Category: Critical Care
Keywords: Cardiac arrest, neruo (PubMed Search)
Posted: 1/15/2019 by Daniel Haase, MD
(Updated: 1/19/2019)
Click here to contact Daniel Haase, MD
--Late awakening (>48h after sedation held) was common (78/402) in patients with cardiac arrest in prospective cohort study
--Poor prognostic signs of discontinuous (10-49% suppression) EEG and absent brain stem reflexes were independently associated with late awakening. Use of midazolam also associated with late awakening
--Late awakeners had good functional outcome when compared to early awakeners
DON'T NEUROPROGNOSTIC EARLY (OR IN ED)!
And traditional poor prognostic signs may not be as poor as previously thought!
------------------
Rey A, Rossetti AO, Miroz JP, et al. Late Awakening in Survivors of Postanoxic Coma: Early Neurophysiologic Predictors and Association With ICU and Long-Term Neurologic Recovery. Critical Care Medicine: January 2019 - Volume 47 - Issue 1 - p 85–92
Category: Critical Care
Keywords: RV dysfunction, APRV, echo, ultrasound (PubMed Search)
Posted: 8/1/2017 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
--RV systolic function is negatively affected by high RV afterload
--High mean airway pressures on the ventilator (particularly in modes such as APRV [airway pressure release ventilation]) can induce RV dysfunction
*****CLICK BELOW FOR A GREAT CASE!!!*****
A 25yoF with ARDS is on APRV (36/0 and 5/0.5). She is on norepi to maintain a MAP >65. A bedside echo reveals a dilated, dysfunctional RV.
--Open "A4C end diastole"
Measurement of TAPSE confirms the RV dysfunction, but also reveals the cause.
--Open "TAPSE"
Every 5th beat, the TAPSE significantly improves to "normal" range. The four beats inbetween are abnormal. The 5th normal beat coincides with the APRV relase, when airway pressures are zero! Thus, this change in RV function is from the ventilator alone. The TAPSE decreases by almost 40%!
--Open "TAPSE measured"
Be careful with high mean airway pressures in patients with known or suspected RV dysfunction. This is why we try to avoid intubation in HD significant pulmonary embolism!
Category: Critical Care
Keywords: Sepsis, Septic Shock, Fluid resuscitation (PubMed Search)
Posted: 1/31/2017 by Daniel Haase, MD
(Updated: 2/18/2017)
Click here to contact Daniel Haase, MD
At the Society of Critical Care Meeting (SCCM) this month, updates to the Surviving Sepsis Guidelines were released. Recommendations include:
--Initial 30mL/kg crystalloid resuscitation with frequent reassessment of fluid responsiveness using dynamic (not static) measures [goodbye CVP/ScvO2!]
--Initiation of broad-spectrum antibiotics within ONE hour of sepsis recognition [two agents from different classes]
--Further hemodynamic assessement (e.g. echo for cardiac function) if clinical assessment does not reveal the type of shock [get out the ultrasound!]
Rhodes A, Evans LE, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017 Jan 18.
Category: Critical Care
Keywords: Sepsis, Antibiotics, Septic Shock (PubMed Search)
Posted: 1/10/2017 by Daniel Haase, MD
(Updated: 2/18/2017)
Click here to contact Daniel Haase, MD
--Recent meta-analysis comparing continuous infusion versus intermittent bolus dosing of beta-lactam antibiotics demonstrates mortality benefit (NNT = 15) in patients with severe sepsis or septic shock. (1)
--Consider beta-lactam continuous infusion on your septic patients if your hospital pharmacy allows
[Thanks to Anne Weichold, CRNP for providing the article for this pearl!]
--Beta-Lactams are time-dependent antibiotics (i.e. longer time above MIC = more time killing) annd continuous infusions should have concentrations consistently above MIC.
--Previous studies not powered to demonstrate mortality benefit, but showed pharmocokinetic improvement and higher rates of clinical cure (2)
Pratical aspects
This means the patient will require an additional IV most of the time
Most hospitals do not have a pharmacy protocol for infusion of most extended-spectrum B-lactams
1. Roberts JA, Abdul-Aziz MH, Davis JS, et al. Continuous versus Intermittent B-Lactam Infusion in Severe Sepsis. Am J Resp Crit Care Med. 2016; 194 (6): 681-91.
2. Abdul-Aziz MH, Sulaiman H, Mat-Nor MB, et al. Beta-Lactam Infusion in Severe Sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med. 2016; 42 (10) 1535-45.
Category: Critical Care
Keywords: Intracranial hemorrhage, ICH, PCC, FFP, vitamin K antagonist, VKA, coumadin, warfarin (PubMed Search)
Posted: 12/20/2016 by Daniel Haase, MD
(Updated: 2/18/2017)
Click here to contact Daniel Haase, MD
The Neurocritical Care Society and Society of Critical Care Medicine just came out with new Guidelines for Reversal of Antithrombotics in Intracranial Hemorrhage (ICH) [1]
--PCC is now recommended over FFP in reversal of vitamin K antagonists (VKA) with elevated INR. Either should be co-administered with 10mg IV vitamin K. (Strong recommendation, moderate quality evidence)
TAKE AWAY: PCC should be probably be given over FFP in VKA-ICH when available
--Seems to be primarily based on a recent Lancet trial, which was stopped early due to safety concerns [2], but demonstrated more rapid reversal of INR and less hematoma expansion.
--In that study, all hematoma expansion related deaths occurred in the FFP group.
--Study was not designed to look at 90 day outcome, but trended towards improved survival.
1. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: Executive Summary. A Statement for Healthcare Professionals From the Neurocritical Care Society and the Society of Critical Care Medicine. Frontera JA, Lewin JJ 3rd, et al. Crit Care Med. 2016 Dec;44(12):2251-2257.
2. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): a randomised trial. Steiner T, Poli S, et al. Lancet Neurol. 2016 May;15(6):566-73.
Category: Critical Care
Keywords: Pulmonary embolism, syncope (PubMed Search)
Posted: 11/29/2016 by Daniel Haase, MD
(Updated: 11/30/2016)
Click here to contact Daniel Haase, MD
--In this study, PE was diagnosed in ~17% of patients hospitalized for syncope (though this represents only ~4%% of patients presenting to the ED with syncope).
--Patients with PE were more likely to have tachypnea, tachycardia, relative hypotension, signs of DVT, and active cancer -- take a good history and do a good physical exam!
--Consider risk stratifying (Wells/Geneva) and/or performing a D-dimer (i.e "rule out" PE) on your syncope patients, particularly when no alternative diagnosis is apparent.
--The 17.3% prevalence of PE is in admitted patients only (in Italy). Again, 3.8% of patients presenting with syncope had PE diagnosed (though the study was not designed to study the prevalence of PE in patients presenting to the ED with syncope).
--Think about this! They only admitted 27.7% of patients with syncope!!! This suggests they only admitted sick patients with significant comorbidities.
--The vast majority of patients were ruled out by history, physical and ancillary testing and sent home (72.3%).
--Think about PE in syncope patients and do a reasonable work up (i.e. not all hospitalized PE patients need a CTA or V/Q)
Prevalence of Pulmonary Embolism among Patients Hospitalized for Syncope. Prandoni P, Lensing AW, et al. PESIT Investigators.. N Engl J Med. 2016 Oct 20;375(16):1524-1531
Category: Critical Care
Posted: 11/8/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
It's Election Day in the US, so here are some interesting facts about Presidential causes of death:
George Washington likely died from epiglottitis on 12/14/1799
CLICK BELOW FOR MORE INTERESTING FACTS!
Other interesting facts:
Leading causes of death:
Category: Critical Care
Keywords: ECMO, PE, hypotension (PubMed Search)
Posted: 10/18/2016 by Daniel Haase, MD
(Updated: 4/10/2018)
Click here to contact Daniel Haase, MD
--Massive PE is defined as PE with obstructive shock (hypotension [SBP <90] or end-organ malperfusion)
--Consider venoarterial (VA) ECMO in massive PE for hemodynamic support, particularly prior to intubation
--VA ECMO may prevent intubation/mechanical ventilation, surgical intervention, systemic and local thrombolysis
--Patients on VA ECMO require systemic anti-coagulation to prevent arterial embolism. So, patients with relative and absolute contraindications to catheter-directed and systemic thrombolysis should be considered for VA ECMO for HD support while AC works.
--Intubating already hemodynamically tenuous patients is dangerous and increases in intra-thoracic pressure worsens RV failure and suppressing patient's catecholamine drive with sedation during RSI may also worsen hemodynamics.
--Frequently, patients who get VA ECMO will not require surgical embolectomy as the clot burden will resolve after a few days of heparin. And RV function with improve as demonstrated by serial echocardiography
--A recent review showed an overall survival of 70% in VA ECMO patients for massive PE. This included patients already in cardiac arrest. Review included case series, cohorts, but no RCTs.
1. Extracorporeal membrane oxygenation in acute massive pulmonary embolism: a systematic review. Yusuff HO, Zochios V, Vuylsteke A. Perfusion. 2015 Nov;30(8):611-6. doi: 10.1177/0267659115583377. Epub 2015 Apr 24. Review.
Category: Critical Care
Keywords: Fluids, Fluid resuscitation, Metabolic Acidosis (PubMed Search)
Posted: 9/27/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
TAKE HOME POINTS:
-- High chloride load is associated with adverse outcomes in large-volume resuscitation (>60mL/kg in 24h), including increased risk of death [1]
-- Avoid supraphysiologic chloride solutions (i.e. normal saline) when resuscitation volumes are likely to exceed 60mL/kg (e.g. sepsis, DKA)
-- Hyperchloremic metabolic acidosis (HMA) is frequently associated with large-volume resuscitation, particularly with normal saline (0.9% NS) [2]
--HMA can result in decreased renal blood flow and renal cortical hypoperfusion, even in healthy volunteers [3]
-- Chloride load is also associated with acute kidney injury in this study, but this effect goes away once severity of illness is controlled.
-- It is not clear why increased chloride load is associated with increased mortality
-- Consider more "physiologic" fluids, such as plasmalyte A
1. Sen A, Keener CM, et al. Chloride Content of Fluids Used for Large-Volume Resuscitation Is Associated With Reduced Survival. Crit Care Med. 2016 Sep 15. [Epub ahead of print]
2. Kellum JA. Saline-induced hyperchloremic metabolic acidosis. Crit Care Med. 2002 Jan;30(1):259-61.
3. Chowdhury AH, Cox EF, et al. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012 Jul;256(1):18-24.
Category: Critical Care
Keywords: Intracerebral hemorrhage, intraparenchymal hemorrhage, ICH, IPH, hypertensive emergency, blood pressure, neurocritical care, nicardipine (PubMed Search)
Posted: 8/15/2016 by Daniel Haase, MD
(Updated: 9/6/2016)
Click here to contact Daniel Haase, MD
--Aggressive BP management (SBP <140) in atraumatic intracerebral hemorrhage (ICH) does NOT signifcantly improve mortality or disability compared with traditional goal (SBP <180) [1]
--However, a lower goal (SBP <140) has been shown to decrease hematoma size and be safe compared to a higher goal (SBP <180) [2]
The recently published ATACH-2 study investigated aggressive BP control in hypertensive acute atraumatic ICH/IPH (intraparenchymal hemorrhage). [1]
--Control group SBP 140-179 mmHg vs. intervention group SBP 110-139 mmHg with nicardipine infusion (control group actually had SBP 140-150 vs. intervention group SBP 120-130 most of the time).
--Study stopped early for futility. No difference in mortality or modified Rankin.
Previously, INTERACT2 demonstrated that aggressive SBP management (<140) was safe, decreasing hematoma expansion leading to a change in some individuals' practice. [2]
1. Qureshi AI, Palesch YY, et al; ATACH-2 Trial Investigators and the Neurological Emergency Treatment Trials Network. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N Engl J Med. 2016 Jun 8. [Epub ahead of print] PubMed PMID: 27276234.
2. Anderson CS, Heeley E, et al; INTERACT2 Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013 Jun 20;368(25):2355-65. doi: 10.1056/NEJMoa1214609. Epub 2013 May 29. PubMed PMID: 23713578.
Category: Critical Care
Keywords: PPI, GI bleed, UGIB, GI hemorrhage (PubMed Search)
Posted: 6/7/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
1. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012 Mar;107(3):345-60; quiz 361. doi: 10.1038/ajg.2011.480. Epub 2012 Feb 7. Review. PubMed PMID: 22310222.
2. Barkun AN, et al; International Consensus Upper Gastrointestinal Bleeding Conference Group. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010 Jan 19;152(2):101-13. doi: 10.7326/0003-4819-152-2-201001190-00009. PubMed PMID: 20083829.
3. Sachar H, Vaidya K, Laine L. Intermittent vs continuous proton pump inhibitor therapy for high-risk bleeding ulcers: a systematic review and meta-analysis. JAMA Intern Med. 2014 Nov;174(11):1755-62. doi: 10.1001/jamainternmed.2014.4056. Review. PubMed PMID: 25201154; PubMed Central PMCID: PMC4415726.
4. Neumann I, et aI. Comparison of different regimens of proton pump inhibitors for acute peptic ulcer bleeding. Cochrane Database Syst Rev. 2013 Jun 12;(6):CD007999. doi: 10.1002/14651858.CD007999.pub2. Review. PubMed PMID: 23760821.
5. Pantoprazole. Micromedex 2.0. Truven Health Analytics, Inc. Available at http://micromedexsoultsions. Accessed June 7, 2016.
Category: Critical Care
Keywords: Zika, Guillain-Barre, GBS, ITP, Critical Care (PubMed Search)
Posted: 5/10/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Zika virus has received significant media attention in the US due to its recent link with teratogenicity. But Zika is also associated with critical and life-threatening complications, including death. Differentiating it from other Flavivirus diseases such as Dengue or Chikungunya can be challenging.
Diagnosis
Complications
1. Petersen LR, Jamieson DJ, Powers AM, Honein MA. Zika Virus. N Engl J Med. 2016 Apr 21;374(16):1552-63. doi: 10.1056/NEJMra1602113. Epub 2016 Mar 30. Review. PubMed PMID: 27028561.
2. LaBeaud, AD. Zika virus infection: An overview. uptodate.com. Accessed 5/10/2016.
3. Cao-Lormeau VM, et al. Guillain-Barr Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016 Apr 9;387(10027):1531-9. doi: 10.1016/S0140-6736(16)00562-6. Epub 2016 Mar 2. PubMed PMID: 26948433.
4. Centers for Disease Control and Prevention. Zika virus - What clinicians need to know? Clinician Outreach and Communication Activity (COCA) Call, January 26, 2016. Available at: http://emergency.cdc.gov/coca/ppt/2016/01_26_16_zika.pdf. Accessed May 10, 2016.
Category: Critical Care
Keywords: seizure, status epilepticus, pregnancy (PubMed Search)
Posted: 4/13/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Disclaimer: Talking about seizures/status that is NOT due to eclampsia
TAKE HOME: While no AEDs are completely safe in pregnancy, treatment and stabilization of maternal status epilepticus is paramount for fetal health. Involve neurology/epileptology and OB/maternal-fetal medicine.
1. Hern ndez-D az S, et al; North American AED Pregnancy Registry; North American AED Pregnancy Registry. Comparative safety of antiepileptic drugs during pregnancy. Neurology. 2012 May 22;78(21):1692-9.
2. McElhatton PR. The effects of benzodiazepine use during pregnancy and lactation. Reprod Toxicol. 1994 Nov-Dec;8(6):461-75.
3. Lexicomp online accessed via uptodate.com.
Category: Critical Care
Keywords: Pharmacology, Hypertension, Vasoactive (PubMed Search)
Posted: 3/15/2016 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
There are multiple vasoactive infusions available for acute hypertensive emergencies, many having serious side effect profiles or therapeutic disadvantages.
Clevidipine (Cleviprex) is rapidly-titratable, lipid-soluable dihydropyridine calcium channel blocker which has become increasingly used in the ICU in recent years [1]:
ECLIPSE trial compares clevidipine, nicardipine, nitroglycerin and nitroprusside in cardiac surgery patients. .
Clevidipine was as effective as nicardipine at maintaining a pre-specified BP range, but superior when that BP range was narrowed (also studied in ESCAPE-1 and ESCAPE2 with similar results) [2-3]
TAKE-HOME: Clevidipine is an ultra short-acting, rapidly-titratable vasoactive with favorable cost, pharmacokinetics, and side-effect profile. Consider its use in hypertensive emergencies.
1. Lexicomp (accessed via UpToDate on 3/15/2016)
2. Aronson S, Dyke CM, Stierer KA, et al, "The ECLIPSE Trials: Comparative Studies of Clevidipine to Nitroglycerin, Sodium Nitroprusside, and Nicardipine for Acute Hypertension Treatment in Cardiac Surgery Patients," Anesth Analg, 2008, 107(4):1110-21.
3. ESCAPE-2 Study Group.Treatment of acute postoperative hypertension in cardiac surgery patients: an efficacy study of clevidipine assessing its postoperative antihypertensive effect in cardiac surgery-2 (ESCAPE-2), a randomized, double-blind, placebo-controlled trial.Anesth Analg. 2008 Jul;107(1):59-67.
Category: Critical Care
Keywords: Pulmonary Embolism, PE, submassive PE, thrombolysis, catheter-directed thromblysis, thrombectomy, echo (PubMed Search)
Posted: 1/19/2016 by Daniel Haase, MD
(Updated: 2/10/2016)
Click here to contact Daniel Haase, MD
What classifies "submassive PE"?
Submassive PE has early benefit from systemic thrombolysis at the cost of increased bleeding [1].
Ultrasound-accelerated, catheter-directed thrombolysis (USAT) [the EKOS catheters] has been shown to be safe, with low mortality and bleeding risk, as well as immediately improved RV dilation and clot burden [2-4]. USAT may improve pulmonary hypertension [4].
USAT is superior to heparin/anti-coagulation alone for submassive PE at reversing RV dilation at 24 hours without increased bleeding risk [5].
Long-term studies evaluating chronic thromboembolic pulmonary hypertension (CTEPH) need to be done, comparing USAT with systemic thrombolysis and surgical thombectomy.
Take-home: In patients with submassive PE, USAT should be considered over systemic thombolysis or anti-coagulation alone.
1. PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med. 2014 Apr 10;370(15):1402-11.
2. Engelhardt TC, Taylor AJ, et al. Catheter-directed ultrasound-accelerated thrombolysis for the treatment of acute pulmonary embolism. Thromb Res. 2011 Aug;128(2):149-54
3. Bagla S, Smirniotopoulos JB, et al. Ultrasound-accelerated catheter-directed thrombolysis for acute submassive pulmonary embolism. J Vasc Interv Radiol. 2015 Jul;26(7):1001-6.
4. SEATTLE II Investigators. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism: The SEATTLE II Study. JACC Cardiovasc Interv. 2015 Aug 24;8(10):1382-92.
5. Kucher N, Boekstegers P,et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014 Jan 28;129(4):479-86.
Category: Critical Care
Keywords: Critical care, Trauma, TBI, ICP, hypothermia (PubMed Search)
Posted: 12/22/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
The EuroTherm3235 Trial was a randomized, multi-center trial to study hypothermia (32-35oC) in severe, traumatic brain injury1:
1. Andrews PJ, Sinclair HL, et al; Eurotherm3235 Trial Collaborators. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. N Engl J Med. 2015 Dec 17;373(25):2403-12. doi: 10.1056/NEJMoa1507581. Epub 2015 Oct 7. PubMed PMID: 26444221.
2. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24 Suppl 1:S1-106. PubMed PMID: 17511534.
Category: Critical Care
Keywords: COPD, respiratory failure, antibiotics, ICU (PubMed Search)
Posted: 11/24/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
--The role of antibiotics in acute exacerbations of COPD remains controversial in many settings. However, a recent Cochrane review concludes that antibiotics have "large and consistent" benefit in ICU admissions [1]:
--However, patients on antibiotics had increased side effects, are at risk for increased drug-drug interaction (think azithromycin/levofloxacin), and the effect on multi-drug resistance is unclear.
--GOLD Guidelines are a bit more liberal with their recommendations for antibiotics [2], recommending antibiotics based on symptoms or in patients needing mechanical support.
--TAKEAWAY -- if your patient needs BiPAP or ICU, they should also get antibiotics!
1. Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012 Dec 12;12:CD010257. doi: 10.1002/14651858.CD010257. Review. PubMed PMID: 23235687
2. http://www.goldcopd.org/uploads/users/files/GOLD_Pocket_2015_Feb18.pdf
Category: Critical Care
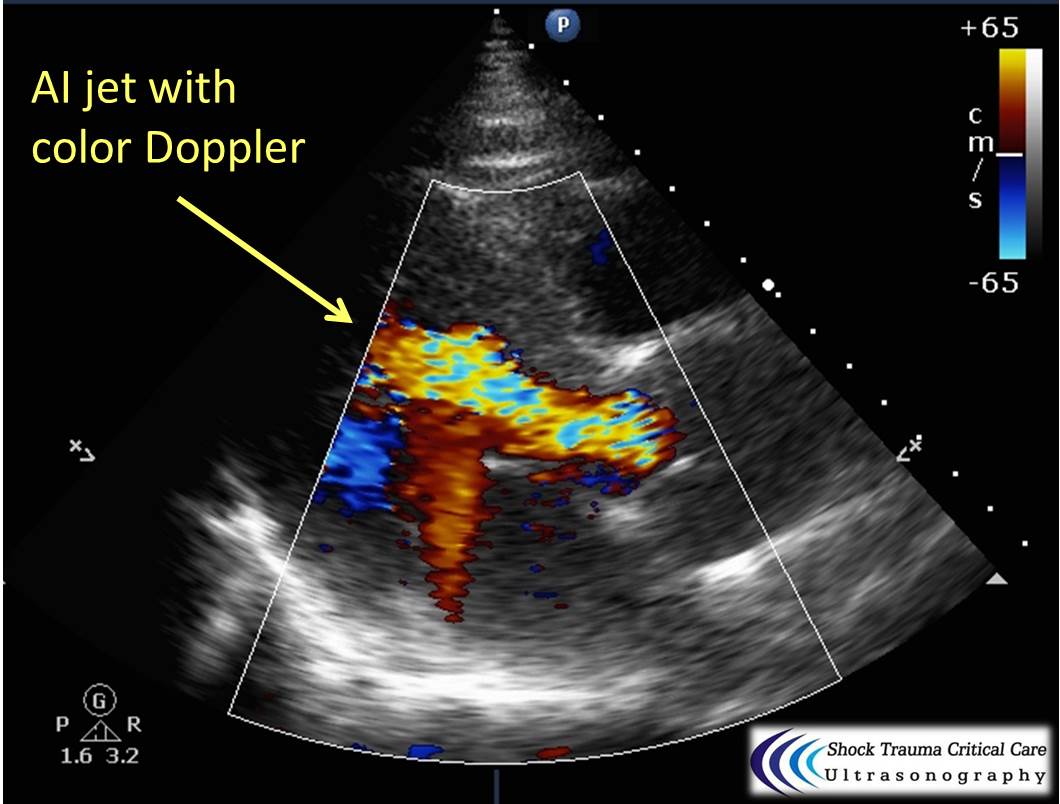
Keywords: Aortic dissection, STEMI, cardiac tamponade, aortic insufficiency, echocardiography (PubMed Search)
Posted: 9/30/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Classically, aortic dissection presents as tearing or ripping chest pain that radiates to the back in a HYPERtensive patient.
However, type A aortic dissections can quickly become HYPOtensive due to any the primary cardiac complications from retrograde dissection into:
Bedside echo can't rule out aortic dissection, but it can help rule in the diagnosis (figure 1) or complications (figure 2) at times.
Category: Critical Care
Keywords: Paracentesis, cirrhosis, ascites, critical care (PubMed Search)
Posted: 9/1/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Your ESLD patient is hypotensive with a tense abdomen, and he needs a paracentesis!
--ALWAYS use ultrasound to localize a fluid pocket [Fig 1]! Take the time to use color Doppler to look for underlying abdominal wall varices [Fig 2]. Cirrhotic patients frequently have abnormal abdominal wall vasculature [1-2].
--Hemorrhage from paracentesis is exceedingly rare, and reversal of mild coagulopathy probably isn't that important [3-4].
--In hypotensive patients, consider placement of a small pigtail catheter for slow, continuous drainage (e.g. 8.3F pericardiocentesis catheter) instead of large-volume paracentesis. Non-tunneled catheter infection risk goes up after 72h [5].
--Albumin replacement improves mortality and incidence of renal failure in patients with SBP or other infection [6-7].
1. Hatch N, Wu TS, Barr L, Roque PJ. Advanced ultrasound procedures. Crit Care Clin. 2014 Apr;30(2):305-29, vi. doi: 10.1016/j.ccc.2013.10.005. Epub 2013 Dec 4. Review. PubMed PMID: 24606778.
2. Thomsen TW, Shaffer RW, White B, Setnik GS. Videos in clinical medicine. Paracentesis. N Engl J Med. 2006 Nov 9;355(19):e21. Erratum in: N Engl J Med. 2007 Feb 15;356(7):760. PubMed PMID: 17093242.
3. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005 Mar 1;21(5):525-9. PubMed PMID: 15740535.
4. McVay PA, Toy PT. Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities. Transfusion. 1991 Feb;31(2):164-71. PubMed PMID: 1996485.
5. Nadir A, Van Thiel DH. Frequency of peritoneal infections among patients undergoing continuous paracentesis with an indwelling catheter. J Ayub Med Coll Abbottabad. 2010 Jan-Mar;22(1):37-41.
6. Kwok CS, Krupa L, Mahtani A, Kaye D, Rushbrook SM, Phillips MG, Gelson W. Albumin reduces paracentesis-induced circulatory dysfunction and reduces death and renal impairment among patients with cirrhosis and infection: a systematic review and meta-analysis. Biomed Res Int. 2013;2013:295153. doi: 10.1155/2013/295153. Epub 2013 Oct 8. Review. PubMed PMID: 24222902; PubMed Central PMCID: PMC3816020.
7. Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, Ruiz-del-Arbol L, Castells L, Vargas V, Soriano G, Guevara M, Gin s P, Rod s J. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999 Aug 5;341(6):403-9. PubMed PMID: 10432325.
Category: Critical Care
Keywords: Anion gap, acidosis, metabolic acidosis, ingestion, critical care (PubMed Search)
Posted: 8/4/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Ever forget all the things that make up MUDPILES in your AG acidosis differential?
Instead, consider the less-complicated mnemonic "KILR"!
K Ketoacidosis (diabetic, alcoholic, starvation)
I Ingestion (salicylate, acetaminophen, methanol, ethylene glycol, CO, CN, iron, INH)
L Lactic acidosis (infection, hemorrhage, hypoperfusion, alcohol, metformin)
R Renal (uremia)
Once you rule out the KLR causes, begin to consider ingestion or a tox source as your source. Remember that many of the listed ingestions can also cause a lactic acidosis.
For more acid/base pearls in greater detail:
http://lifeinthefastlane.com/ccc/anion-gap/
http://emcrit.org/wp-content/uploads/acid_base_sheet_2-2011.pdf (from emcrit.org)
