Category: Critical Care
Keywords: VExUS, IVC, POCUS, Venous Congestion (PubMed Search)
Posted: 12/10/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
The Venous Excess Ultrasound (VExUS) exam integrates IVC, portal, hepatic, and renal vein findings to assess venous congestion and guide management, such as diuresis, in critically ill patients.
Technique:
Tips:
Interpretation:
Sometimes when other clinical information is contradictory, having the extra data point of the VExUS exam can be extremely useful to determine the best plan for a patient. Practice looking for the portal/hepatic veins and getting the waveforms on patients with a CLEAR clinical picture of venous congestion, then practice on more difficult cases.
Assavapokee, T., Rola, P., Assavapokee, N. et al. Decoding VExUS: a practical guide for excelling in point-of-care ultrasound assessment of venous congestion. Ultrasound J 16, 48 (2024). https://doi.org/10.1186/s13089-024-00396-z
Category: Critical Care
Keywords: Subclavian CVC (PubMed Search)
Posted: 12/2/2024 by Jordan Parker, MD
(Updated: 12/3/2024)
Click here to contact Jordan Parker, MD
Background:
Ultrasound-guided subclavian central venous catheter (CVC) placement has become a preferred site due to low risk of infection and a low risk of complication. Complications include arterial puncture, pneumothorax, chylothorax, and malposition of the catheter. Ultrasound guidance can significantly reduce the risk of these complications aside from catheter malposition. The most common sites of malposition are in the ipsilateral internal jugular vein or the contralateral brachiocephalic vein. This study sought to evaluate the rate of catheter malposition between left-and right-sided subclavian vein catheter placement using ultrasound guidance with an infraclavicular approach.
Study:
Results:
Take Home:
For infraclavicular ultrasound-guided subclavian CVC placement, consider using the left-side over the right if no contraindications for left-sided access exist.
The authors proposed anatomical differences in the subclavian veins as the etiology for the difference in malposition rates. Images are provided in the paper. Patient positioning may also play a role which the authors commented on and other clinicians have responded to the article with their thoughts.
Supraclavicular subclavian vein access is also discussed as an alternative option that can provide real-time tracking of the guidewire into the correct location to reduce malposition rates.
Read More below.
Supraclavicular approach and response to the article:
Kander, Thomas MD, PhD1,2; Adrian, Maria MD, PhD1,3; Borgquist, Ola MD, PhD1,3. Right Subclavian Venous Catheterization: Don’t Throw the Baby Out With the Bathwater. Critical Care Medicine 52(12):p e645-e646, December 2024. | DOI: 10.1097/CCM.0000000000006388
Adrian M, Kander T, Lundén R, Borgquist O. The right supraclavicular fossa ultrasound view for correct catheter tip positioning in right subclavian vein catheterisation: a prospective observational study. Anaesthesia. 2022 Jan;77(1):66-72. doi: 10.1111/anae.15534. Epub 2021 Jul 14. PMID: 34260061.
Patient position discussion:
Tokumine, Joho MD, PhD; Moriyama, Kiyoshi MD, PhD; Yorozu, Tomoko MD, PhD. Influence of Arm Abduction on Ipsilateral Internal Jugular Vein Misplacement During Ultrasound-Guided Subclavian Venous Catheterization. Critical Care Medicine 52(12):p e646-e647, December 2024. | DOI: 10.1097/CCM.0000000000006410
Shin KW, Park S, Jo WY, Choi S, Kim YJ, Park HP, Oh H. Comparison of Catheter Malposition Between Left and Right Ultrasound-Guided Infraclavicular Subclavian Venous Catheterizations: A Randomized Controlled Trial. Critical Care Medicine. 2024 Oct 1;52(10):1557-1566. doi: 10.1097/CCM.0000000000006368. Epub 2024 Jun 24. PMID: 38912886.
Category: Critical Care
Keywords: ketamine, etomidate, rapid sequence intubation, hemodynamic instability, adrenal suppression (PubMed Search)
Posted: 11/26/2024 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
It’s the age-old question. We’ve read studies comparing propofol vs. etomidate, ketofol vs. etomidate, and now a meta-analysis about ketamine vs. etomidate. Etomidate is the staple induction agent for RSI, mostly used by Emergency Medicine, and to a degree in the Intensive Care Unit. However, the question about adrenal suppression was initiated in the early 2000s and researchers have been looking for other alternatives. This meta analysis attempted to look for another answer.
Settings: A meta-analysis of randomized controlled trials
Participants: 2384 patients who needed emergent intubation were included.
Outcome measurement: Peri-intubation instability
Study Results:
Compared with etomidate, ketamine was associated with higher risk of hemodynamic instability and moderate certainty (RR 1.29, 95% CI 1.07-1.57).
Ketamine was associated with lower risk of adrenal suppression, again, with moderate uncertainty (RR 0.54, 95% CI 0.45-0.66).
Ketamine was not associated with differences and risk of first successful intubation nor mortality.
Discussion:
Most studies were single center and involved small-moderate sample size, ranging from 20 patients to 700 patients.
For adrenal suppression, there were only 3 studies and a total of 1280 patients, thus, the results are still not definitive.
For an academic exercise, the Number Needed to Harm for both hemodynamic instability and adrenal suppression are calculated here.
Number Needed to Harm for hemodynamic instability: 25.
Number needed to harm for adrendal suppression: 11.
Greer A, Hewitt M, Khazaneh PT, Ergan B, Burry L, Semler MW, Rochwerg B, Sharif S. Ketamine Versus Etomidate for Rapid Sequence Intubation: A Systematic Review and Meta-Analysis of Randomized Trials
Category: Critical Care
Keywords: cardiac arrest, ACLS, IV access (PubMed Search)
Posted: 11/5/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
In out of hospital cardiac arrest (OHCA), does it matter if you choose an intraosseous (IO) vs intravenous (IV) approach to getting access and giving meds?
No, according to a recent study by Couper et al, just published in NEJM. No significant difference in any clinically meaningful outcome including survival, neurologically intact discharge, etc. Technically the IV group had slightly higher rates of ROSC, which just met statistical significance, and to be fair that group did trend very slightly towards better outcomes in some categories, but really well within the range expected by statistical noise.
Interestingly, the median time from EMS arrival to access being established was the same in both groups (12 minutes), which I think raises some face validity questions. Furthermore, of course, previous trials have raised questions as to whether ACLS meds even work or impact outcomes anyways, so naturally if they don't, the method by which they are given isn't likely to matter either.
Bottom Line: This large, well conducted trial continues to support the notion that either an IV-focused, or IO-focused approach to access and medication delivery in OHCA is reasonable. You and your prehospital colleagues can likely continue to make this decision based on personal comfort, local protocols, and patient/case circumstances. At the very least, this continues to support the notion that if an IV is proving challenging, pursuing an IO instead is a very appropriate thing to do.
Couper K, Ji C, Deakin CD, Fothergill RT, Nolan JP, Long JB, Mason JM, Michelet F, Norman C, Nwankwo H, Quinn T, Slowther AM, Smyth MA, Starr KR, Walker A, Wood S, Bell S, Bradley G, Brown M, Brown S, Burrow E, Charlton K, Claxton Dip A, Dra'gon V, Evans C, Falloon J, Foster T, Kearney J, Lang N, Limmer M, Mellett-Smith A, Miller J, Mills C, Osborne R, Rees N, Spaight RES, Squires GL, Tibbetts B, Waddington M, Whitley GA, Wiles JV, Williams J, Wiltshire S, Wright A, Lall R, Perkins GD; PARAMEDIC-3 Collaborators. A Randomized Trial of Drug Route in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2024 Oct 31:10.1056/NEJMoa2407780. doi: 10.1056/NEJMoa2407780. Epub ahead of print. PMID: 39480216; PMCID: PMC7616768.
Category: Critical Care
Posted: 10/22/2024 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Intravascular Volume and the IVC
Rola P, Haycock K, Spiegel R. What every intensivist should know about the IVC. J Crit Care. 2024; 80:154455.
Category: Critical Care
Keywords: vascular access, micropuncture kits, procedures (PubMed Search)
Posted: 10/15/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Getting reliable venous and arterial access is crucial when resuscitating critically ill patients. These lines can be difficult due to patient and situation specific variables.
Micropuncture kits contain a 21-gauge echogenic needle, a stainless-steel hard shaft/soft-tip wire, and a 4 Fr or 5 Fr sheath and introducer. The micropuncture kit offers several advantages that can help overcome difficult situations:
To use a micropuncture kit, gain vessel access with the needle and wire, railroad the sheath and introducer into the vessel, remove the wire, then remove the introducer. Now you have a 4 Fr or 5 Fr sheath in the vessel. This is typically used to introduce a normal central line wire.
For arterial lines, you can place them directly over the wire without dilation. Keep in mind that the 4 Fr sheath (1.3 mm OD) and 5 Fr sheath (1.7 mm OD) are larger than a typical arterial line catheter (18g = 1.27 mm OD). If you dilate then you will cause hematoma.
Find out where your department stores micropuncture kits and get familiar with their components. While it adds an extra step to the procedure, it could make the difference between securing the line or not.
Montrief, T., Ramzy, M., & Long, B. (2021). Micropuncture kits for difficult vascular access. The American journal of emergency medicine.
Category: Critical Care
Keywords: Septic Shock, Vitamin B12, Hydroxocobalamin, sepsis (PubMed Search)
Posted: 10/8/2024 by Jordan Parker, MD
Click here to contact Jordan Parker, MD
Background:
Septic shock is a severe and common critical illness that is managed in the emergency department. Our current foundation of treatment includes IV fluids, empiric antibiotic coverage, vasopressor therapy, source control and corticosteroids for refractory shock. The levels of nitric oxide (NO) and hydrogen sulfide (H2S) are elevated in sepsis and associated with worse outcomes. Hydroxocobalamin is an inhibitor of NO activity and production and a scavenger of H2S [1,2]. Most of the current data is limited to observational studies looking at hydroxocobalamin in cardiac surgery related vasodilatory shock with few case series and reports for use in septic shock. The available data has shown an improvement in hemodynamics and reduction in vasopressor requirements in various vasodilatory shock states [2]. Chromaturia and self-limited red skin discoloration are common side effects but current data has not shown significant adverse events [3,4]. Patel et al, performed a phase 2 single-center trial to evaluate use of high dose IV hydroxocobalamin in patients with septic shock.
Study:
Results
Take home
There is a low risk of serious adverse events from high dose hydroxocobalamin use [3,4]. For now, it may be reasonable to consider in cases of septic shock refractory to standard care but there isn’t enough data to support its regular use yet.
Category: Critical Care
Keywords: albumin, crystalloid, septic shock, mortality (PubMed Search)
Posted: 10/1/2024 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Title: Albumin Versus Balanced Crystalloid for the Early Resuscitation of Sepsis: An Open Parallel-Group Randomized Feasibility Trial— The ABC-Sepsis Trial
Settings: 15 ED in the United Kingdom. This study is a feasibility study but it looked at mortality as a primary outcome.
Participants:
• Patients with Sepsis, with their National Early Warning Score (NEWS) ? 5 (These patients have estimated mortality of 20%). IV fluid resuscitation needs to be within 1 hour of assessment.
• 300 Patients were randomized to receive balanced crystalloids or 5% human albumin solution (HAS) only, within 6 hours of randomization.
Outcome measurement: 30-day mortality, Hospital length of stay (HLOS)
Study Results:
• The median time for receiving IV fluid from randomization was 41 minutes (HAS) vs. 36 minutes (crystalloids).
• Total volume of IV fluid per Kg in first 6 hours 14.5 ml/kg (HAS) vs. 18.8 ml/kg (crystalloids).
• Other interventions (vasopressor, Renal replacement therapy, invasive ventilation) were similar.
• Complications (AKI, pulmonary edema, allergy) were lower for Crystalloids group
• Median hospital LOS = 6 days for both groups.
• 90-day mortality: 31 (21.1%) (HAS) vs. 22 (14.8%) (Crystalloids), OR 1.54 (95% 0.8-2.8)
Discussion:
• Total volumes for resuscitation in the first 6 hours was 750 ml (HAS) and 1250 ml (crystalloids). This signified a trend toward lower total volume of resuscitation (remember that 30 ml/kg recommendation)
• The 2024 guidelines from Chest (REF 2) suggested that: “In Critically ill adult patients (excluding patients with thermal injuries and ARDS), intravenous albumin is not suggested for first line volume replacement or to increase serum albumin levels. Therefore, we should not give patients (except for cirrhosis or spontaneous bacterial peritonitis) albumin just to reduce the volume of fluid.
• The authors suggested that even a definitive trial in the future will not be able to demonstrate a significant benefit of using 5% albumin.
Conclusion:
There is lower mortality (numerical but not statistically) among the group with balanced crystalloids.
1. Gray AJ, Oatey K, Grahamslaw J, Irvine S, Cafferkey J, Kennel T, Norrie J, Walsh T, Lone N, Horner D, Appelboam A, Hall P, Skipworth RJE, Bell D, Rooney K, Shankar-Hari M, Corfield AR; Albumin, Balanced, and Crystalloid-Sepsis (ABC-Sepsis) Investigators. Albumin Versus Balanced Crystalloid for the Early Resuscitation of Sepsis: An Open Parallel-Group Randomized Feasibility Trial- The ABC-Sepsis Trial. Crit Care Med. 2024 Oct 1;52(10):1520-1532. doi: 10.1097/CCM.0000000000006348. Epub 2024 Jun 24. PMID: 38912884.
2. Callum J, Skubas NJ, Bathla A, Keshavarz H, Clark EG, Rochwerg B, Fergusson D, Arbous S, Bauer SR, China L, Fung M, Jug R, Neill M, Paine C, Pavenski K, Shah PS, Robinson S, Shan H, Szczepiorkowski ZM, Thevenot T, Wu B, Stanworth S, Shehata N; International Collaboration for Transfusion Medicine Guidelines Intravenous Albumin Guideline Group. Use of Intravenous Albumin: A Guideline From the International Collaboration for Transfusion Medicine Guidelines. Chest. 2024 Aug;166(2):321-338. doi: 10.1016/j.chest.2024.02.049. Epub 2024 Mar 4. PMID: 38447639; PMCID: PMC11317816.
Category: Critical Care
Posted: 9/24/2024 by Caleb Chan, MD
(Updated: 2/1/2026)
Click here to contact Caleb Chan, MD
Some points from this narrative review:
Take home pearls:
van Eijk JA, Doeleman LC, Loer SA, Koster RW, van Schuppen H, Schober P. Ventilation during cardiopulmonary resuscitation: A narrative review. Resuscitation. 2024;203:110366.
Category: Critical Care
Posted: 9/17/2024 by William Teeter, MD
Click here to contact William Teeter, MD
I wanted to send out two websites curated in part by UMEM current and past faculty/residents/fellows which have a wealth of critical care lectures and resources:
Disclosure: *I am one of the webmasters for the STCMTCC, but have no affiliation with MCCP other than as an enthusiastic reader.
Category: Critical Care
Keywords: RSI, intubation, critical care, out of hospital cardiac arrest (PubMed Search)
Posted: 9/10/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Airway management in the pre-hospital setting is a matter of much controversy, and overall I will defer to my EMS colleagues, but several previous studies have failed to show a benefit to endotracheal intubation in the field as opposed to alternate approaches like a supraglottic airway. Another nod in this direction has recently come out, with Battaglini et al performing a post-hoc analysis of one of the larger studies in the history of cardiac arrest, TTM-2, looking specifically at outcomes stratified by pre-hospital airway management strategy.
Do patients who undergo endotracheal intubation in the field do better than those who get a supraglottic airway?
No, they don't. TTM-2 included 1900 patients, of whom 1702 had enough data to be included in this re-analysis. 28% got supraglottic airways, and 72% got endotracheal intubation. The groups were reasonably well matched on most characteristics, and if anything most well-known prognostic factors favored the endotracheal intubation group (very slightly). It should be noted that several outcome metrics, including modified Rankin scale, did show slight signs of benefit for the endotracheal intubation group, even sometimes in a statistically significant fashion, but fell out when a multi-regression analysis, which was the primary endpoint, was done.
Bottom Line: In pre-hospital cardiac arrest, there remains limited data to support the notion that endotracheal intubation results in better outcomes than supraglottic airway placement. You should defer to your local protocols and continue to work with your paramedics and EMS directors as evidence continues to evolve. For now, I don't think there's sufficient data to suggest that a given patient should be intubated vs undergoing supraglottic airway placement, and it is probably best to defer to the judgement, training, and protocols of your folks on scene.
Battaglini D, Schiavetti I, Ball L, Christian Jakobsen J, Lilja G, Friberg H, David Wendel-Garcia P, Young PJ, Eastwood G, Chew MS, Unden J, Thomas M, Joannidis M, Nichol A, Lundin A, Hollenberg J, Hammond N, Saxena M, Martin A, Solar M, Silvio Taccone F, Dankiewicz J, Nielsen N, Morten Grejs A, Wise MP, Hängghi M, Smid O, Patroniti N, Robba C; TTM2 trial investigators§. Association between Early Airway Intervention in the Pre-Hospital setting and Outcomes in Out of Hospital Cardiac Arrest Patients: a post-hoc analysis of the Target Temperature Management-2 (TTM2) trial. Resuscitation. 2024 Sep 5:110390. doi: 10.1016/j.resuscitation.2024.110390. Epub ahead of print. PMID: 39244144.
Category: Critical Care
Keywords: OHCA, opioid, opiates, fentanyl, overdose, cardiac arrest (PubMed Search)
Posted: 9/2/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
The incidence of opioid-overdose-related deaths has clearly increased in the past decade, with recent estimates of up to 17% of OHCA being opioid-related in 2023. [1,2] The use of naloxone for opiate reversal in overdose is well-established, with reasonable inference but no formal proof that its use could help in opioid-associated out of hospital cardiac arrest (OA-OHCA). [3] The August publication of two trials [4,5] retrospectively examining naloxone administration in OHCA offers some perspectives…
and
[View “Visual Diagnosis” for slightly more detail on the referenced studies.]
Bottom Line: While prospective trials are absolutely needed to offer more definitive evidence regarding the use of empiric naloxone in nontraumatic OHCA, the rising incidence of OA-OHCA in the U.S. and current findings are convincing enough to encourage early naloxone administration, especially in populations with higher incidence of opioid use.
U.S. Mortality due to Opioid Overdose (CDC data)
Dillon et al, JAMA
Strong et al, Resuscitation
Category: Critical Care
Posted: 8/27/2024 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Hepatorenal Syndrome
Nadim M, et al. Hepatorenal syndrome in the intensive care unit. Intensive Care Med. 2024; 50:978-981.
Category: Critical Care
Keywords: Euglycemic DKA (PubMed Search)
Posted: 8/20/2024 by Cody Couperus-Mashewske, MD
Click here to contact Cody Couperus-Mashewske, MD
Euglycemic DKA (eDKA) is a medical emergency requiring prompt attention. It is caused by an imbalance of insulin and glucagon leading to ketone accumulation (1-3). In addition to typical risk factors for DKA, those for eDKA include SGLT-2 inhibitor use and pregnancy, with 30% of DKA cases in pregnancy presenting euglycemic (4, 5).
eDKA presents with an anion gap metabolic acidosis, ketosis/ketonuria, & blood glucose less than 250 mg/dL.
Diagnosis requires ruling out other causes of anion gap metabolic acidosis, including toxic ingestions.
The cornerstone of eDKA management is ensuring enough dextrose to allow needed insulin administration to reverse ketone accumulation.
1. McCabe, D. E., Strollo, B. P. & Fuhrman, G. M. Euglycemic Diabetic Ketoacidosis in the Surgical Patient. Am. Surg. 89, 1083–1086 (2023).
2. Chaudhry, A., Roels, C. & Lee, J. Sodium–Glucose Cotransporter-2 Inhibitor–associated Euglycemic Diabetic Ketoacidosis: Lessons From a Case Series of 4 Patients Undergoing Coronary Artery Bypass Grafting Surgery. Can. J. Diabetes 46, 843–850 (2022).
3. Wan Azman, S. S., Sukor, N., Abu Shamsi, M. Y., Ismail, I. & Kamaruddin, N. A. Case Report: High-Calorie Glucose Infusion and Tight Glycemic Control in Ameliorating Refractory Acidosis of Empagliflozin-Induced Euglycemic Diabetic Ketoacidosis. Front. Endocrinol. 13, 867647 (2022).
4. Jaber, J. F., Standley, M. & Reddy, R. Euglycemic Diabetic Ketoacidosis in Pregnancy: A Case Report and Review of Current Literature. Case Rep. Crit. Care 2019, 1–5 (2019).
5. Algaly, G., Abdelrahman, A. & Ahmed, S. M. I. Euglycemic diabetic ketoacidosis in a pregnant woman. J. Am. Coll. Emerg. Physicians Open 4, e13089 (2023).
6. Dutta, S. et al. Euglycemic diabetic ketoacidosis associated with SGLT2 inhibitors: A systematic review and quantitative analysis. J. Fam. Med. Prim. Care 11, 927 (2022).
7. Koceva, A. & Kravos Tramšek, N. A. From Sweet to Sour: SGLT-2-Inhibitor-Induced Euglycemic Diabetic Ketoacidosis. J. Pers. Med. 14, 665 (2024).
8. Juneja, D., Nasa, P., Jain, R. & Singh, O. Sodium-glucose Cotransporter-2 Inhibitors induced euglycemic diabetic ketoacidosis: A meta summary of case reports. World J. Diabetes 14, 1314–1322 (2023).
9. Albert, S. G., Shrestha, E. & Wood, E. M. Euglycemic diabetic ketoacidosis: The paradox of delayed correction of acidosis. Diabetes Metab. Syndr. Clin. Res. Rev. 17, 102848 (2023).
Category: Critical Care
Keywords: DKA (PubMed Search)
Posted: 8/13/2024 by Jordan Parker, MD
Click here to contact Jordan Parker, MD
Diabetic ketoacidosis (DKA) is a serious condition that carries the risk of significant morbidity and mortality if not managed appropriately. Typically managed with an infusion of regular insulin, IV fluids, and electrolytes, there is evidence to support treatment of mild to moderate DKA with a subcutaneous (SQ) regimen using a combo of fast-acting and long-acting insulin instead, decreasing the need for ICU admission without increasing adverse events [1].
What patients?
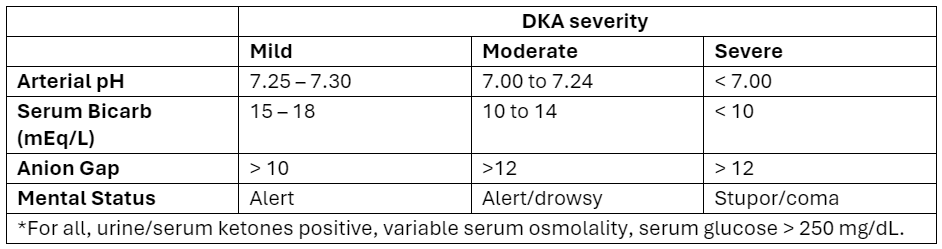
Adapted from Abbas et al.
How to manage?
Initial dose
Subsequent dosing:
If serum glucose is > 250 mg/dL
If serum glucose is < 250 mg/dL
Bottom Line
DKA management with a SQ insulin protocol is a reasonable approach for patients with mild to moderate DKA, is supported by the American Diabetes Association [5], and can be particularly helpful in this era of ED boarding and bed shortages. Give a long-acting insulin dose every 24 hours (or restart the patient’s home long-acting regimen) and short-acting insulin every 2 to 4 hours. Aggressive IV fluid resuscitation, electrolyte repletion, and treatment of underlying precipitating cause remain additional cornerstones of DKA management.
Category: Critical Care
Keywords: meropenem, continuous administration, critically ill (PubMed Search)
Posted: 8/6/2024 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
We heard it before. Continuous administration of antibiotics might be associated with better outcomes. However, results from smaller randomized controlled trials of beta-lactam showed inconsistent conclusions. Therefore, a large RCT was conducted
Settings: 31 ICUs in Croatia, Italy, Kazakhstan, Russia between June 2018 – August 2022.
Randomized, double-blind control trial.
Participants:
Outcome measurement:
Study Results:
Discussion:
Conclusion:
In critically ill patients with sepsis, continuous administration of meropenem did not improve mortality nor reduce the emergence of pandrug resistant bacteria.
Monti G, Bradic N, Marzaroli M, Konkayev A, Fominskiy E, Kotani Y, Likhvantsev VV, Momesso E, Nogtev P, Lobreglio R, Redkin I, Toffoletto F, Bruni A, Baiardo Redaelli M, D'Andrea N, Paternoster G, Scandroglio AM, Gallicchio F, Ballestra M, Calabrò MG, Cotoia A, Perone R, Cuffaro R, Montrucchio G, Pota V, Ananiadou S, Lembo R, Musu M, Rauch S, Galbiati C, Pinelli F, Pasin L, Guarracino F, Santarpino G, Agrò FE, Bove T, Corradi F, Forfori F, Longhini F, Cecconi M, Landoni G, Bellomo R, Zangrillo A; MERCY Investigators. Continuous vs Intermittent Meropenem Administration in Critically Ill Patients With Sepsis: The MERCY Randomized Clinical Trial. JAMA. 2023 Jul 11;330(2):141-151. doi: 10.1001/jama.2023.10598. PMID: 37326473; PMCID: PMC10276329.
Category: Critical Care
Posted: 7/23/2024 by William Teeter, MD
(Updated: 2/1/2026)
Click here to contact William Teeter, MD
Do Sepsis Alert Systems Work?
Researchers in Korea completed a high quality systematic review and meta-analysis of sepsis alert systems for adult ED patients
Using high quality methods, they identified over 3000 studies with 22 meeting criteria.
They found these systems were associated with:
Electronic alerts were further associated with:
Summary (+ a little editorialization)
As annoying as we may find these systems in our daily practice, there is growing evidence that they do provide some benefit with impacts on task saturation and decreasing cognitive load in addition to real patient benefit. While there is also recent evidence that physician gestalt performs well against these systems, there is a suggested benefit in their inclusion in clinical decision making as a safety net or as an “assist”.
The incorporation of rule-based algorithms like these in more advance machine learning methods are covered quite well in a recent opinion piece on “The AI Future of Emergency Medicine”. However, it is important to always know the source of any “algorithm” that you are using, whether rule or mathematically based, given real concerns for bias and error.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821277
https://www.sciencedirect.com/science/article/pii/S019606442400043X
https://www.sciencedirect.com/science/article/abs/pii/S0196064424000994
Category: Critical Care
Posted: 7/16/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
The CLOVERS trial (NEJM 2023) examined one of the eternal questions of critical care, liberal vs restrictive fluid management in sepsis… and found no difference. But there are criticism of CLOVERS, and while some other trials agreed with this result, there are also signals in the literature that restrictive fluid strategies are beneficial. Furthermore, we know that these trials suffer from issues of heterogeneity, and often lump together very different patients.
Jorda et al recently published in Critical Care a posthoc re-analysis of CLOVERS looking specifically at patients with advanced CKD (eGFR < 30). This is a challenging group of patients to manage. On the one hand their renal function is already marginal, so the last thing we want to do is potentially deprive starved kidneys of necessary intravascular volume, but on the flip side their septic shock puts them at high risk of full blown renal failure (transient or permanent) and they're thus at very high risk of fluid overload with aggressive resuscitative fluids and potentially limited ability to clear those fluids renally in the next few days. So how did these patients do in CLOVERS?
They did significantly better with the restrictive fluid strategy (mortality 22% vs 39%, HR CI 0.29-0.85). They also had more pressor free days and vent free days.
Bottom Line (my opinion): While a restrictive vs liberal fluid strategy in septic shock remains a bit up for debate, the evidence continues to slowly tip towards restrictive fluids (i.e. earlier pressors) as the preferred approach. In patients with advanced CKD (eGFR < 30), there is probably now sufficient evidence to favor vasopressors over IV fluid administration when resuscitating septic shock.
Jorda A, Douglas IS, Staudinger T, Heinz G, Bergmann F, Oberbauer R, Sengölge G, Zeitlinger M, Jilma B, Shapiro NI, Gelbenegger G. Fluid management for sepsis-induced hypotension in patients with advanced chronic kidney disease: a secondary analysis of the CLOVERS trial. Crit Care. 2024 Jul 11;28(1):231. doi: 10.1186/s13054-024-05019-6. PMID: 38992663; PMCID: PMC11238412.
National Heart, Lung, and Blood Institute Prevention and Early Treatment of Acute Lung Injury Clinical Trials Network; Shapiro NI, Douglas IS, Brower RG, Brown SM, Exline MC, Ginde AA, Gong MN, Grissom CK, Hayden D, Hough CL, Huang W, Iwashyna TJ, Jones AE, Khan A, Lai P, Liu KD, Miller CD, Oldmixon K, Park PK, Rice TW, Ringwood N, Semler MW, Steingrub JS, Talmor D, Thompson BT, Yealy DM, Self WH. Early Restrictive or Liberal Fluid Management for Sepsis-Induced Hypotension. N Engl J Med. 2023 Feb 9;388(6):499-510. doi: 10.1056/NEJMoa2212663. Epub 2023 Jan 21. PMID: 36688507; PMCID: PMC10685906.
Category: Critical Care
Keywords: Corticosteroids, septic shock, ARDS, acute respiratory distress syndrome, community acquired pneumonia, CAP, dexamethasone, methylprednisolone, hydrocortisone (PubMed Search)
Posted: 7/9/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
This May, the Society of Critical Care Medicine (SCCM) published new recommendations [1] for the use of corticosteroids in critical illness (separate from patients with known adrenal insufficiency or on chronic steroids), namely:
Bottom Line:
For severe bacterial pneumonia and septic shock, ED physicians should feel comfortable administering a dose of hydrocortisone 50mg IV as hydrocortisone 200mg/day is an accepted regimen for these disease processes.
For patients with ARDS who remain boarding in the ED, EM docs should discuss initiation of steroids with their intensivists, whether the institutional preference is for dexamethasone 20mg IV (per DEXA-ARDS) [6] or methylprednisolone 1mg/kg/day (per Meduri)[7].
Category: Critical Care
Posted: 7/2/2024 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Noninvasive Ventilation for Preoxygenation
Gibbs KW, Semler MW, Driver BE, et al. Noninvasive ventilation for preoxygenation during emergency intubation. N Engl J Med. 2024; 390:2165-77.
