Category: Neurology
Keywords: MS, steroids, MRI (PubMed Search)
Posted: 6/23/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Multiple sclerosis (MS) relapses are defined as new or worsening neurologic deficits lasting 24 hours or more in the absence of fever or infection. Symptoms may be visual, motor, sensory, balance or cognitive. It is a clinical diagnosis, but the presence of a new gadolinium-enhancing lesion on MRI can be used as a radiologic marker of an MS relapse. However, it is unclear whether asymptomatic lesions should be treated, making it prudent to rely on the clinical evaluation rather than the MRI for diagnosis.
Moderate to severe relapses should be treated within 1 week of onset. The mainstay of treatment for relapses is IV methylprednisolone, usually dosed at 500mg to 1g per day for 3-7 days.
Similar symptoms occurring in the presence of fever, heat exposure, stress or infection (such as urinary or upper respiratory tract infections) are "pseudoexacerbations", and should not be treated as an MS relapse.
Berkovich RR. Acute Multiple Sclerosis Relapse. Continuum 2016;22(3):799 814.
Category: Neurology
Keywords: PATCH, ICB, Platelets (PubMed Search)
Posted: 6/19/2016 by Michael Bond, MD
Click here to contact Michael Bond, MD
The PATCH trail, recently published in the Lancet, looked at whether giving platelets to patients, that were on anti-platelet therapy (e.g.: aspirin, clopedrigrel, or dipyridamole) for at least 7 days at the time of their spontaneous intracerebral hemorrhage, improved neurologic outcomes and mortality.
This was a large (60 hospitals) multicener, open-label, masked endpoint, randomized trial that enrolled a total of 190 patients (97 platelet transfusion and 93 standard care).
The outcomes were surprising. Patient in the Platelet group had a higher rat of death or dependence at 3 months (Adjusted OR 2.05; 95% CI 1.18 3.56; p = 0.0114).
The authors concluded "Platelet transfusion seems inferior to standard care for people taking anti-platelet therapy before a spontaneous intracerebral hemorrhage"
Though this is the first study to look at this, the studies design and outcomes should really make use reconsider whether we give these patients platelets. The thought is that ICB or hemorrhagic strokes also have a component of ischemic stroke and a watershed area that's blood flow becomes compromised with the platelet transfusion.
TAKE HOME POINT: We should not routinely transfuse platelets in our patients that were on antiplatelet therapy prior to their ICB.
Baharoglu MI et al. Platelet Transfusion Versus Standard Care After Acute Stroke due to Spontaneous Cerebral Haemorrhage Associated with Antiplatelt Therapy (PATCH): A Randomised, Open-Label, Phase 3 Trial. Lancet 2016; 1 9
Category: Neurology
Keywords: MRA, MRV, non-contrast, contrast-enhanced, gadolinium, time-of-flight, TOF (PubMed Search)
Posted: 6/8/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Gadolinium - To Use or Not Use?
| Non-Contrast MRA/MRV | Contrast-Enhanced MRA/MRV | |
| How Does It Work? | * Time-of-flight (TOF) is a commonly used sequence * Relies on flow of blood into imaging plane * Difference between signal of blood and suppressed background tissue | * Similar to CT angiography/venography * Higher intravascular signal purely from gadolinium-based contrast, not dependent on flow
|
| Pros | * Does not require contrast
| * Generally better image quality * Shorter acquisition time |
| Cons | * Slow, turbulent, or retrograde flow may result in signal loss * Over-estimates stenosis * Longer acquisition time | * RIsks associated with contrast use * Timing of image acquisition important |
| Applications | * Patients with allergy to gadolinium, renal dysfunction, pregnancy * Evaluation of intracranial vessels and cerebral venous system | * Evaluation of stenoses and occlusions of the neck vessels and their origins at the aortic arch
|
Follow me on Twitter @ EM_NCC
Category: Neurology
Keywords: headache, analgesia, cluster, migraine, oxygen (PubMed Search)
Posted: 5/25/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Short Answer: No
Classically, some therapies for headaches are thought to be effective in only certain classifications of headaches, such as triptans in migraines, or oxygen in cluster headaches. This is not necessarily true.
Triptans have been successfully used in cluster headaches, as found in the 2013 Cochrane review.1
More recently, "high-flow" oxygen (referring to 12 L/min of oxygen, delivered through a facemask) has been studied in migraine headaches, with promising results. When compared with placebo (air), oxygen used for 15 minutes was more effective in pain relief and improving visual symptom, with no significant adverse events. 2
1. Law S, Derry S, Moore RA. Triptans for acute cluster headache. Cochrane Database Syst Rev. 2013 Jul 17;7
2. Singhal AB, Maas MB, Goldstein JN, et al. High-flow oxygen therapy for treatment of acute migraine: A randomized crossover trial. Cephalalgia. 2016 May 20.
Category: Neurology
Keywords: magnetic resonance imaging, MRI, T1, T2, FLAIR, DWI, ADC (PubMed Search)
Posted: 5/11/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Want to learn more about how to read a brain MRI? Here are the basics:
Stay tuned for more pearls in this series on brain MRI!
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: seizure, epilepsy, antiepileptic (PubMed Search)
Posted: 4/28/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
A 25 year old patient presents to the emergency department (ED) with a first unprovoked seizure. His ED workup is normal and he is back to his baseline, and you plan to discharge the patient with outpatient follow up within 1 week. The patient is requesting to be discharged on an anti-epileptic drug (AED). What do you do?
Educate the patient about the risk of recurrence, and the possible side effects of AEDs!
The American Academy of Neurology (AAN) specifically addressed this in their 2015 guidelines. A few points to remember:
- The risk of recurrence is greatest within the first 2 years, and occurs in 21-45% of patients.
- The risk of recurrence increases with a remote brain lesion or injury, abnormal EEG, significant brain imaging abnormality or nocturnal seizures.
- AED therapy is likely to reduce the risk of a 2nd unprovoked seizure by about 35% over the next 2 years, but the delay in initiating therapy does not increase the long-term remission risk.
Is it different if the patient had multiple seizures within 24 hours?
Patients presenting with multiple seizures in a 24-hour period were as likely to have seizure recurrence as those presenting with a single seizure, irrespective of etiology or treatment.
Bergey GK. Management of a First Seizure. Continuum 2016;22(1):38 50.
Category: Neurology
Keywords: dizzy, dizzinesss, acute vestibular syndrome, triggered episodic vestibular syndrome, spontaneous episodic vestibular syndrome, HINTS, Dix-Hallpike (PubMed Search)
Posted: 4/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
What Do You Mean By Dizzy?
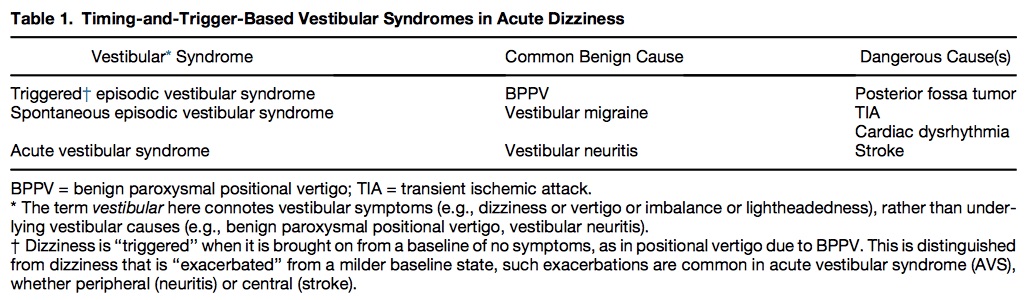
Table 1 shows common benign and serious causes of these vestibular syndromes.
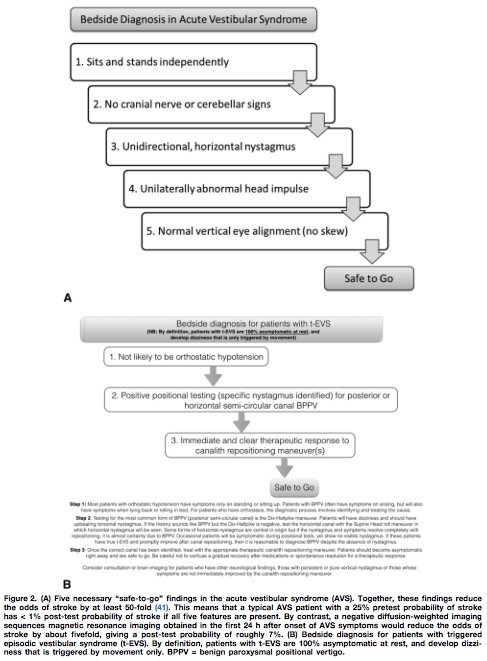
Utilizing the HINTS battery or the Dix-Hallpike maneuver, a “safe to go” algorithm for acute vestibular syndrome and triggered episodic vestibular syndrome is outlined in Figure 2.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: geriatrics, seizures, mimics, TIA, syncope (PubMed Search)
Posted: 3/23/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Carlson C, Anderson CT. Special Issues in Epilepsy: The Elderly, the Immunocompromised, and Bone Health. Continuum 2016;22(1):246 261
Category: Neurology
Keywords: Up-gaze paresis, ophthalmoparesis, hydrocephalus, shunt malfunction (PubMed Search)
Posted: 3/9/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Sunset Eye Sign
Category: Neurology
Keywords: pseudoseizures, EEG, somatoform, psychiatric (PubMed Search)
Posted: 2/24/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Chen DK and LaFrance WC. Diagnosis and Treatment of Nonepileptic Seizures. Continuum 2016;22(1):116 131
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, venography, CTV, MRV (PubMed Search)
Posted: 2/10/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: CT venography is good for diagnosing CVT, but MRI/MRV is superior for detection of isolated cortical venous thromboses and assessing parenchymal damage.
Bonneville F. Imaging of cerebral venous thrombosis. Diagn Interv Imaging. 2014;95:1145-1150.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: airway, intubation, intracranial hemorrhage, ketamine, opiates, RSI (PubMed Search)
Posted: 1/27/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Airway management is an integral part of caring of critically ill patients, but is there anything that should be done differently in the neurologically injured patient?
Bucher J, Koyfman A. Intubation of the Neurologically Injured Patient. JEM 49 (6) 920-7
Category: Neurology
Keywords: Traumatic brain injury, psychiatric disorders, anxiety, depression (PubMed Search)
Posted: 1/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line:
Scholten AC, Haagsma JA, Cnossen MC, et al. Prevalence and risk factors of anxiety and depressive disorders following traumatic brain injury: a systematic review. J Neurotrauma. 2016 Jan 5. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: CSF, LP, HSV, infection (PubMed Search)
Posted: 12/22/2015 by Danya Khoujah, MBBS
(Updated: 1/16/2016)
Click here to contact Danya Khoujah, MBBS
HSV infection of the CNS is one of few treatable viral diseases. HSV encephalitis of older children and adults is almost always caused by herpes simplex virus type 1 (HSV-1), and in individuals older than 20, is due to HSV reactivation.
Temporal lobe localization is characteristic for HSV encephalitis in individuals older than 3 months, and is responsible for its characteristic presentation, namely bizarre behavior and expressive aphasia.
CSF analysis will usually reveal an elevated protein level, and a lymphocytic cellular predominance.
CSF protein concentration is a function of disease duration, and will continue to rise even with administration of treatment (acyclovir) and may remain elevated after the completion of therapy.
5% of CSF samples will be totally normal, and the diagnosis will only be revealed with positive PCR detection of viral DNA in the CSF, which is the gold standard for diagnosis.
The sensitivity of MRI is similar to CSF analysis, with 5% of patients with HSV encephalitis having a normal MRI on presentation, and subsequently developing abnormalities.
Of note, HSV-2 tends to cause aseptic meningitis rather than encephalitis in adults, and has a benign course.
Bottom Line? Keep a high index of suspicion for HSV encephalitis, and treat the patient empirically despite a normal CSF/MRI pending PCR results.
Whitley RJ. Herpes Simplex Virus Infections of the Central Nervous System. Continuum 2015;21(6):1704 13
Category: Neurology
Keywords: Stroke, NIH stroke scale, NIHSS (PubMed Search)
Posted: 12/9/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
A recent study compared the original NIHSS with the shortened 11, 8, and 5 item versions.4
Bottom Line: The original 15-item NIHSS should still be used to evaluate patients’ stroke severity.
The reliability of the NIHSS has been found to improve with personal and videotaped training.
Follow me on Twitter @ EM_NCC
Category: Neurology
Keywords: Seizure, Status Epilepticus, Dissociative Agents (PubMed Search)
Posted: 11/26/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Ketamine has been the drug du jour for everything from agitation to pain, but status epilepticus?
Looking at the pathophysiology of seizures, they occur due to an imbalance between excitatory mechanisms (through glutamate at the NMDA receptors) and inibitory mechanisms (at GABA receptors). The mainstay for seizure treatment has been mostly potentiation of the inhibitory mechanisms, but why not inhibit the excitatory mechanisms at the NMDA receptors?
Ketamine is the only NMDA antagonist that has been investigated for refractory status epilepticus, mostly in retrospective small series, with only 3 prospective cohort studies, totaling to 162 patients (110 adults and 52 pediatrics). Variable results were recorded, from studies with complete response in all patients to complete treatment failure, with a total of 56.5% of the adult patients having electrographic response. The optimal bolus dose appears to be 1.5-4.5 mg/kg, with an infusion of up to 10 mg/kg/hour.
Bottom Line? Consider using ketamine in patients who are in refractory status - after benzodiazepines, a 2nd line agent (such as fosphenytoin, valproic acid or levetiracetam) and IV anesthetics have failed.
(NMDA: N-methyl-D-aspartate, GABA: -aminobutyric acid)
Zeiler FA. Early Use of the NMDA Receptor Antagonist Ketamine in Refractory and Superrefractory Status Epilepticus. Hindawi 2015; 831-60
Category: Neurology
Keywords: serotonin syndrome, SSRI, cyproheptadine (PubMed Search)
Posted: 11/11/2015 by WanTsu Wendy Chang, MD
(Updated: 11/12/2015)
Click here to contact WanTsu Wendy Chang, MD
Last month we discussed causes of serotonin syndrome including common ED medications such as cyclobenzaprine (Flexeril), tramadol (Ultram), metoclopramide (Reglan), and ondansetron (Zofran).
Let’s conclude this series and discuss how to treat serotonin syndrome:
This concludes our 3-part series on serotonin syndrome!
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: serotonin syndrome, SSRI, SNRI, MAOI, TCA (PubMed Search)
Posted: 10/14/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Last month we discussed symptoms of serotonin syndrome and its diagnosis by the Hunter Criteria. Let's move on to what causes serotonin syndrome.
Serotonin Syndrome - What Causes It?

** Stay tuned for the conclusion on management of serotonin syndrome **
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: SAH, cerebral venous thrombosis, head CT (PubMed Search)
Posted: 9/23/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
A thunderclap headache is defined as a very severe headache that reaches its maximum intensity within 1 minute.
One of the most common causes (and the one associated with this buzzword on board questions!) is subarachnoid hemorrhage, but what else can cause a it?
- Reversible cerebral vasoconstriction syndrome (RCVS): suggested by recurrent thunderclap headaches (2-10) over 1 to 2 weeks. Normal CT and LP, with vasoconstriction on angiography. Can lead to SAH, ICH or ischemic stroke.
- Cervical artery dissection
- Cerebral venous sinus thrombosis
- Spontaneous intracranial hypotension: characterized by orthostatic HAs and auditory muffling.
- Intracerebral hemorrhage
- “Primary”: a diagnosis of exclusion
Bottom line? All patients with thunderclap HA should have a stat head CT with no contrast, then have SAH excluded with an LP, CTA or MRI/MRA. Just because you excluded SAH in a patient with thunderclap headache does not mean you’re done with the emergency workup.
TJ Schwedt. Thunderclap Headache. Continuum 2015; 21(4): 1058-71
Category: Neurology
Keywords: serotonin syndrome, SSRI, autonomic hyperactivity, hyperreflexia, clonus, Hunter Criteria (PubMed Search)
Posted: 9/9/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Serotonin Syndrome - What is It?
** Stay tuned for part 2 on what causes serotonin syndrome **
Follow me on Twitter @EM_NCC
