Category: Critical Care
Posted: 2/19/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Managing Traumatic Hemorrhagic Shock
Bougle A, et al. Resuscitative strategies in traumatic hemorrhagic shock. Annals of Intensive Care 2013; 3.
Category: Critical Care
Posted: 2/12/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Propofol is generally a well-tolerated sedative / amnestic but occasionally it can lead to the propofol infusion syndrome (PRIS); a metabolic disorder causing end-organ dysfunction.
Suspect PRIS in patients with increasing lactate levels, worsening metabolic acidosis, worsening renal function, increased triglyceride levels, or creatinine kinase levels. End-organ effects include:
The true incidence of PRIS is unknown, however, certain risk factors have been identified:
Prevent PRIS by using adequate analgesia (with morphine or fentanyl) post-intubation, which may reduce the overall dosage of propofol ultimately reducing the risk.
If PRIS develops, stop propofol and provide supportive care; IV fluids, ensuring good urine output, adequate oxygenation, dialysis (if indicated), vasopressor and inotropic support.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 2/5/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Needle Decompression - Are we Teaching the Right Location?
Inaba K, et al. Optimal positioning for emergent needle thoracostomy: A cadaver-based study. J Trauma 2011; 71:1099-1103.
Inaba K, et al. Radiologic evaluation of alternative sites for needle decompression of tension pneumothorax. Arch Surg 2012; 147:813-8.
Martin M, et al. Does needle decompression provide adequate and effective decompression of tension pneumothorax? J Trauma 2012; 73:1412-1417.
Category: Critical Care
Posted: 1/29/2013 by Haney Mallemat, MD
(Updated: 1/30/2013)
Click here to contact Haney Mallemat, MD
The updated Surviving Sepsis Guidelines have been released (click here) and here are some recommendations as they pertain to hemodynamic management (grades of recommendations in parenthesis).
Fluid therapy
Vasopressors (targeting MAP of at least 65 mmHg)
Corticosteroids
Inotropic Therapy
Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock. Crit Care Med. 2013 Feb;41(2):580-637.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 1/22/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Postintubation Hypotension
Heffner AC, Swords D, Kline JA, et al. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care 2012; 27:417e9-417e13.
Heffner AC, Swords D, Nussbaum ML, et al. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care 2012; 27:587-593.
Category: Critical Care
Posted: 1/15/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intra-aortic balloon pumps (IABP) are devices that provide hemodynamic support during cardiogenic shock; the balloon inflates during diastole (improving coronary artery perfusion) and deflates during systole (reducing afterload and improving systemic perfusion). Click here to see a 41 second video illustrating how it works.
Several guidelines recommend placement of an IABP for patients in cardiogenic shock secondary to acute myocardial infarction (AMI), if early revascularization (e.g., CABG) is planned (Class I recommendation). Data behind this recommendation, however, is limited.
The IABP-SHOCK II trial was a randomized, multi-center, open-label study that enrolled 600 patients (598 in the analysis) with cardiogenic shock secondary to AMI (STEMI or NSTEMI). Patients were randomized to the control group (receiving standard therapy; N=298) or the experimental group (receiving IABP; N=300).
No significant difference was found between groups with respect to 30-day mortality (primary end-point), secondary end-points (e.g., time to hemodynamic stabilization, renal function, lactate levels, etc.), or complications (e.g., major bleeding, peripheral ischemic complications, etc.).
Bottom line: Perhaps it is time to reassess the approach to cardiogenic shock secondary to AMI when early revascularization is planned. At this time consultation with local expertise is recommended.
Category: Critical Care
Posted: 1/8/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
The Crashing Cardiac Transplant Patient
Chacko P, Philip S. Emergency department presentation of heart transplant recipients with acute heart failure. Heart Failure Clinics 2009; 5:129-143.
Costanzo MR, et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant 2010; 29:914.956.
Category: Critical Care
Posted: 1/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) or DIHS (Drug-Induced Hypersensitivity Syndrome) is a potentially life-threatening adverse drug-reaction.
Incidence is 1/1,000 to 1/10,00 drug exposures. It occurs 2-6 weeks after the drug is first introduced, distinguishing it from other adverse drug-reactions which typically occur sooner.
The syndrome classically includes:
The most commonly implicated drugs are anticonvulsants (e.g., carbamazepine, phenobarbital, and phenytoin), sulfonamides, and allopurinol.
Recovery is typically complete after discontinuing the offending drug; systemic steroids may promote resolution of the illness.
Cacoub P. et al. The DRESS syndrome: a literature review. Am J Med 2011 Jul;124(7):588-97. http://www.ncbi.nlm.nih.gov/pubmed/21592453
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
Category: Critical Care
Posted: 12/25/2012 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
VV-ECMO for Refractory Hypoxemia
Combes A, et al. What is the niche for extracorporeal membrane oxygenation in severe acute respiratory distress syndrome? Curr Opin Crit Care 2012; 18:527-32.
Category: Critical Care
Posted: 12/18/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Management of patients with severe traumatic brain injury (TBI) typically involves the use of invasive intra-parenchymal pressure monitors. Although use of these monitors is recommended by TBI management guidelines, good quality evidence of benefit is lacking.
A recently published study evaluated the outcomes of TBI patients using a management protocol incorporating either an intracranial pressure (ICP) monitor compared to use of the clinical exam PLUS serial neuroimaging; a total of 324 patients were prospectively randomized into either group.
The primary study outcome was a composite of survival, impaired consciousness, and functional status at both three and six months.
The results of the study did not show a significant difference in the:
Bottom line: This study suggests that clinical exam PLUS serial neuroimaging may perform as well as invasive intra-parenchymal monitors for guiding therapy in TBI patients.
Chestnut, R. et al. A Trial of Intracranial-Pressure Monitoring in Traumatic Brain Injury. NEJM 2012 Dec 12. http://www.ncbi.nlm.nih.gov/pubmed/23234472
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 12/11/2012 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Ultrasound-Guided Pericardiocentesis
L'Italien AJ. Critical cardiovascular skills and procedures in the emergency department. Emerg Med Clin N Am 2013; 31:151-206.
Tirado A, Wu T, Noble VE, et al. Ultrasound-guided procedures in the emergency department - Diagnostic and therapeutic asset. Emerg Med Clin N Am 2013; 31:117-149.
Category: Critical Care
Keywords: anaphylaxis, tryptase, diagnosis (PubMed Search)
Posted: 12/6/2012 by Ellen Lemkin, MD, PharmD
(Updated: 2/1/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Simons EF, Ardusso LE, Bilo MB, et al. 2012 Update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis.
Category: Critical Care
Posted: 11/27/2012 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Managing Critically Ill Patients with AKI
Brienza N, et al. Protocoled resuscitation and the prevention of acute kidney injury. Curr Opin Crit Care 2012; 18:613-622.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int 2012; 2(S):1-138.
Category: Critical Care
Posted: 11/20/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A low-tidal volume (or protective) strategy of mechanical ventilation (i.e., tidal volume of 6-8cc/kg of ideal body weight) has previously been demonstrated to be beneficial in patients with acute respiratory distress syndrome (ARDS).
A meta-analysis was recently performed to determine whether this strategy of mechanical ventilation is also beneficial for patients without lung injury prior to initiation of mechanical ventilation.
Dr. Neto, et al. performed a meta-analysis of 20 studies (total of 2,822 mechanically ventilated patients) comparing a conventional ventilation strategy (average tidal volume was 10.6 cc/kg) to a protective ventilation strategy (average tidal volume was 6.4 cc/kg) of mechanical ventilation.
The authors concluded that patients ventilated with a protective lung-strategy had reductions in:
Bottom-line: This meta-analysis supports the notion that a strategy of low-tidal volume ventilation may have benefits for patients without ARDS, however prospective studies are needed.
Neto, S. et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome. JAMA, Oct. 24/31; 308;16.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 11/13/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Burn Patients and Antibiotic Dosing
Jamal JA, et al. Improving antibiotic dosing in special situations in the ICU: burns, renal replacement therapy and extracorporeal membrane oxygenation. Curr Opin Crit Care 2012; 18:460-71.
Category: Critical Care
Posted: 11/6/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Previous pearls have described the increasing evidence against colloid (e.g., hydroxyethyl starch) use during resuscitation. Now it appears that the crystalloid 0.9% normal saline (NS) may be under fire.
The use of large volumes of NS has been associated with hyperchloremic metabolic acidosis and harm in animal studies. The risk of harm in humans, however, has been less clear.
Bellomo et al. conducted a prospective observational study in which patients being resuscitated in the control group received NS at the clinicians' discretion; i.e., chloride-liberal strategy. The use of NS was restricted in the intervention group, where other less chloride containing fluids were used for resuscitation (e.g., Ringer's Lactate); i.e., a chloride-restrictive strategy.
The authors found that when compared to patients in the chloride-liberal group, the chloride-restrictive group had significantly less rise in baseline creatinine, less overall AKI, and a reduced need for renal replacement therapy.
Bottom line: Although this was only an observational study, the liberal use of normal saline during resuscitation may increase the risk of AKI and renal replacement therapy.
Bellomo, R. et al. Association between a chloride-liberal vs. chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012 Oct 17;308(15):1566-72. doi: 10.1001/jama.2012.13356.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Critical Care
Posted: 10/30/2012 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Serotonin Toxicity in the Critically Ill
Bienvenu OJ, Neufeld KJ, Needham DM. Treatment of four psychiatric emergencies in the intensive care unit. Crit Care Med 2012; 40:2662-2670.
Category: Critical Care
Posted: 10/22/2012 by Haney Mallemat, MD
(Updated: 10/24/2012)
Click here to contact Haney Mallemat, MD
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
Category: Critical Care
Posted: 10/16/2012 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Delirium in the Critically Ill
Bienvenu OJ, Neufeld KJ, Needham DM. Treatment of four psychiatric emergencies in the intensive care unit. Crit Care Med 2012; 40:2662-2670.
Category: Critical Care
Posted: 10/9/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
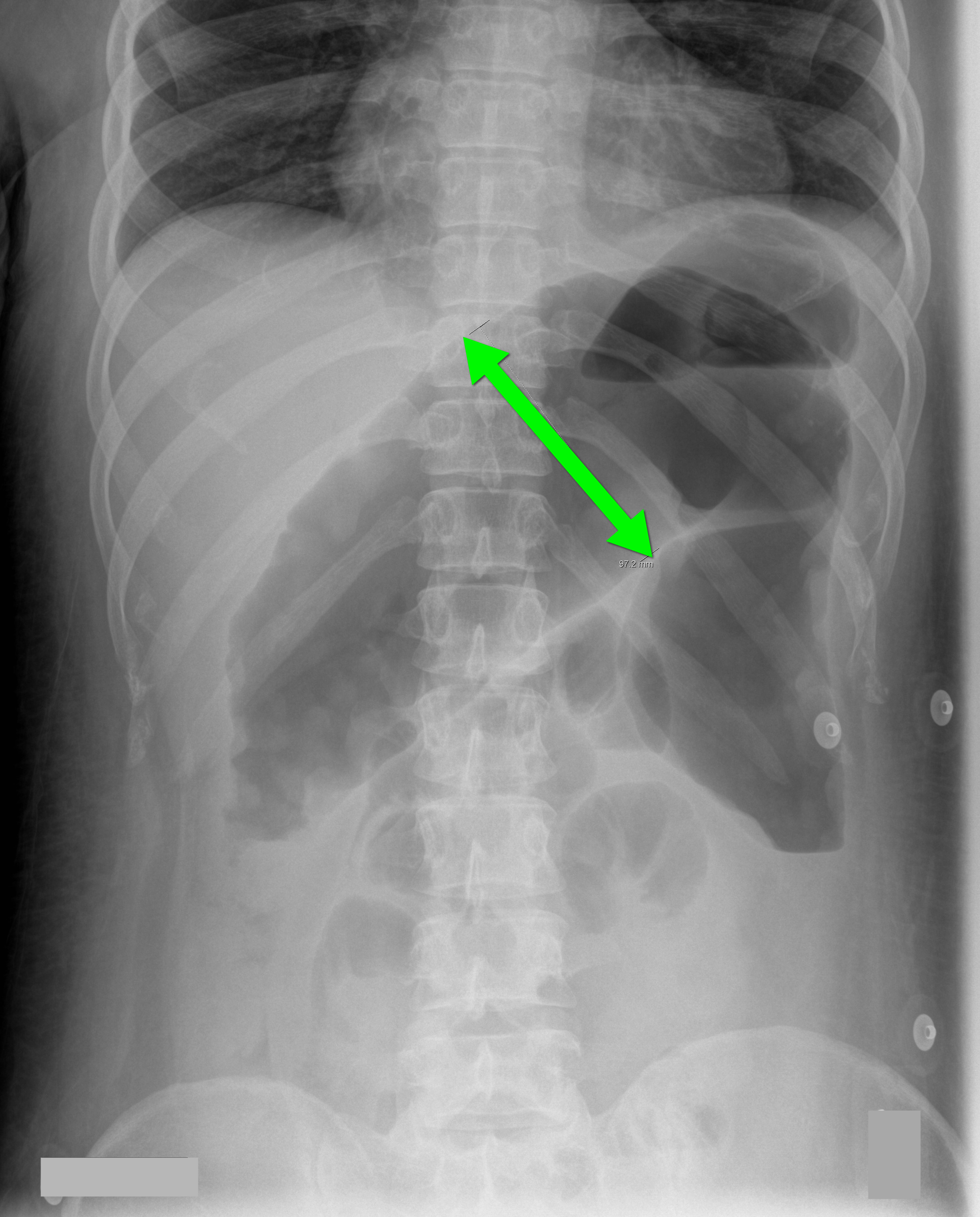
70 year-old male recently treated for community-acquired pneumonia presents with bloody diarrhea, fever, and severe abdominal pain. Abdominal Xray is shown below. Diagnosis?
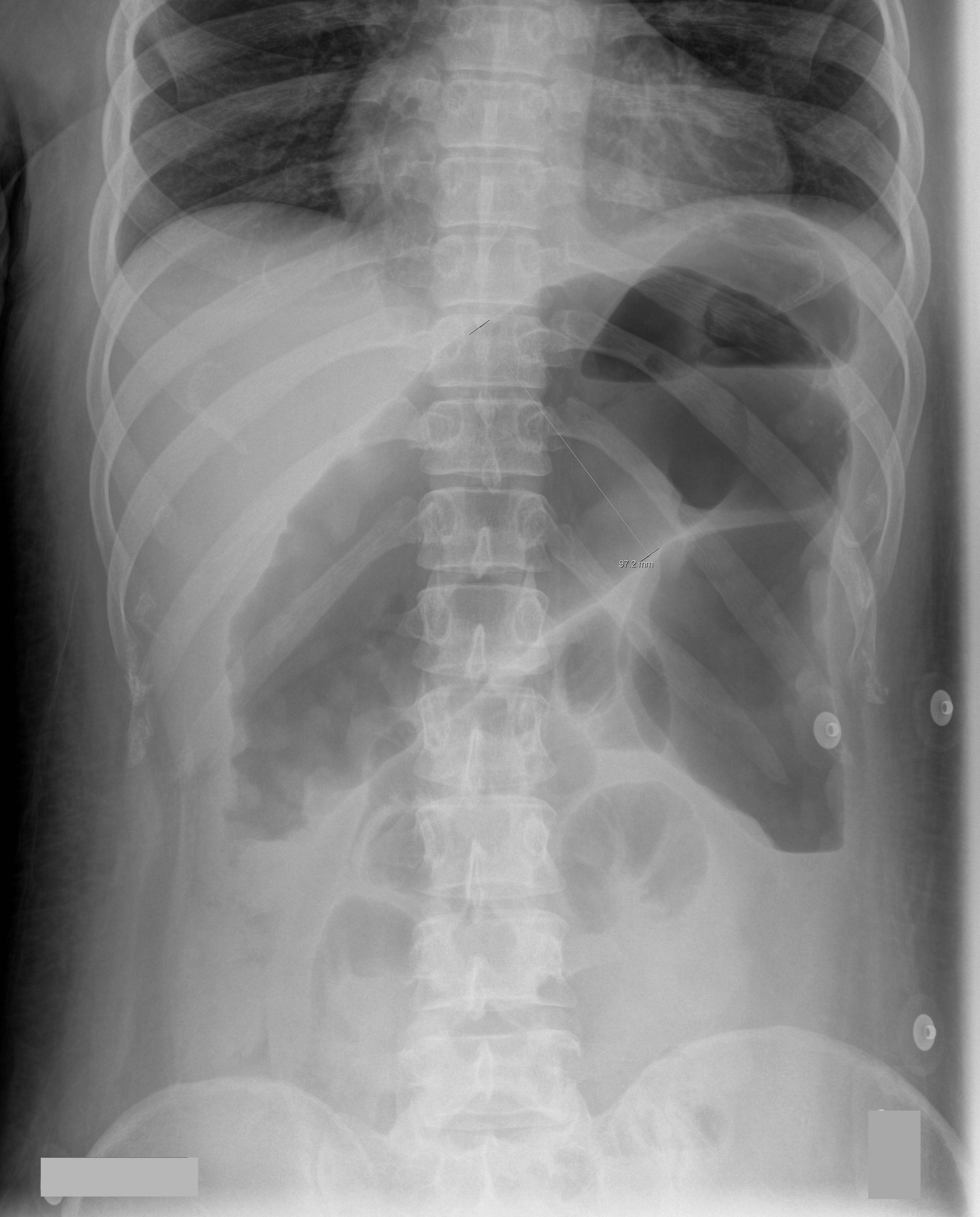
Answer: Toxic Megacolon
Toxic megacolon (TM) is an acute colitis with segmental or total colonic dilation (>6cm) plus systemic toxicity.
Actual incidence is unknown, but it is believed that TM is rising because of increasing cases of Clostridium difficile and the aging population.
The most common etiologies are ulcerative, chron, and pseudomembranous colitis, but other causes exist and can be categorized as:
The diagnosis is made based on clinical evidence of colitis plus evidence of colonic dilation on abdominal XR (diameter > 6cm, loss of haustra, or free intraperitoneal air secondary to perforation) or CT scan (demonstrating dilation or perforation).
Treatment includes:
Autenrieth, D et al. Toxic Megacolon Inflammatory Bowel Dis. 2011 Aug 29.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
