Category: Neurology
Keywords: seizure, status epilepticus, benzodiazepine, antiepileptic, failure (PubMed Search)
Posted: 6/12/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Underdosing of benzodiazepines in status epilepticus may contribute to treatment failure.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: MRI, neuro exam, bladder, gait (PubMed Search)
Posted: 4/24/2019 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Gorter K. Influence of laminectomy on the course of cervical myelopathy. Acta Neurochir (Wien) 1976;33(3Y4):265-281
Category: Neurology
Keywords: 23.4%, mannitol, intracranial hypertension, herniation, IO (PubMed Search)
Posted: 4/11/2019 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Use of IO allows more rapid administration of 23.4% NaCl with no immediate serious complications.
Wang J, Fang Y, Ramesh S, et al. Intraosseous administration of 23.4% NaCl for treatment of intracranial hypertension. Neurocrit Care. 2019;30(2):364-371.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: headache, back pain, misdiagnosis, stroke, intraspinal, epidural, abscess (PubMed Search)
Posted: 3/14/2019 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The rate of serious neurologic conditions missed at an initial ED visit is low. However, the potential harm of misdiagnosis can be substantial.
Category: Neurology
Keywords: spinal cord, physical exam, assessment (PubMed Search)
Posted: 2/28/2019 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Back pain with lower extremity symptoms can be concerning for cauda equina. Some pointers regarding the H&P:
None of these symptoms independently predicts cauda equina syndrome with an accuracy greater than 65%.
Bottom Line: do not depend on any one finding to reliably exclude or confirm cauda equina.
Shapiro S. Medical realities of cauda equina syndrome secondary to lumbar disc herniation. Spine (Phila Pa 1976). 2000;25(3):348-351; discussion 352
Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J. 2011;20(5):690-697. (Review article)
Bell DA, Collie D, Statham PF. Cauda equina syndrome: what is the correlation between clinical assessment and MRI scanning? Br J Neurosurg. 2007;21(2):201-203
Category: Neurology
Keywords: stroke, thrombolytics, tPA (PubMed Search)
Posted: 1/23/2019 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Powers WJ et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49. DOI: 10.1161/STR.0000000000000158
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, volume, ABC/2 (PubMed Search)
Posted: 1/9/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
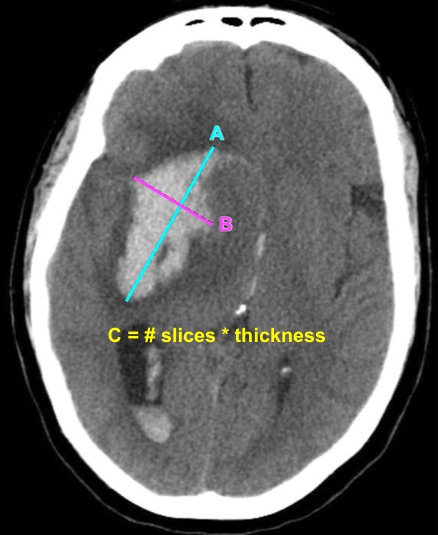
Bottom Line: EPs can reliably estimate ICH volume using the ABC/2 formula. Communicating ICH volume to neurosurgical and neurocritical care consultants can help direct treatment decisions.
Dsouza LB, Pathan SA, Bhutta ZA, et al. ABC/2 estimation in intracerebral hemorrhage: A comparison study between emergency radiologists and emergency physicians. Am J Emerg Med. 2018 Dec 19. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: headache, post concussion syndrome (PubMed Search)
Posted: 12/16/2018 by Brian Corwell, MD
(Updated: 12/23/2018)
Click here to contact Brian Corwell, MD
A previous pearl discussed medication-overuse headache (MOH).
MOH is also known as analgesic rebound headache, drug-induced headache or medication-misuse headache.
It is defined as headache… occurring on 15** or more days per month in a patient with a preexisting headache disorder who has been overusing one or more acute treatment drugs for headache with symptoms for three or more months.
The diagnosis is clinical, and requires a hx of chronic daily headache with analgesic use more than 2-3d per week.
The diagnosis of MOH is supported if headache frequency increases in response to increasing medication use, and/or improves when the overused medication is withdrawn.
The headache may improve transiently with analgesics and returns as the medication wears off. The clinical improvement after wash out is not rapid however, patients may undergo a period where their headaches will get worse. This period could last in the order of a few months in some cases.
The meds can be dc’d cold turkey or tapered depending on clinical scenario.
Greatest in middle aged persons. The prevalence rages from 1% to 2% with a 3:1 female to male ratio.
Migraine is the most common associated primary headache disorder.
** Each medication class has a specific threshold.
Triptans, ergot alkaloids, combination analgesics, or opioids on ten or more days per month constitute medication overuse.
Use of simple analgesics, including aspirin, acetaminophen and NSAIDS on 15 or more days per month constitutes medication overuse.
Caffeine intake of more than 200mg per day increases the risk of MOH.
Consider MOH in patients in the appropriate clinical scenario as sometimes doing less is more!
Category: Neurology
Keywords: ultrasound, lumbar puncture, LP, landmark (PubMed Search)
Posted: 12/12/2018 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider using pre-procedural ultrasound-assistance for all lumbar punctures.
Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2018 Aug 21. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: diplopia, imaging, radiology, CT, ophthalmology (PubMed Search)
Posted: 11/28/2018 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Diplopia can be a challenging complaint to address in the ED. Although not all patients will require imaging, use the simplified table below to help guide the imaging study needed:
| Clinical Situation | Suspected Diagnosis | Imaging Study | |
| Diplopia + cerebellar signs and symptoms | Brainstem pathology | MRI brain | |
| 6th CN palsy + papilledema | Increased intracranial pressure (e.g. idiopathic intracranial hypertension or cerebral venous thrombosis) | CT/CTV brain | |
| 3rd CN palsy (especially involving the pupil) | Compressive lesion (aneurysm of posterior communicating or internal carotid artery) | CT/CTA brain | |
| Diplopia + thyroid disease + decreased visual acuity | Optic nerve compression | CT orbits | |
| Intranuclear ophthalmoplegia | Multiple sclerosis | MRI brain | |
| Diplopia + facial or head trauma | Fracture causing CN disruption | CT head (dry) | |
| Diplopia + multiple CN involvement (3,4,6) + numbness over V1 and V2 of trigeminal nerve (CN5) +/- proptosis | Unilateral, decreased visual acuity | Orbital apex pathology | CT orbits with contrast |
| Uni- or bi-lateral, normal visual acuity | Cavernous sinus thrombosis | CT/CTV brain | |
C.N.: cranial nerve
Margolin E, Lam C. Approach to a Patient with Diplopia in the Emergency Department. J Emerg Med. 2018 Jun;54(6):799-806
Category: Neurology
Keywords: cervical, spine, clearance, triage, nurse, trauma (PubMed Search)
Posted: 11/14/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: ED triage nurses can safely use the Canadian C-Spine Rule. This approach can improve patient care and decrease length of stay in the ED.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: CSF, lumbar puncture, infectious diseases (PubMed Search)
Posted: 10/24/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Manifestations due to neurosyphilis present as one of 3 categories: stroke due to arteritis, masses in the brain (granulomata), and chronic meningitis.
Although serum VDRL/TPPA tests will be positive in almost all patients, it’s important to remember that the diagnosis requires the presence of ALL of the following criteria:
1. positive treponemal (e.g. FTA-ABS, TP-PA) AND nontreponemal (e.g. VDRL, RPR) serum test results
2. positive CSF VDRL OR positive CSF FTA-ABS test result
3. one CSF laboratory test abnormality, such as pleocytosis (cell count >20/μL) or high protein level (>0.5 g/L)
4. clinical symptoms
This is important because the treatment of neurosyphilis is distinctly different from other forms, as it requires admission for IV antibiotics for at least 10 days.
Bonus Pearl: CSF RPR is unreliable as it is more likely to be falsely positive than other specific CSF testing.
Halperin JJ. Neuroborreliosis and Neurosyphilis. CONTINUUM 2018;24(5):1439–1458
Category: Neurology
Keywords: stroke, TIA, antiplatelet, aspirin, clopidogrel, POINT, CHANCE (PubMed Search)
Posted: 10/10/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Does using a combination of aspirin and clopidogrel decrease your patient’s risk of recurrent stroke after a minor ischemic stroke or high risk TIA event?
Bottom Line: The use of DAPT in minor ischemic stroke and high risk TIA reduces the risk of recurrent stroke. However, the duration of DAPT may affect the risk of major hemorrhage.
| Trial | POINT (Johnston et al, NEJM 2018) | CHANCE (Wang et al, NEJM 2013) |
| Location | N. America, Europe, Australia, New Zealand (82.8% enrolled in the US) | China |
| Population | Age ≥ 18 Within 12 hours of sympton onset NIHSS ≤ 3 or TIA with ABCD ≥ 4 | Age ≥ 40 Within 24 hours of symptom onset NIHSS ≤ 3 or TIA with ABCD ≥ 4 |
| Study Group | Clopidogrel 600mg load, then 75mg daily x 90 days + Aspirin 50-325mg daily x 90 days | Clopidogrel 300mg load, then 75mg daily x 90 days + Aspirin 75mg daily x 21 days |
| Control Group | Aspirin 50-325mg daily x 90 days + Placebo | Aspirin 75mg daily x 90 days + Placebo |
| Primary Efficacy Outcome | Major ischemic event defined as cardiovascular death, stroke, MI | Stroke (ischemic or hemorrhagic) |
| Primary Safety Outcome | Major hemorrhage defined as symptomatic ICH, intraocular bleeding causing vision loss, transfusion ≥ 2 units PRBCs, hospitalization/death related to hemorrhage | Moderate hemorrhage defined as transfusion requirement Severe hemorrhage defined as fatal, ICH, hemodynamic compromise |
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: weakness, sensory symptoms, MRI, LP (PubMed Search)
Posted: 9/26/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Frohman EM, Wingerchuk DM. Clinical practice. Transverse myelitis. N Engl J Med. 2010;363(6):564-572.
de Seze J, Lanctin C, Lebrun C, et al. Idiopathic acute transverse myelitis: application of the recent diagnostic criteria. Neurology. 2005;65(12):1950-1953.
Category: Neurology
Keywords: shingles, weakness, infection (PubMed Search)
Posted: 8/22/2018 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, anticoagulation, low molecular weight heparin, LMWH, UFH (PubMed Search)
Posted: 8/8/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: LMWH appear to be similar in efficacy and safety compared with UFH for the management of CVT.
Al Rawahi B, Almegren M, Carrier M. The efficacy and safety of anticoagulation in cerebral vein thrombosis: a systematic review and meta-analysis. Thromb Res 2018;169:135-9. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: infarct, paralysis, numbness (PubMed Search)
Posted: 7/25/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
An infarct of the spinal cord is technically considered a stroke
The most common risk factor is a recent aortic surgery. Can also occur with straining and lifting (rare)
Patients will present with symptoms of spinal cord involvement with a hyperacute onset (less than 4 hours)
Although the “classic” presentation is anterior cord syndrome (flaccid paralysis, dissociated sensory loss (pinprick and temperature), preserved dorsal column function), patients may present with loss of all functions below the level of infarct due to spinal shock, confusing the clinical picture.
The most common level is T10
Rabinstein AA. Vascular myelopathies. Continuum (Minneap Minn). 2015;21(1 Spinal Cord Disorders):67-83.
Category: Neurology
Keywords: capacity, dementia, altered mental status, medicolegal, ethics (PubMed Search)
Posted: 6/27/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Medical decision-making capacity refers to the patient’s ability to make informed decisions regarding their care, and emergency physicians are frequently required to assess whether a patient possess this capacity. Patients with acute or chronic neurological diseases (such as dementia) may lack this capacity, and this should be identified, especially in life-threatening situations. The patient must have the ability to:
communicate a consistent choice
understand (and express) the risks, benefits, alternatives and consequences
appreciate how the information applies to the particular situation
reason through the choices to make a decision
There are numerous tools that may help with this assessment, but none has been validated in the ED. Be careful of determining that the patient lacks capacity just because of the diagnosis they carry.
BONUS PEARLS:
Capacity is a fluid concept; a patient may have the capacity to make simple decisions but not more complex ones. Capacity may also change over time
Psychiatry consultation to determine capacity is not obligatory but may be utilized for a second opinion.
Rodgers JJ, Kass JS. Assessment of Medical Decision-making Capacity in Patients With Dementia. Continuum 2018;24(3):920–925.
Category: Neurology
Keywords: Syncope, neurological, neuroimaging, CT, MRI (PubMed Search)
Posted: 6/13/2018 by WanTsu Wendy Chang, MD
(Updated: 2/1/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider obtaining neuroimaging in patients presenting with syncope only if clinical features suggest probable neurological syncope.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: myelopathy, myelitis, physical exam (PubMed Search)
Posted: 5/23/2018 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Lhermitte’s phenomenon is as a sign of cervical spinal cord demyelination. It is considered positive if flexion of the neck causes a tingling sensation moving down the limbs or trunk, and may be reported as a symptom or elicited as a sign. This is due to stretching of the dorsal column sensory fibers, the commonest cause of which is multiple sclerosis. Other causes include other myelopathies, such as B12 deficiency, radiation and toxic (due to chemotherapy) or idiopathic myelitis. Its sensitivity is low at 16%, but its specificity for myelopathy is high at 97%.
Kempster PA, Rollinson RD. The Lhermitte phenomenon: variant forms and their significance. J Clin Neurosci 2008;15(4):379–81.
Khare S, Seth D. Lhermitte's Sign: The current status. Ann Indian Acad Neurol. 2015 Apr-Jun; 18(2): 154-156.
