Category: Visual Diagnosis
Keywords: Herpes Zoster Ophthalmicus; Hutchinson's sign (PubMed Search)
Posted: 2/6/2017 by Hussain Alhashem, MBBS
(Updated: 2/1/2026)
Click here to contact Hussain Alhashem, MBBS
24-year-old male with a history of Wagner's Granulomatosis, currently on Cellcept (Mycophenolate Mofetil) and high dose prednisolone, presented with two days of sore throat, malaise and the lesions shown in the picture. What is the diagnosis?


Answer: Herpes Zoster with Hutchinson's sign.
- This patient is presenting with a well demarcated eruptive skin lesion involving the tip of the nose and half of the lip and palate. This lesion is suggestive of Herpes Zoster with Hutchinson's sign.
- Hutchinson's sign is associated with a high rate of corneal denervation and ocular involvement. Some studies suggest that up to 100% of patients with Hutchinson's sign will present with a serious intraocular pathology.
- In addition to starting systemic antiviral therapy, all patients who present with Hutchinson's sign need an immediate and complete ophthalmologic evaluation including a complete slit lamp examination.
Adam, R. S., Vale, N., Bona, M. D., Hasanee, K., & Farrokhyar, F. (2010). Triaging herpes zoster ophthalmicus patients in the emergency department: do all patients require referral?. Academic Emergency Medicine, 17(11), 1183-1188.
Van Dyk, M., & Meyer, D. (2010). Hutchinson's sign as a marker of ocular involvement in HIV-positive patients with herpes zoster ophthalmicus. SAMJ: South African Medical Journal, 100(3), 172-174.
Category: Visual Diagnosis
Posted: 1/2/2017 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 36-year-old male, who recently immigrated from Africa, presented to the ED with fever, rash, cough and shortness of breath. He was noted to be febrile to 39.0 C. The rash is disseminated but present mainly in his trunk as shown in the picture.

Disseminated Varicella Zoster Virus (VZV) Infection
- The patient is presenting with a rash in different stages, associated with fever and signs of systematic involvement, indicating a disseminated varicella infection.
- Definitive diagnosis of disseminated VZV infection is made by detecting its DNA in multiple anatomic sites.
- The most common complication of VZV infection in immunocompetent adults is VZV pneumonia. Early detection of VZV pneumonia can be done with bronchoalveolar lavage and PCR testing.
- Treatment is with IV acyclovir and is more effective if started within 24 hours of the beginning of symptoms. In cases that require prolonged treatment, gene sequencing should be done to detect resistant strains.
Beby?Defaux, Agnès, et al. "Disseminated varicella with multiorgan failure in an immunocompetent adult." Journal of medical virology 81.4 (2009): 747-749.
Category: Visual Diagnosis
Posted: 12/12/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
30 Year-old female presents to the ED for a rash. The rash started suddenly, mainly in her extremities and it is painful. The patient denied having fever or chills. Her past medical history is unremarkable. She admits to using cocaine frequently. The rash is shown in the picture.

Levamisole-Induced Vasculitis
- Levamisole is an antihelmintic drug that was banned by the US Food and Drug Administration in 2000 because of its adverse effects.
- It is added to cocaine to increase its weight and potentiate its effect.
- Patients usually present with painful purpuric rash without central necrosis.
- Laboratory values might include agranulocytosis and elevated ESR.
- Treatment is by cessation of cocaine use.
- Because Levamisole is strongly associated with agranulocytosis, corticosteroids should be avoided to prevent immunosuppression.
Roberts, Jordan A., and Patricia Chévez-Barrios. "Levamisole-induced vasculitis: a characteristic cutaneous vasculitis associated with levamisole-adulterated cocaine." Archives of pathology & laboratory medicine 139.8 (2015): 1058-1061.
Category: Visual Diagnosis
Keywords: Intussusception, pediatric, ultrasound (PubMed Search)
Posted: 11/21/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
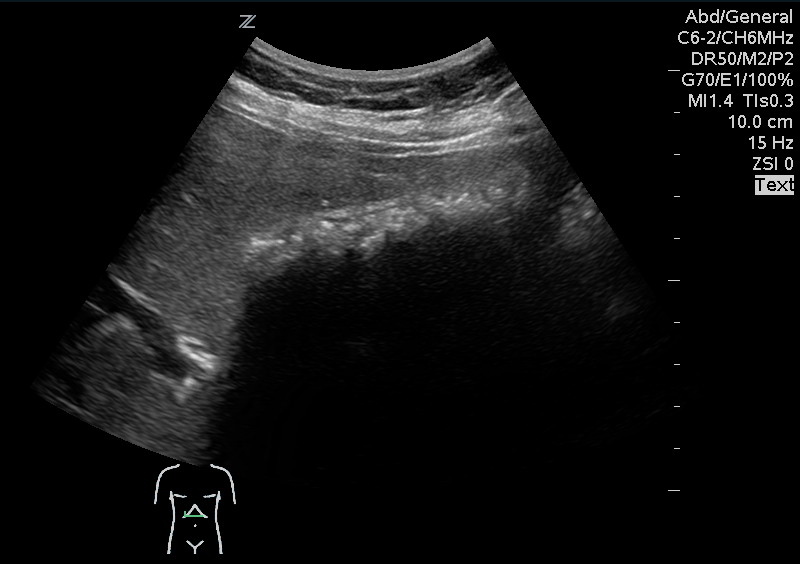
A 15 months old male with no past medical history, presenting with two days of decreased oral intake and decreased urine output. The exam was notable for minimal tenderness of abdomen. During an oral fluid challenge in the ED, the patient had a single episode of bilious vomiting. The ED physician ordered an ultrasound study and the results are shown below. What is the diagnosis?

Diagnosis: Intussusception.
- The use of point of care ultrasound in the ED shortens the time to diagnosis and to definitive treatment. It has a sensitivity of 98-100% even if done by an inexperienced sonographer.
- To diagnose intussusception in the pediatric population, use the High-frequency linear probe for a better image quality. Start with scanning the right upper quadrant, and then move down to scan all four quadrants.
- Classic ultrasound findings include either a Donut-shaped or a Pseudo-kidney appearance, seen as a hypoechoic outer ring and a hyperechoic center. Other variants include; Mesenteric Crescent, where the inner loop will have a crescent hyperechoic appearance with few hypoechoic areas representing lymph nodes, or Central Limb of the Intussusceptum, where a fluid collection is present in the central limb of the intussusceptum instead of a collapsed limb.
- Utilize the US doppler to check for blood flow to the intestinal loops. Diminished blood flow correlates with irreducibility.
Del-Pozo, Gloria, et al. "Intussusception in children: current concepts in diagnosis and enema reduction." Radiographics 19.2 (1999): 299-319.
Category: Visual Diagnosis
Posted: 10/31/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
30 year old female presents with a painful finger for 1 week. Finger exam showed the following. What is the diagnosis ?

Herpetic whitlow
- It is caused by either HSV 1 or 2.
- Infection is usually transmitted by direct unprotected contact.
- Healthcare workers are at risk of contracting the infection if appropriate preventative measures were not taken when dealing with patients who have the infection.
- Diagnosis is mainly clinical. Tzank smears can be done to confirm the diagnosis if in doubt.
- Treatment with Acyclovir is thought to shorten the duration of the infection and prevent recurrence if started within 72 hours of beginning of symptoms.
- Incision of the vesicular lesion is contraindicated and can cause severe bacterial superinfection.
McDonald, Lucas S., et al. "Hand infections." The Journal of hand surgery36.8 (2011): 1403-1412.
Category: Visual Diagnosis
Posted: 10/3/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 41 year old female presenting with intermittent RUQ abdominal pain for 1 week. An ultrasound of the right upper quadrant was performed. What is the diagnosis ?

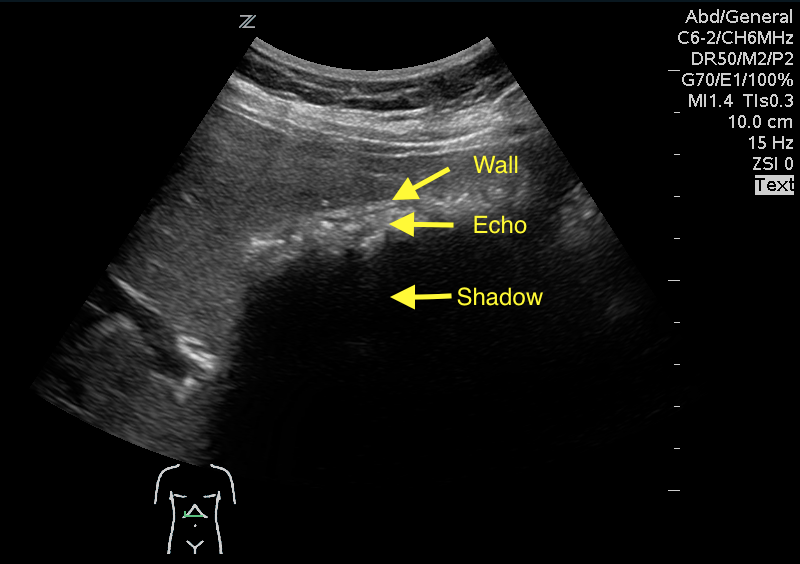
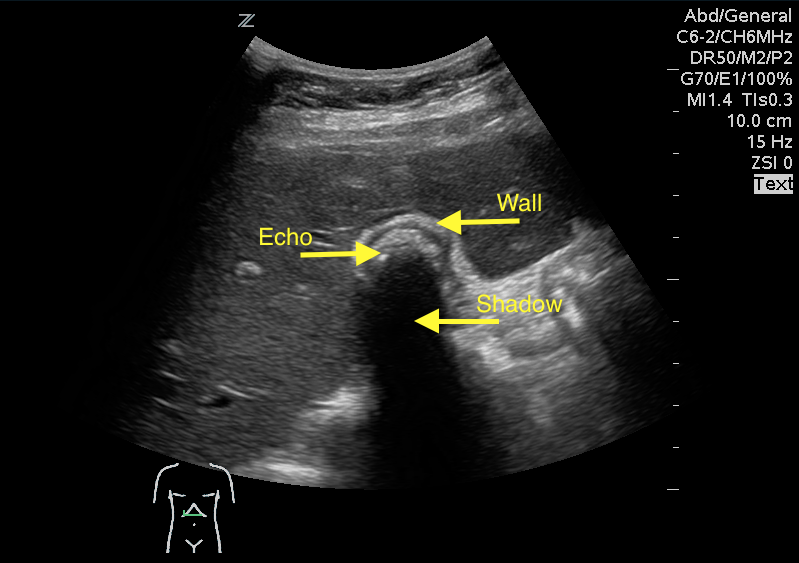
Answer: WES sign
WES sign stands for Wall Echo Shadow sign. It is a triad of:
1- Thick echogenic gall bladder wall (W)
2- Echoes filling the gallbladder (E)
3- A posterior acoustic shadow (S)
Rybicki, F. J. (2000). The WES Sign 1. Radiology, 214(3), 881-882.
Category: Visual Diagnosis
Posted: 9/19/2016 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 67 year old female with history of CVA, presented from a nursing home with RUQ abdominal pain and inablitiy to tolerate PO for 3 days. A CT scan of her abdomen was obtained. What is the diagnosis ?

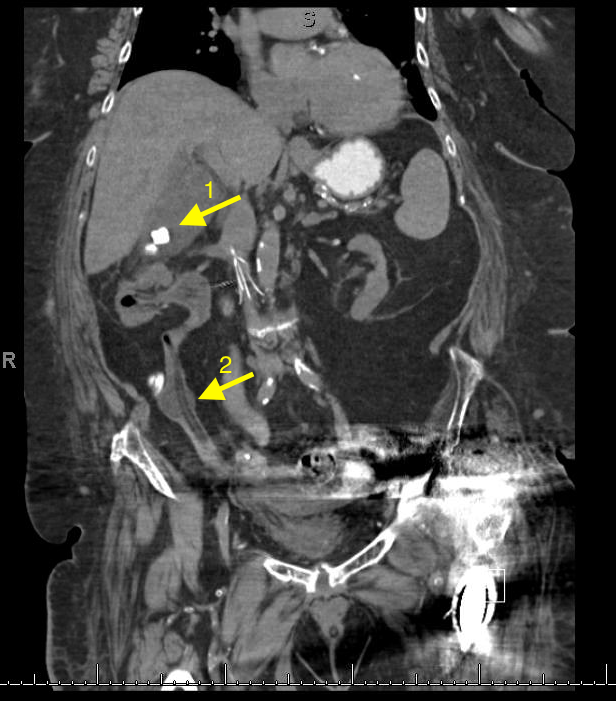
1- Cholecystitis
Ultrasound remains the best modality to test for cholecystitis. However, CT scans can still be obtained for non-classic presentations. The negative predictive value of CT is still relatively high. CT has a negative predictive value of 89%, compared to 97% to that of ultrasound. The absence of cholecysitis on CT will help the argument against the diagnosis, but if the suspicion is high an ultrasound study should still be obtained.
Things to look for on an abdominal CT that are suggestive of cholecysitis:
Gallbladder distension ( >5 cm width, >8 cm length).
Wall thickening ( >4mm thickness).
Pericholecystic fat stranding.
Presence of gallstones.
2- An inflated foley catheter in the ureter!
Ureteric insertion of foley catheters is a very rare complication of foley catheterization. There are no clear predisposing factors to this complication. However, it is thought that the presence of an underlying anatomical deformity (e.g. abnormal ureteric insertion site) might put the patient at a higher risk for it. Inflating a balloon in the ureter might result in severe ureteric injury. A suggested method to prevent this kind of injury is to perform bladder aspiration to insure balloon positioning prior to inflation.
References
1- Shakespear, Jonathan S., Akram M. Shaaban, and Maryam Rezvani. "CT findings of acute cholecystitis and its complications." American Journal of Roentgenology 194.6 (2010): 1523-1529.
2- Kim, Myung Ki, and Kwangsung Park. "Unusual complication of urethral catheterization: a case report." Journal of Korean medical science 23.1 (2008): 161.
