the years after childbirth
Schmiegelow M, Andersson C, Kober L, et al. Prepregnancy Obesity and Associations With Stroke and Myocardial Infarction in Women in the Years After Childbirth. Circulation 2014;129:330-337.
Category: Cardiology
Keywords: Wide complex tachycardia, ventricular tachycardia (PubMed Search)
Posted: 1/26/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
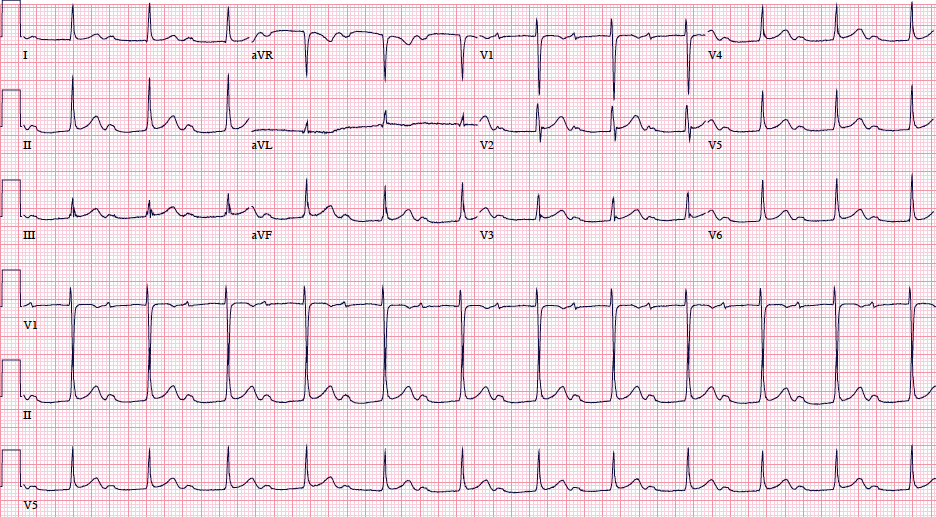
A 48 year old woman has acute chest pain and palpitations over the past several hours. She has felt similar palpitations in the past but never sought medical attention. She arrives to your ED alert and anxious. HR = 270, BP=130/100. ECG is below. What’s the diagnosis and treatment?
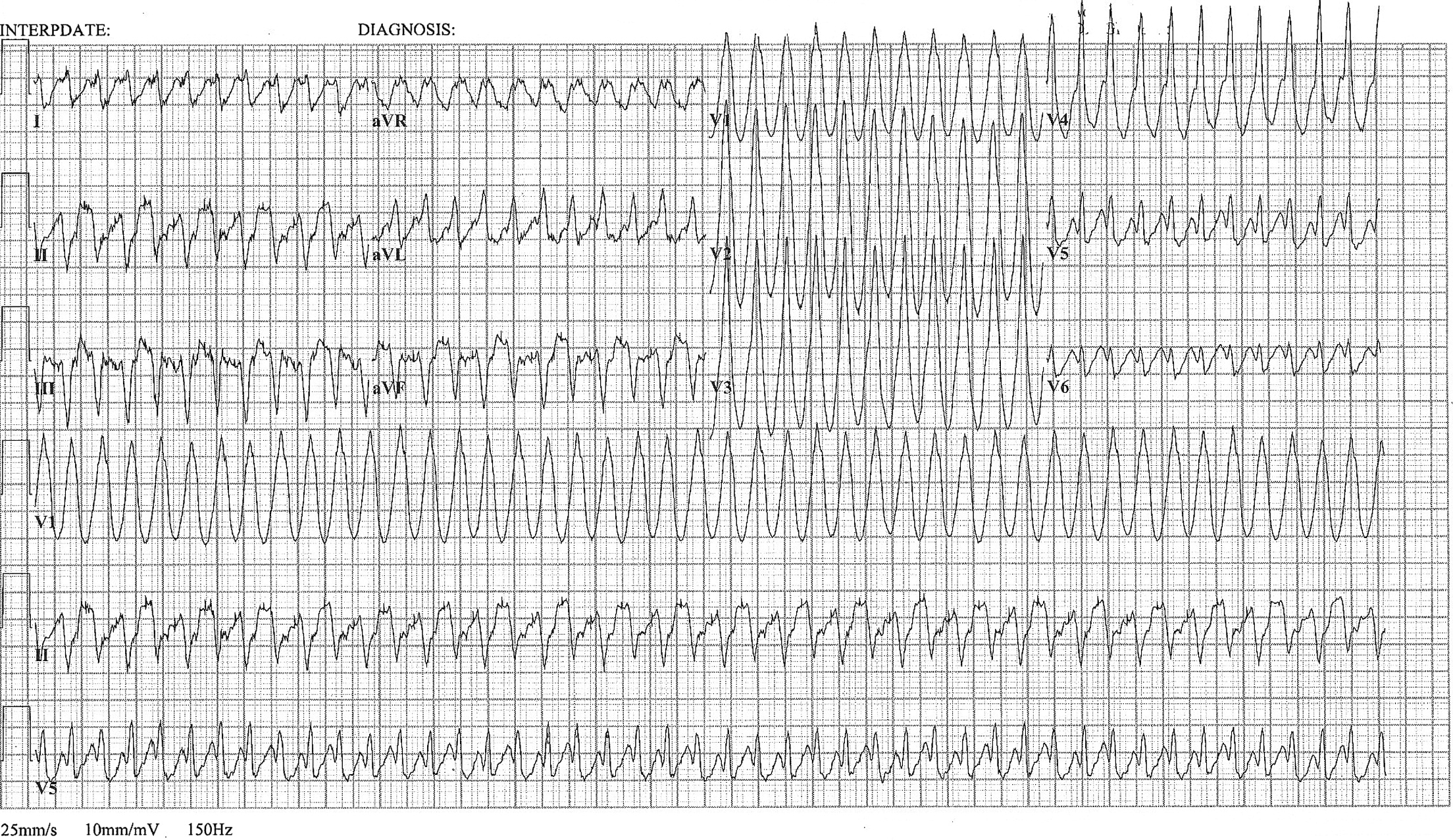
Most wide complex regular tachycardias are ventricular tachycardia (VT). However, supraventricular tachycardias can also cause wide complexes through aberrant conduction and accessory pathways.
Nelson JG, Zhu DW. Atrial Flutter with 1:1 Conduction in Undiagnosed Wolff-Parkinson-White Syndrome. The Journal of Emergency Medicine. January 2014. Pubmed Link
Category: Cardiology
Posted: 1/19/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Pacing Atrioventricular Block
- Atrioventricular (AV) block is classically treated with restoration of heart rate via right ventricular pacing, however high rates of right ventricular pacing is associated w/ left ventricular systolic dysfunction
- A recent multi-center randomized control trial (RCT) assessed the efficacy of right vs biventricular pacing in heart failure w/ AV block [BLOCK HF Trial]
- Primary outcomes of: morbidity, mortality, and adverse left ventricular remodeling were shown to be significantly lower in biventricular vs right ventricular pacing
- In patients with a high rate of pacing and/or an abnormally low left ventricular ejection fraction biventricular pacing may be more advantageous than conventional right ventricular pacing
Curtis A.B., Worley S.J., Adamson P.B.,et al: Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med 2013; 368: 1585-1593
Category: Cardiology
Keywords: PVC, Premature ventricular beats, Premature ventricular complexes (PubMed Search)
Posted: 1/12/2014 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Differentiation between right and left ventricular origin of premature beats can be useful clinically.
PVCs arising from the right ventricle have a left bundle branch block morphology (dominant S wave in V1)
PVCs arising from the left ventricle have a right bundle branch block morphology (dominant R wave in V1)
Left Ventricular premature beats are more often associated with heart disease and may precipitate ventricular fibrillation, whereas right ventricular premature beats are commonly seen in individuals with normal hearts.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Wagner, Galen. Chapter 15 - Premature Beats. Marriott's Practical Electrocardiography, 12th Edition. 2013
Category: Cardiology
Posted: 1/5/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Assessment of Intermediate Coronary Lesions
- Coronary angiography alone to assess CAD is fraught with subjectivity
- Fractional flow reserve (FFR) has become the standard to assess/quantify obstructive CAD; it determines the myocardial flow in the presence of stenosis identifying the lesion responsible for ischemia
- FFR assesses focal stenosis, but does not consider diffuse atherosclerotic narrowing or microcirculatory dysfunction as contributors of ischemic heart disease
- An index of microcirculatory resistance (IMR) can be concomitantly measured with FFR during cardiac catheterization to specifically evaluate the microvasculature
- Coronary flow reserve (CFR) was the 1st proposed method for assessment of intermediate coronary lesion, but proved suboptimal because of its variability especially in patients with microvascular dysfunction (diabetes, prior MI, etc.)
- Utilization of FFR, IMR, and CFR together support the existence of differentiated patterns of ischemic heart disease & may help to determine future ischemic events
Echavarria-Pinto M, Escaned J, Macias E, et al. Disturbed Coronary Hemodynamics in Vessels With Intermediate Stenosis Evaluated With Fractional Flow Reserve: A Combined Analysis of Epicardial and Microcirculatory Involvement in Ischemic Heart Disease. Circulation Volume 128(24), 17 December 2013, p 2557–2566
Category: Cardiology
Keywords: ST-elevation, Cardiology, MI (PubMed Search)
Posted: 12/29/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
There is debate and confusion regarding where and how to measure ST elevation (STE). Do you measure the STE at the J-point? Or at 40 msec after the J-point? And how much STE is considered significant? The current guidelines have clarified this issue.
- STE should be measured at the J-point.
- STEMI is defined by STE ≥ 1 mm in at least 2 contiguous leads, with the exception of leads V2-V3.
- STEMI is defined by STE ≥ 2 mm in leads V2-V3 in men.
- STEMI is defined by STE ≥ 1.5 mm in leads V2-V3 in women.
For more cardiology pearls from the 2013 literature , check out Amal Mattu's Articles You've Gotta Know!
Want more emergency cardiology pearls? Follow me @alifarzadmd
2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction
O'Gara PT, Kushner FG, Ascheim DD, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Circulation. 2013;127:e362-e425 Pubmed Link
Category: Cardiology
Posted: 12/22/2013 by Semhar Tewelde, MD
(Updated: 1/31/2026)
Click here to contact Semhar Tewelde, MD
Metoprolol Usage Cardioprotective
Ibanez B, Sanchez-Brunete V, Pizarro G, et al. Effect of early metoprolol on infarct size in ST-segment-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial. Circulation. 2013 Oct 1; 128(14):1495-503.
Category: Cardiology
Keywords: ACS, Chest Pain, HEART score (PubMed Search)
Posted: 12/8/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Bottom-line: The HEART score can help to objectively risk stratify ED patients with chest pain into low, intermediate, and high risk groups. Using the HEART score can also facilitate more efficient and effective communication with colleagues.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. International Journal of Cardiology. 2013;168(3):2153–2158.
Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191–196.
Category: Cardiology
Keywords: Cardiac Transplant (PubMed Search)
Posted: 12/1/2013 by Semhar Tewelde, MD
(Updated: 8/28/2014)
Click here to contact Semhar Tewelde, MD
ECG Following Cardiac Transplant
Chou's Electrocardiography in Clinical Practice: Adult and Pediatric 6th Edition
Category: Cardiology
Keywords: Therapeutic Hypothermia, ROSC, Cardiac Arrest, Resuscitation (PubMed Search)
Posted: 11/23/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Want more emergency cardiology pearls? Follow me @alifarzadmd
Category: Cardiology
Keywords: Intra-Aortic Balloon Pump, Cardiogenic Shock (PubMed Search)
Posted: 11/15/2013 by Semhar Tewelde, MD
(Updated: 11/17/2013)
Click here to contact Semhar Tewelde, MD
Utility of Intra-Aortic Balloon Pump (IABP)
Kettner J, Sramko M, Holek M, et al. Utility of Intra-Aortic Balloon Pump Support For Ventricular Septal Rupture and Acute Mitral Regurgitation Complicating Acute Myocardial Infarction. American Journal of Cardiology. 2013 Vol 112 Issue 11 Pages 1709-1713
Category: Cardiology
Keywords: AMI, LBBB, Sgarbossa criteria (PubMed Search)
Posted: 11/9/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Diagnosis of STEMI in patients with LBBB can be challenging. Guidelines that previously recommended emergent reperfusion for these patients have been reconsidered to avoid inappropriate cath lab activation and fibrinolytic therapy.
The 2013 ACC/AHA STEMI guidelines no longer consider new or presumably new LBBB a STEMI equivalent. This dramatic change may prevent inappropriate therapy for some, but fail to help identify patients with LBBB who are having STEMI's. Delayed reperfusion in this population could be fatal and is estimated to affect 5,000-10,000 patients per year in the US alone.
The Sgarbossa ECG criteria are the most validated tool to aid in the diagnosis of STEMI in the presence of LBBB. A Sgarbossa score of ≥ 3 has high specificity (>98%) and positive predictive value for acute MI and angiography-confirmed coronary occlusion. The following algorithm has been recently proposed to identify the high-risk population in which reperfusion therapy would be denied by the 2013 STEMI guidelines.
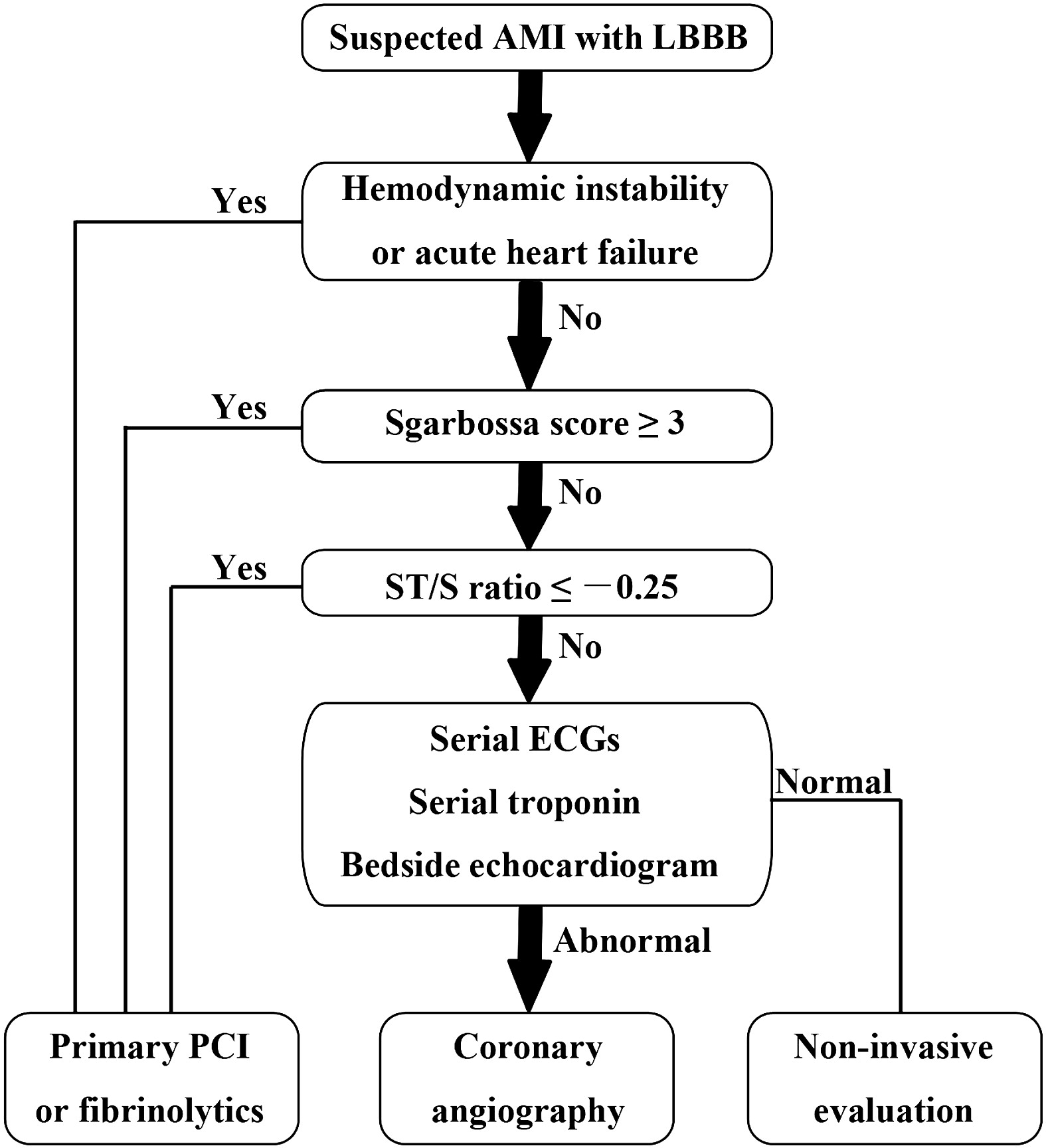
Watch this video to review Sgarbossa criteria and the modified Sgarbossa rule.
Want more emergency cardiology pearls? Follow me @alifarzadmd
The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? American Heart Journal. 2013;166(3):409–413.
Category: Cardiology
Posted: 11/3/2013 by Semhar Tewelde, MD
(Updated: 11/16/2013)
Click here to contact Semhar Tewelde, MD
Secondary Prevention in AMI
Just as aspirin is pivotal in the treatment of acute coronary syndrome, medications such as beta-blocker, statins, and angiotensin-converting enzyme inhibitors have been proven to be essential in secondary prevention of AMI.
Patients after AMI are typically discharged on appropriate secondary prevention medications; however the prescribed doses are often far below the proven efficacy based on clinical trials.
A review of 6,748 patients from 31 hospitals enrolled in 2 U.S. registries (2003 to 2008) illustrated that only 1 in 3 patients were prescribed these medications at goal doses.
Of patients not discharged on goal doses, up-titration during follow-up occurred infrequently ~25%.
Optimal medication dosing and appropriate titration is integral to prevention of further morbidity and mortality.
Arnold S, Spertus J, Masoudi F, et al. Beyond Medication Prescription as Performace Measure: Optimal Secondary Prevention Dosing After Acute Myocardial Infarction. JACC Nov 5, 2013 Vol 62:19;1791-1801
Category: Cardiology
Keywords: AV Block (PubMed Search)
Posted: 10/27/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
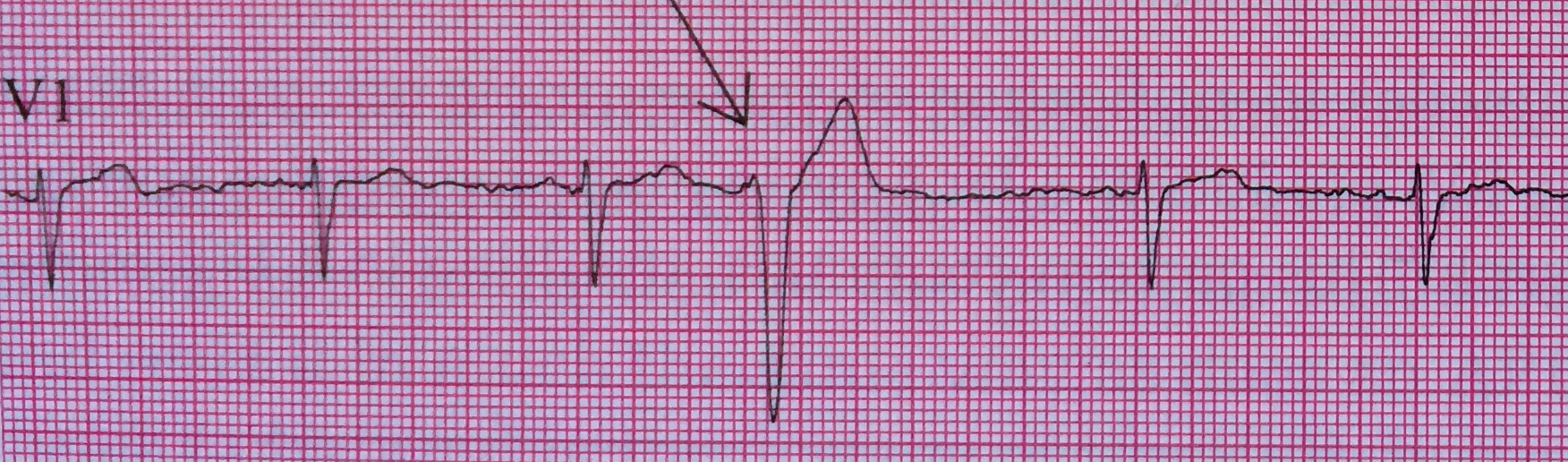
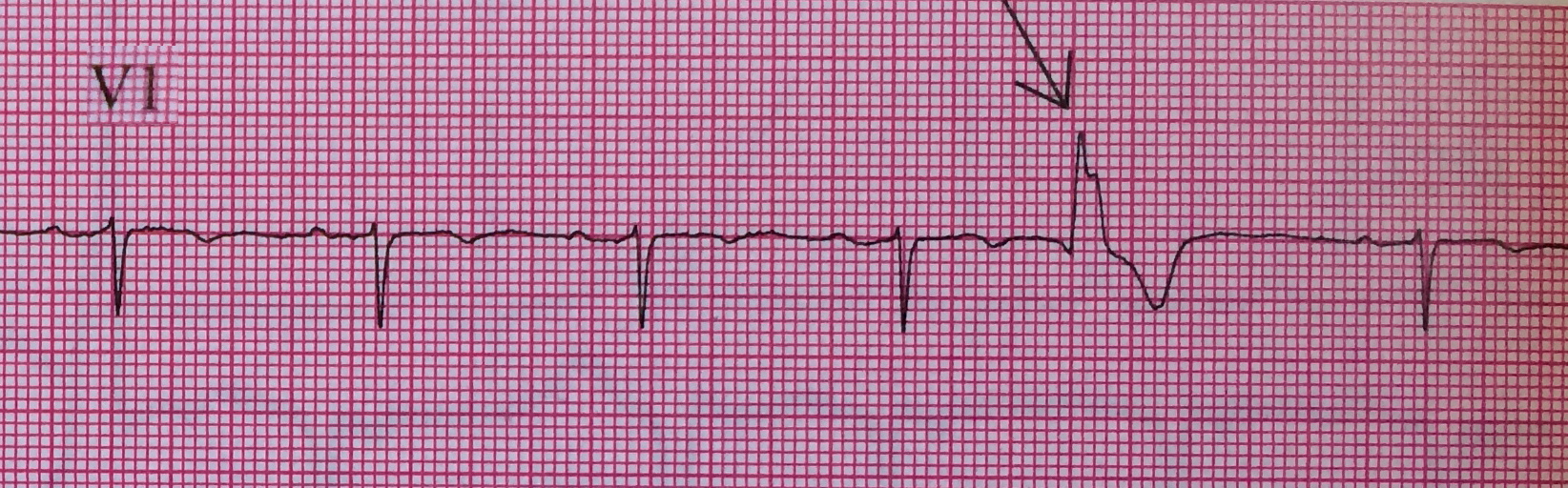
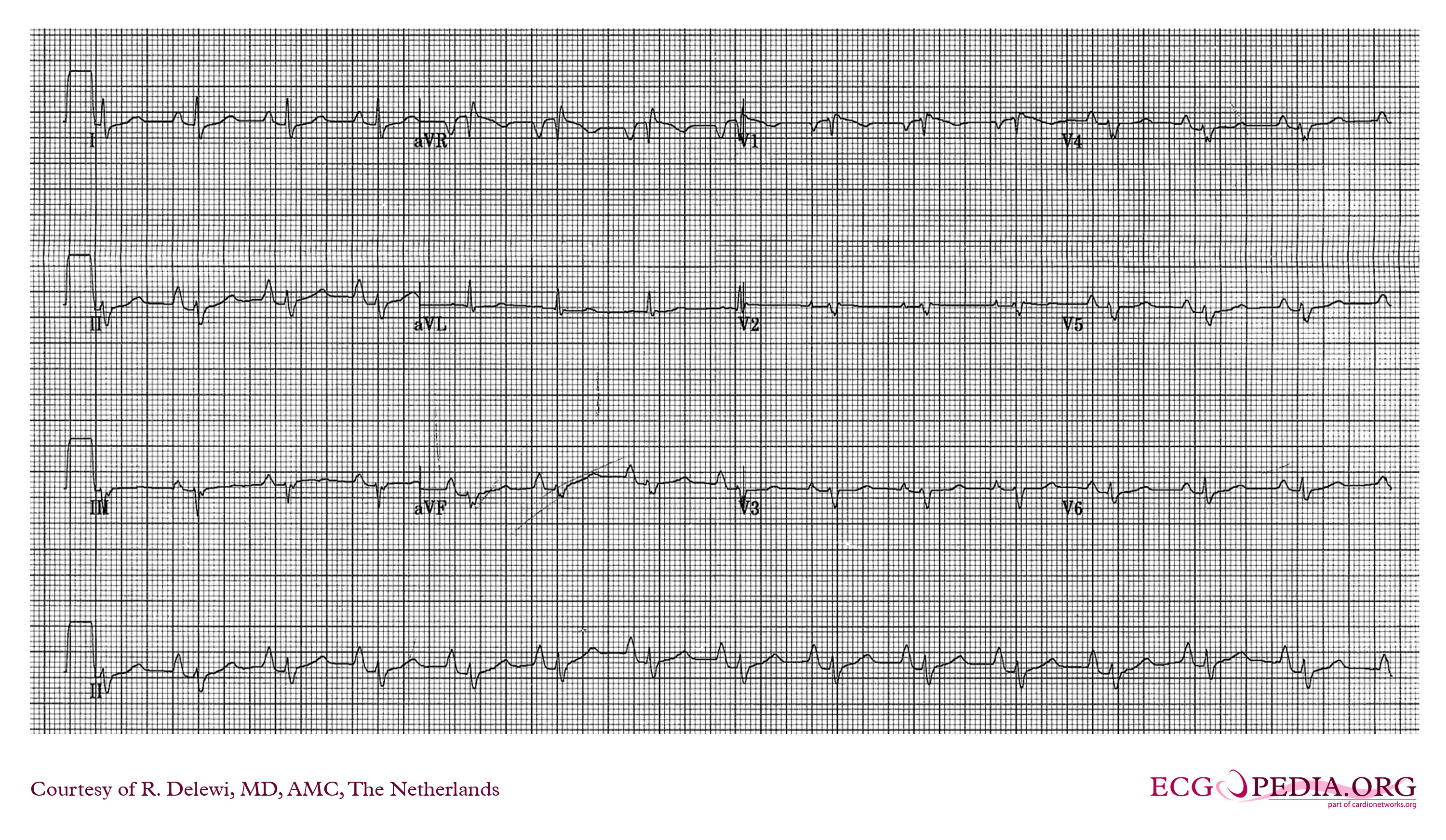
First-degree atrioventricular (AV) block is defined as an abnormally prolonged PR-interval >200ms. Although traditionally considered to be a benign clinical entity, not all first degree AV blocks are treated the same.
Markedly prolonged PR-intervals (PR >300ms) can cause symptoms and hemodynamic compromise due to inadequate timing of atrial and ventricular contractions. Consider the following ECG from a 32 YOF with intermittent episodes of syncope and dizziness…
There is marked first degree AV block (PR=434 ms). When the PR-interval gets too long, AV dyssynchrony compromises ventricular filling and decreases cardiac output, similar to the so-called pacemaker syndrome.
Current ACC/AHA guidelines state that permanent pacemaker implantation is reasonable for marked first degree AV block with hemodynamic compromise or symptoms similar to those of pacemaker syndrome. (Class IIa, Level of Evidence B). The guidelines caution that pacemakers are not indicated in asymptomatic patients with isolated first degree AV block.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Special thanks to Dr. Brandon Cole for submitting the ECG
References / Further Reading (Attached)
First-Degree AV Block-An Entirely Benign Finding or a Potentially Curable Cause of Cardiac Disease? Annals of Noninvasive Electrocardiology.2013;18(3):215–224. doi:10.1111/anec.12062.
ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008;117(21):e350–e408. doi:10.1161/CIRCUALTIONAHA.108.189742.
Category: Cardiology
Posted: 10/20/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Ebstein's Anomaly
Osiro S, Tiwari K, Mathenge N, et al. When Lithum Hurts: A Look at Ebstein Anomaly. Cardiology in Review. Oct 2013, Vol 21(5); pgs 257-263.
Category: Cardiology
Keywords: Dyspnea, Chest Pain (PubMed Search)
Posted: 10/13/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
A 48 year-old female presents to the ED with progressive dyspnea and chest discomfort over the past 3 months. HR = 105, BP = 100/60 mmHg, with mild JVD on exam. Her ECG is shown below. What ECG abnormalites are present? What does your differential diagnosis include? What is the best initial diagnostic test?
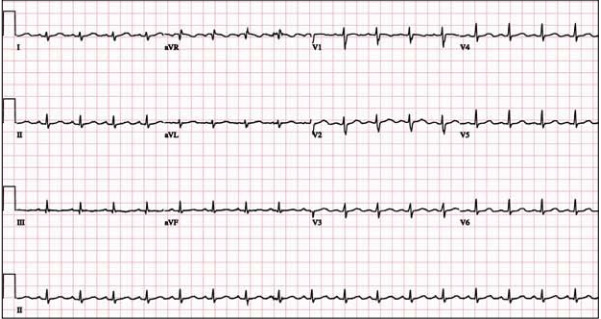
The ECG shows sinus tachycardia at rate of 107 with low QRS voltage diffusely. Echocardiogram revealed significant pericardial effusion with signs of impending tamponade. Emergent pericardiocentesis was performed and her symptoms improved.
Low QRS voltage (LQRSV)
LQRSV Differential
Want more emergency cardiology pearls? Follow me @alifarzadmd
Category: Cardiology
Keywords: Aortic Syndrome, Aortic Dissection, Intramural hematoma, Atheromatous ulcer (PubMed Search)
Posted: 10/6/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Acute Aortic Syndromes
Classically, aortic dissection is considered the primary culprit in patients with chest pain that radiates to the back (aortic pain) or chest pain combined with ischemia (cerebral, cardiac, peripheral), syncope, or cardiac arrest. However, it should not be your only concern: the rate of aortic rupture is much higher in penetrating atheromatous ulcer (42%) and intramural hematoma (35%) than in aortic dissection (types A 7.5% and type B 4.1%).
Chest pain with concomitant ischemic symptoms and acute decompensation should prompt consideration of several etiologies under the umbrella of aortic syndromes and not limited to dissection :
Sheikh A, Ali K, Mazhar S. Acute Aortic Syndrome. Circulation 2013;128:1122-1127
Coady MA, Rizzo JA, Elefteriades JA. Pathological Variants of thoracic aortic dissection. Penetrating atherosclerotic ulcers and intramural hematomas. Cardiol Clin. 1999;17:637-657
Category: Cardiology
Posted: 9/29/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
The primary goal in management of STEMI is rapid coronary revascularization. STEMI's are occasionally complicated by ventricular fibrillation (VF) arrest. High quality chest compressions and early defibrillation will improve survival. But what can be done in cases where conventional ACLS measures fail and patients have shock-refractory VF?
Some have suggested that emergent PCI with ongoing CPR en route may be beneficial. This option may be considered in close consultation with cardiology if the arrest is thought to be driven by ongoing ischemia and infarction. However, definitive data is lacking and this has only been described in a handful of case reports.
There may also be a role for venoarterial ECMO to aid in perfusion of vital organs and limit the risk of multisystem organ failure. The ECMO circuit can also help facilitate therapeutic hypothermia after the culprit vessel(s) is revascularized and rhythm is restored.
Chances for survival are highest in younger patients, those that do not have chronic illnesses, and those who received immediate CPR after arrest.
Summary:
Consider emergent consultation for salvage PCI and ECMO in select cases of shock-refractory ventricular fibrillation associated with STEMI
Want more emergency cardiology pearls? Follow me @alifarzadmd
A recently published case report (attached) presents a fascinating case where salvage PCI and ECMO were used for shock-refractory VF. The patient survives with good neurological outcome. It highlights the multidisciplinary cooperation and resources necessary to utilize these heroic practices.
Brown DFM, Jaffer FA, Baker JN, Gurol ME. Case records of the Massachusetts General Hospital. Case 28-2013. A 52-year-old man with cardiac arrest after an acute myocardial infarction. N Engl J Med. 2013;369(11):1047–1054. doi:10.1056/NEJMcpc1304164.
