Category: Trauma
Keywords: brain injury, score, prediction (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/23/2025)
Click here to contact Robert Flint, MD
In 252 mild traumatic brain injury patients seen at 3 level I centers that were given the Rivermead Post Concussion Symptoms Questionnaire within 24 hours of arrival, 3 month post concussive symptoms were significantly correlated with their score on the questionnaire. This questionnaire take 3 minutes to complete. This may be helpful in prognosticating who will have post-concussive symptoms and who will need additional follow up.
Gray, Samuel et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Geriatrics
Keywords: hip fracture, nerve block, mortality, delerium (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/20/2025)
Click here to contact Robert Flint, MD
In reviewing the limited literature available, the authors found that fascia iliaca blocks did not improve mortality but did improve hospital length of stay, decreased opiate use, and decreased delirium rates. More research is needed, however this tool should be added to our multimodal pain control toolbox.
Finch, Alexander S. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: rsi, neck injury, penetrating, airway (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/16/2025)
Click here to contact Robert Flint, MD
This group looked at 88 patients intubated for penetrating neck injury and found 95% received neuromuscular blocking agents, 73% were intubated using a bougie, and 95% were intubated on first pass.
The authors concluded; “Rapid sequence intubation with bougie use was an effective default approach to definitive airway management in ED patients with penetrating neck trauma.”
Lee, Daniel H. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: primary care, hypertension, diabetes, trauma (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/9/2025)
Click here to contact Robert Flint, MD
These authors followed 250 consecutive trauma activation patients over a one year period. In hospital elevated blood pressure and glucose level correlated with a new diagnosis of hypertension and diabetes respectively over that 1 year time line. Some of these patients also had a new diagnosis of HIV, substance use disorder and hepatitis C. Using their contact with the health system due to trauma can be a way to screen for undiagnosed medical problems such as diabetes and hypertension. Assuring outpatient follow up for these patients will have an effect on their long term morbidity and mortality.
Banks, Kian C. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: Analgesia, trauma, prehospital, multimodal (PubMed Search)
Posted: 11/1/2025 by Robert Flint, MD
(Updated: 11/2/2025)
Click here to contact Robert Flint, MD
In a German study comparing one EMS jurisdiction which used IV paracetamol (acetaminophen) in combination with nalbuphine (Nubian, opiate agonist/antagonist) to another jurisdiction which used piritramide (synthetic opioid similar to fentanyl) for prehospital traumatic pain, the combination worked better to decrease pain on a numerical scale. There were no differences in typical safety measures.
The use of an antagonist/agonist theoretically could precipitate withdrawal in non-opiate naive patients and could influence in hospital analgesic choices. The literature on this is mixed.
This study offers further evidence of the efficacy of multi-modal pain control, the feasibility of paramedics using IV paracetamol and the possibility of using rapid onset opioid agonist/antagonist in the prehospital setting.
Lohmann, J., Deicke, M., Deslandes, M. et al. Prehospital analgesia for trauma-related pain by paramedics: a comparative retrospective observational study of paracetamol, nalbuphine plus paracetamol, and piritramide. Scand J Trauma Resusc Emerg Med 33, 152 (2025). https://doi.org/10.1186/s13049-025-01470-8
Category: Critical Care
Keywords: Cardiac arrest, norepinephrine, re-arrest, advantage, epinephrine (PubMed Search)
Posted: 11/1/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
A scoping review of literature involving norepinephrine use during cardiac arrest associated with a shockable rhythm found:
-evidence in animal and signal in human trials of improved myocardial and cerebral blood flow
-a suggestion of less re-arrest
There is not enough evidence comparing epinephrine to norepinephrine however this would be an excellent area of research with a theoretical advantage to norepinephrine.
Bouman, S.J., Baldussu, E., Franssen, G.H. et al. The effects of norepinephrine in shockable cardiac arrest, a scoping review. Scand J Trauma Resusc Emerg Med 33, 155 (2025). https://doi.org/10.1186/s13049-025-01480-6
Category: EMS
Keywords: cardiac arrest, mechanical devices, AHA (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/30/2025)
Click here to contact Robert Flint, MD
In the newly released American Heart Association guidelines on CPR and cardiovascular care, they state there is no evidence that mechanical compression devices show improvement in survival when compared to manual CPR. They do not recommend routine use of mechanical devices except when high quality CPR can not be maintained or when healthcare personnel safety is impacted such as during transport to the hospital.
Surely there will be more to follow on this topic.
Part 1: Executive Summary: 2025 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Author:
Marina Del Rios, Jason A. Bartos, Ashish R. Panchal, Dianne L. Atkins, et al.
Publication:
Circulation
Publisher:
Wolters Kluwer Health, Inc.
Date:
Oct 22, 2025
Category: Geriatrics
Keywords: cardiac arrest, older, epinephrine (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/29/2025)
Click here to contact Robert Flint, MD
These authors looked at survival to discharge pre and post-implementation of a single dose epinephrine protocol for out of hospital cardiac arrest as it relates to age ranges. They found that older patients had a survival rate of 12% in the single dose protocol compared to 6% in the multidose protocol. Younger and middle aged patients had no difference in survival pre and post-implementation. At least in older adults, epinephrine does not seem to offer much benefit when given more than one time during cardiac arrest.
Single Dose Epinephrine Protocol Is Associated With Improved Survival of Older Adults With Out-Of-Hospital Cardiac Arrest
Ethan J. Lilien, Nicklaus P. Ashburn, Tyler S. George, Anna C. Snavely, Bryan P. Beaver, Casey G. Costa, Michael A. Chado, Harris A. Cannon, James E. Winslow, R. Darrell Nelson … See all authors
First published: 25 September 2025 Academic Emergency Medicine
Category: EMS
Keywords: single dose, epinephrine, cardiac arrest, survival (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/27/2025)
Click here to contact Robert Flint, MD
The authors conducted a pre- and post-implementation study after five North Carolina county EMS agencies switched to single dose epinephrine during out of hospital cardiac arrest treatment from the traditional multidose (every 3-5 minutes) protocol. They looked at 1 year before and 1 year after implementation. They found no difference in survival to discharge from the hospital in the two groups but there was less return to spontaneous circulation in the single dose group.
Ashburn, N. P., Beaver, B. P., Snavely, A. C., Nazir, N., Winslow, J. T., Nelson, R. D., … Stopyra, J. P. (2022). One and Done Epinephrine in Out-of-Hospital Cardiac Arrest? Outcomes in a Multiagency United States Study. Prehospital Emergency Care, 27(6), 751–757. https://doi.org/10.1080/10903127.2022.2120135
Category: Trauma
Keywords: brain injury, evidence, eucapnia, normotensive, care (PubMed Search)
Posted: 10/25/2025 by Robert Flint, MD
(Updated: 10/26/2025)
Click here to contact Robert Flint, MD
Another paper emphasizing care for brain injured patients should include:
-pre-intubation preoxygenation to avoid hypoxia
-pre-intubation avoid extremes in blood pressure (hypotension kills)
-use hemodynamically neutral induction agents such as ketamine or etomidate
-post intubation target eucapnia on the ventilator. (do not aim for low CO2)
-post intubation maintain adequate sedation to avoid increased intercranial pressure
Hoyne J, Edlow J. Airway Management in Patients With Acute Brain Injury or Ischemia. J Emerg Med. 2025 Jul;74:125-133. doi: 10.1016/j.jemermed.2024.12.015. Epub 2025 Jan 6. PMID: 40348691.
Category: Geriatrics
Keywords: RSV, geriatric, heart failure, morbidity (PubMed Search)
Posted: 10/19/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This study looked at older patients admitted to the hospital with a diagnosis of one of the following: RSV infection, UTI, influenza, fracture. Those patients with RSV had longer stays, higher mortality, higher ICU length of stay and interestingly more cardiovascular complications up to one year after hospitalization. Further evidence we should be testing for RSV in our ill older patients and encouraging vaccination.
Category: Geriatrics
Keywords: fall, score, geriatric, prediction (PubMed Search)
Posted: 10/11/2025 by Robert Flint, MD
(Updated: 10/12/2025)
Click here to contact Robert Flint, MD
These authors used information available from both the medical record as well as from a survey instrument given in the emergency department to created this fall risk score. A score over 6 had a 63% sensitivity and 75% specificity of predicting future falls.
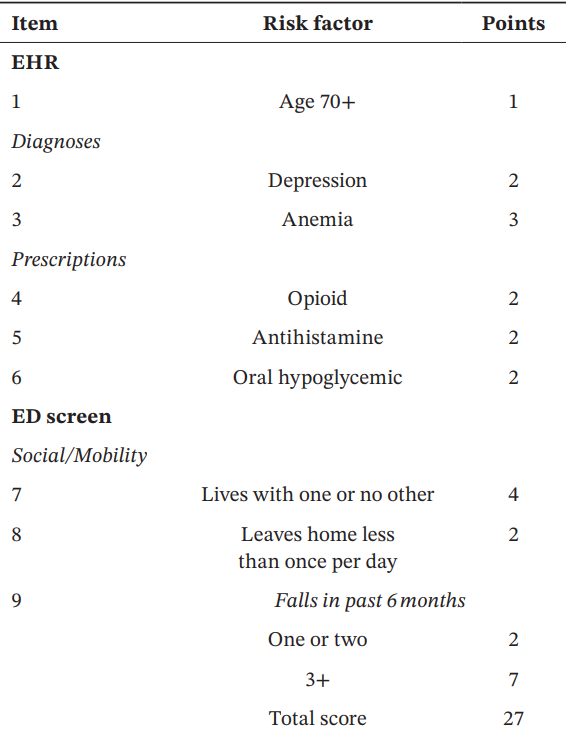

Acaemic Emergency Medicine 2025 0:1-12
Category: Gastrointestional
Keywords: GI bleed, presentation, antithrombotics (PubMed Search)
Posted: 10/8/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In a retrospective observational study comparing patients both on and not on antithromotics (DOAC/warfarin or anti platelets) who presented with a GI bleed these authors found:
“Patients with anticoagulant therapy more often present with a lower source of GI bleeding than both those on antiplatelet medications and those with no antithrombotics. Overall patients on anticoagulants are also less likely to present with hematemesis, even with a later confirmed upper GI bleeding. Furthermore, results indicate that the need for endoscopic interventions and transfusions are dependent on initial presenting symptoms but not affected by antithrombotic therapy at admission.”
Forsberg-Puckett, A., Wurm Johansson, G. & Regnér, S. Presentation of gastrointestinal bleeding in patients with antithrombotic therapy, results from a consecutive retrospective cohort. Scand J Trauma Resusc Emerg Med 33, 146 (2025). https://doi.org/10.1186/s13049-025-01431-1
Category: Trauma
Keywords: head injury, trauma, geriatric (PubMed Search)
Posted: 10/4/2025 by Robert Flint, MD
(Updated: 10/5/2025)
Click here to contact Robert Flint, MD
This paper reminds us older patients have higher mortality and worse outcomes overall if their injury includes a head injury. Any mechanism that results in head injury, including fall from standing, has a higher potential for death, disability, and long term cognitive decline in older patients. Triaging these patients to trauma centers can lead to better outcomes. The difficulty is knowing which patients to send to trauma centers vs. emergency departments. The authors write:
"clinicians should consider transporting to a trauma center in geriatric patients with head trauma, if feasible. However, given the frequency with which head injury occurs, transportation to a trauma center for all patients with head trauma is likely to overwhelm EMS systems and hospitals. Unfortunately, the existing literature does not delineate the subset of patients whose condition will benefit from this evaluation . Given these considerations, we recommend EMS clinicians consider abnormal mental status, presence of anti-coagulation, and loss of consciousness as considerations to transport to a trauma center in cases where the need for trauma center evaluation is not clear.”
Haussner, W. K., Breyre, A. M., Bascombe, K., Barrett, W. J., Camacho, M. A., Overton-Harris, P., … Colwell, C. (2025). Prehospital Trauma Compendium: Management of Geriatric Trauma Patients – A Position Statement and Resource Document of NAEMSP. Prehospital Emergency Care, 1–10. https://doi.org/10.1080/10903127.2025.2557006
Category: Geriatrics
Keywords: trauma, geriatric, prehospital, EMS (PubMed Search)
Posted: 10/4/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Reenforcing the recent pearl on geriatric trauma patient care, here is the National Association EMS Physicians statement on prehospital care.
"EMS clinicians should use age-adjusted, physiologic criteria to guide decisions to transport geriatric trauma patients to the most appropriate level of trauma center available in the community.
Geriatric trauma patients should be promptly evaluated for pain and should receive analgesic interventions in a timely manner. Analgesic medications should be dosed following weight-based guidance and should be administered with consideration of potential drug interactions and age-related changes in drug metabolism and side effects.
EMS clinicians should consult advance care planning documents, e.g., Physician Orders for Life-Sustaining Treatment (POLST), when available, to guide care in emergency scenarios, including management of traumatic injuries.
While older patients are at higher risk for spinal injuries, including lumbar and cervical spine fractures, traditional spinal motion restriction practices may not be suitable for older patients due to age-related anatomic changes in spinal alignment and increased risk for cutaneous pressure-related injuries. EMS clinicians should exercise judgment to determine when and how to best achieve spinal motion restriction if spinal injury is suspected in geriatric trauma patients."
Haussner, W. K., Breyre, A. M., Bascombe, K., Barrett, W. J., Camacho, M. A., Overton-Harris, P., … Colwell, C. (2025). Prehospital Trauma Compendium: Management of Geriatric Trauma Patients – A Position Statement and Resource Document of NAEMSP. Prehospital Emergency Care, 1–10. https://doi.org/10.1080/10903127.2025.2557006
Category: Geriatrics
Keywords: geriatrics, frail, diverticulitis (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 10/1/2025)
Click here to contact Robert Flint, MD
This retrospective study looking at a readmission database for patients greater than 65 years categorized 10,000 patients into non-frail, pre-frail and frail based on the five-factor modified frailty index. They found no difference in recurrent diverticulitis among the groups but did find:
“frailty was a predictor of mortality on index hospitalization (adjusted odds ratio, 1.99; p < 0.001) and readmissions (adjusted odds ratio, 3.05; p < 0.001)…frail patients are at increased risk of mortality once they develop diverticulitis. Optimal management for frail patients with diverticulitis must be defined to improve outcomes.”
Once again, assessing your patient's frailty can help you predict outcomes and have meaningful discussions with patients and their families.
Hejazi, Omar MD; Colosimo, Christina DO, MS, FACS; Khurshid, Muhammad Haris MD; Stewart, Collin MD, FACS; Al Ma'ani, Mohammad MD; Anand, Tanya MD, MPH, FACS; Castillo Diaz, Francisco MD; Castanon, Lourdes MD, FACS; Magnotti, Louis J. MD, MS, FACS; Joseph, Bellal MD, FACS. Does frailty predict readmission and mortality in diverticulitis? A nationwide analysis. Journal of Trauma and Acute Care Surgery 99(4):p 605-610, October 2025. | DOI: 10.1097/TA.0000000000004707
Category: Critical Care
Keywords: compartment syndrome, abdomen, critically ill (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 9/28/2025)
Click here to contact Robert Flint, MD
This review article reminds us that abdominal hypertension and compartment syndrome need to remain on our differential diagnosis for critically ill and injured patients. Pressure is measured with an intra-bladder catheter. Normal pressure is 5-7 mm HG. Sustained over 12 mm Hg is hypertension and sustained over 20 mm Hg is compartment syndrome.
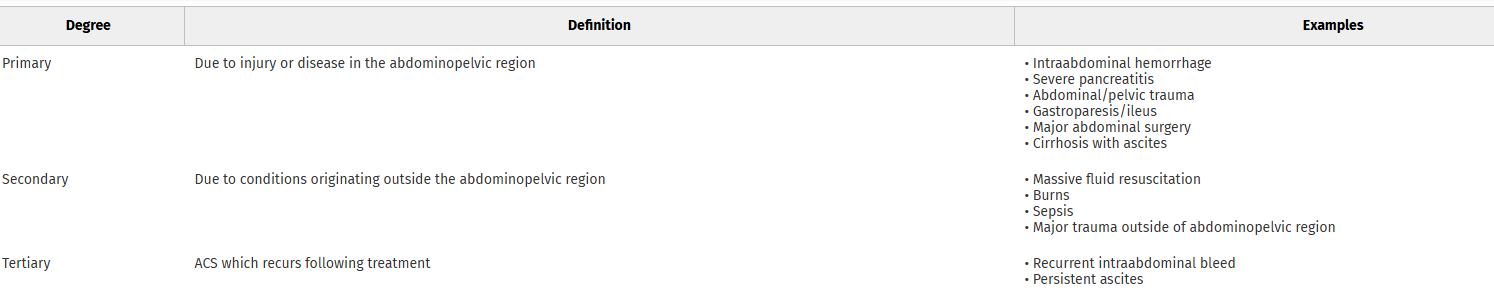
Arcieri, Talia R. MD; Meizoso, Jonathan P. MD, MSPH, FACS. Intraabdominal hypertension and abdominal compartment syndrome: What you need to know. Journal of Trauma and Acute Care Surgery 99(4):p 504-513, October 2025. | DOI: 10.1097/TA.0000000000004603
Category: Toxicology
Keywords: alcohol withdrawal, phenobarbital, protocol, implimentation (PubMed Search)
Posted: 9/24/2025 by Robert Flint, MD
(Updated: 9/25/2025)
Click here to contact Robert Flint, MD
This study looking at pre and post-phenobarbital order set use to treat inpatient alcohol withdrawal syndrome found:
“AWS symptoms resolved more rapidly after implementation, with a 4.2- to 5.0-point reduction in daily maximum CIWA-Ar scores at 24 to 96 hours from hospital presentation, 30.1-hour reduction in AWS treatment duration (95% CI, 16.7-43.5 hours), and 2.2-day reduction in time to hospital discharge (95% CI, 0.7-3.7 days). Safety outcomes did not significantly differ before and after implementation.”
Remember phenobarbital can be used for alcohol withdrawal for our ED patients as well.
Here is the protocol:
Nursing
Vital signs 10 minutes after phenobarbital loading dose
Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) every 1-4 hours based on score
Loading Dose
Phenobarbital 15 mg/kg intravenous piggyback (recommended for most patients)
Phenobarbital 10 mg/kg intravenous piggyback (low risk or heavily pretreated with benzodiazepines)
As-Needed Doses
Phenobarbital 130 mg intravenous twice as needed for uncontrolled agitation or CIWA-Ar ?15
Phenobarbital 260 mg intravenous once as needed for uncontrolled agitation or CIWA-Ar ?15
Wolpaw BJ, Oren H, Quinnan-Hostein L, et al. Hospital-Wide Implementation, Clinical Outcomes, and Safety of Phenobarbital for Alcohol Withdrawal. JAMA Netw Open. 2025;8(8):e2528694. doi:10.1001/jamanetworkopen.2025.28694
Category: Trauma
Keywords: Head injury, geriatric, interracial hemorrhage (PubMed Search)
Posted: 9/21/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This systematic review of the literature found four findings associated with intercranial hemorrhage in older patients after a fall. They were: focal neurologic findings, external signs of trauma on the head, loss of consciousness, and male sex.
We still need better studies as this is completely based on the quantity and quality of literature available to review. This information is not enough to change liberal CT imagining in older patients after a fall. It is the beginning of the study process.
Dubucs X, Gingras V, Boucher V, Carmichael PH, Ruel M, De Wit K, Grewal K, Mercier É, Blanchard PG, Benhamed A, Charpentier S, Émond M. Risk Factors for Traumatic Intracranial Hemorrhage in Older Adults Sustaining a Head Injury in Ground-Level Falls: A Systematic Review and Meta-analysis. Ann Emerg Med. 2025 Jul 22:S0196-0644(25)00313-0. doi: 10.1016/j.annemergmed.2025.05.021. Epub ahead of print. PMID: 40699169.
Category: Trauma
Keywords: TXA, EMS, prehospital, consensus (PubMed Search)
Posted: 9/14/2025 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
The National Association of EMS Physicians, the American College of Surgeons Committee on Trauma, and the American College of Emergency Physicians recommends:
• Prehospital TXA administration may reduce mortality in adult trauma patients with hemorrhagic shock when administered after lifesaving interventions.
• Prehospital TXA administration appears safe, with low risk of thromboembolic events or seizure.
• The ideal dose, rate, and route of prehospital administration of TXA for adult trauma patients with hemorrhagic shock has not been determined. Current evidence suggests EMS agencies may administer either a 1-g intravenous/intraosseous dose (followed by a hospital-based 1-g infusion over 8 hours) or a 2-g intravenous/intraosseous dose as an infusion or slow push.
• Prehospital TXA administration, if used for adult trauma patients, should be given to those with clinical signs of hemorrhagic shock and no later than 3 hours post-injury. There is no evidence to date to suggest improved clinical outcomes from TXA initiation beyond this time or in those without clinically significant bleeding.
• The role of prehospital TXA in pediatric trauma patients with clinical signs of hemorrhagic shock has not been studied, and standardized dosing has not been established. If used, it should be given within 3 hours of injury.
• Prehospital TXA administration, if used, should be clearly communicated to receiving health care professionals to promote appropriate monitoring and to avoid duplicate administration(s).
• A multidisciplinary team, led by EMS physicians, that includes EMS clinicians, emergency physicians, and trauma surgeons should be responsible for developing a quality improvement program to assess prehospital TXA administration for protocol compliance and identification of clinical complications.
Barrett, Whitney J. MD; Kaucher, Kevin A. PharmD, BCCCP; Orpet, Ross E. MD; Campion, Eric M. MD; Goodloe, Jeffrey M. MD; Fischer, Peter E. MD, MS, NRP; Colwell, Christopher B. MD; Lyng, John W. MD, NRP. Tranexamic acid in trauma: A joint position statement and resource document of NAEMSP, ACEP, and ACS-COT. Journal of Trauma and Acute Care Surgery 99(3):p 357-363, September 2025. | DOI: 10.1097/TA.0000000000004727
