Category: Trauma
Keywords: Stab wound, chest radiograph, pneumothorax (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This small study from South Africa shows stab wounds to the chest with a pneumothorax less than 0.5 cm that were managed conservatively had completely resolved on 12 hour repeat chest X-ray. This could facilitate earlier discharge of these patients. It also supports conservative (non-tube placement) approach to asymptomatic small pneumothoraces from stab wounds.
Kong V, Cheung C, Lee D, et al. Defining the optimal timing of interval chest radiograph in conservatively managed small pneumothorax from thoracic stab wounds – a South African experience. Trauma. 2025;28(1):14-17. doi:10.1177/14604086251396434
Category: Geriatrics
Keywords: Tramadol, geriatrics (PubMed Search)
Posted: 1/29/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Tramadol has been viewed as a safer alternative for pain control than opioids. This study says differently.
“Tramadol use was associated with increased risk of multiple ER utilizations, falls/fractures, CVD hospitalizations, safety event hospitalizations, and mortality (new users only) compared to nonuse.”
Musich S, Wang SS, Schaeffer JA, Slindee L, Kraemer S, Yeh CS. Safety Events Associated with Tramadol Use Among Older Adults with Osteoarthritis. Popul Health Manag. 2021 Feb;24(1):122-132. doi: 10.1089/pop.2019.0220. Epub 2020
Category: Trauma
Keywords: Pelvic fracture, EMS (PubMed Search)
Posted: 1/25/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
A reminder from a recent position paper on pelvic trauma that we should not be doing stability testing to evaluate pelvic trauma
“EMS clinicians should recognize the challenges in accurately identifying pelvic fractures by physical exam alone. Manual stability testing of the pelvis is neither sensitive nor specific and may cause harm.”
Lyng, J. W., Corsa, J. G., Raetzke, B. D., Wilson, B. R., McCoy, A., Patterson, S. C., … Bosson, N. (2025). Prehospital Trauma Compendium: Evaluation and Management of Suspected Pelvis Fractures – An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 1–35. https://doi.org/10.1080/10903127.2025.2540420
Category: Geriatrics
Keywords: Delerium, antihistamine, geriatrics (PubMed Search)
Posted: 1/18/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In 261 ED patients over age 65 receiving first generation antihistamines, 15% had an adverse reaction. Most common was delirium and urinary retention. Age over 85, previous cognitive impairment and multiple doses increased the risk of adverse reaction. Along with previous literature, this should discourage use of first generation antihistamines in older ED patients.
Killen, E., Cusumano, M., Zhang, Z., Newman, R., Voigtmann, J., Sanford, A. M, & Bitter, C. C. (2025). First-Generation Antihistamine Use in Geriatric Emergency Department Patients: Retrospective Review. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 27(1). http://dx.doi.org/10.5811/westjem.47491 Retrieved from https://escholarship.org/uc/item/7230n5z1
Category: Toxicology
Keywords: Opiate use disorder, MOUD, initiation (PubMed Search)
Posted: 1/15/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In this study reviewing data from the American College of Emergency Physicians’ Emergency Quality Network substance use disorder program, EDs prescribed naloxone in 27% of patients discharged after opioid overdose. Only 7% received ED administered or prescription for buprenorphine, etc. There is a lot of room for improvement in the care we provide for this subset of ED patients.
Weiner, Scott G. et al.
Annals of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: Prehospital, transfusion, non-trauma (PubMed Search)
Posted: 1/11/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Much has been written about the benefits of prehospital blood transfusion for traumatic hemorrhage. Can this success be ascribed to non-traumatic hemorrhage as well? This small study (50 patients over 10 years!) says there were improvements in patient physiology (shock index) for those patients receiving blood for GI bleed, etc. Much more research is needed however this could be a beneficial practice in the future.
Kodakadath, H., Dillane, S., Griggs, J. et al. Pre-hospital blood transfusion in non-traumatic major haemorrhage: a retrospective observational study. Scand J Trauma Resusc Emerg Med 33, 191 (2025). https://doi.org/10.1186/s13049-025-01495-z
Category: Trauma
Keywords: Ketamine, nebulized, pain control (PubMed Search)
Posted: 1/3/2026 by Robert Flint, MD
(Updated: 1/4/2026)
Click here to contact Robert Flint, MD
This systematic review found improved pain scale at 15 and 120 minutes in 495 patients who received nebulized ketamine. Dosing at 0.75 mg/kg was as effective as 1.5 mg/kg and the nebulized ketamine was non-inferior to IV morphine and ketamine with fewer side effects.
Kirk, D., Whiles, E., Jones, A. et al. Breathing new life into pain management: a systematic review of nebulised ketamine for analgesia. Scand J Trauma Resusc Emerg Med 33, 196 (2025). https://doi.org/10.1186/s13049-025-01501-4
Category: Geriatrics
Keywords: FRAIL, geriatric, prediction tool, Barthel (PubMed Search)
Posted: 1/1/2026 by Robert Flint, MD
(Updated: 1/3/2026)
Click here to contact Robert Flint, MD
The Geriatric Measurement Tool (GMT) was used in this study prospectively to assess 24 hour mortality rate in ED patients over age 65. The GMT is a combination of FRAIL Questionnaire and Barthel index for Activity of Daily Living. The study found:
“ From 700 enrolled patients, GMT categorization revealed that 53.6% of patients were in Category-4 (moderate/more dependent and frail), while 34% were in Category-1 (independent or slight dependency, prefrail/fit). The 24-h mortality rate was 9%. GMT Category-4 demonstrated high sensitivity (87.3%) for mortality prediction, but low specificity (49.7%). Conversely, GMT Category-1 showed low sensitivity (44.1%) but high specificity (90.2%) for predicting discharge.”
Probably the biggest take away is we should be thinking about assessing our older patient's health status using some validated scale/tool to help us have conversations with patients and families regarding prognosis and interventions.
Category: Geriatrics
Keywords: FRAIL, geriatric, prediction tool, mortality, (PubMed Search)
Posted: 1/1/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
The Geriatric Measurement Tool combines the FRAIL Questionnaire with the Barthel Index For Daily Living to give a prognosis on your patient's mortality. First used to predict mortality in older patients with pneumonia during COVID-19 pandemic. Now being investigated for other ED patient populations.
FRAIL Questionnaire: Fatigue, Resistance, Aerobic, Illness, Weight loss. https://www.activeagingweek.com/pdf/abbott/FRAILQuestionnaire.pdf
Barthel: Ten questions about ADL's to create a score 0-100. https://www.mdcalc.com/calc/3912/barthel-index-activities-daily-living-adl
Zaman, Süeda et al. Journal of Emergency Medicine, Volume 79, 560 - 567
2. Gómez-Moreno, C., Chacón-Corral, A.A., Pérez-Méndez, A. et al. Association between a geriatric measure tool and adverse outcomes among older adults treated in an emergency department: a retrospective cohort study. Intern Emerg Med 20, 2205–2213 (2025). https://doi.org/10.1007/s11739-024-03843-w
Category: Administration
Keywords: industry sponsored, money, research, PI (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/31/2025)
Click here to contact Robert Flint, MD
This study looked at industry sponsored payments to EM physician through non-covered entities (ie not directly to physician or through an academic institution). It found a $100 million increase from 2015-23 in this payment model. It appears that private equity is not the only money entering emergency medicine in the past decade.
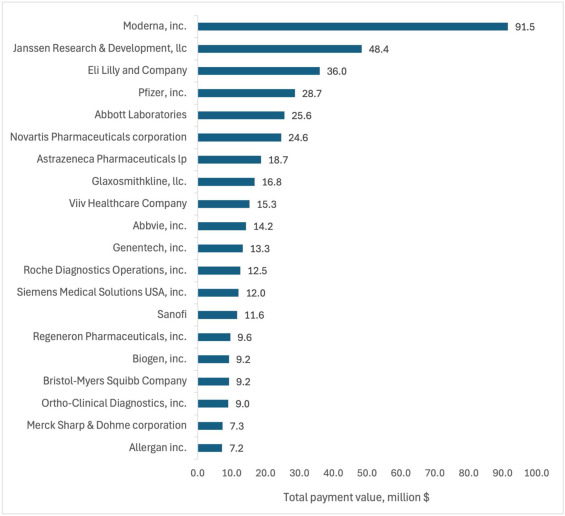
Total value of Industry-Sponsored Research Payments (ISRPs) by company. The 20 companies with highest total ISRPs awarded to emergency physician PIs.
Rizer, Nicholas W et al.
Journal of Emergency Medicine, Volume 79, 21 - 30
Category: Quality Assurance/Quality Improvement
Keywords: radiology, report, risk, management (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/29/2025)
Click here to contact Robert Flint, MD
We have all been on that busy shift and just quickly looked at the impression section of the radiology report whether that is a CT, plain film, US or MRI. In doing this you run the risk of missing important information that is contained in the body of the report and has either not been carried down into the impression or contradicts the impression by some error.
To avoid missing important information that can impact patient care, always read the entire report and look at the images yourself. You have seen the patient, know the clinical history, and a second set of eyes never hurts.
Category: Trauma
Keywords: hypocalcemia, trauma, mortaility, rate (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/28/2025)
Click here to contact Robert Flint, MD
Previous small studies had put the prevalence of hypocalcemia in trauma patients at 23-56%. This single center study of 2200 patients looked at prevalence and outcome and found a much lower prevalence however worse outcomes than those who were not hypocalcemic.
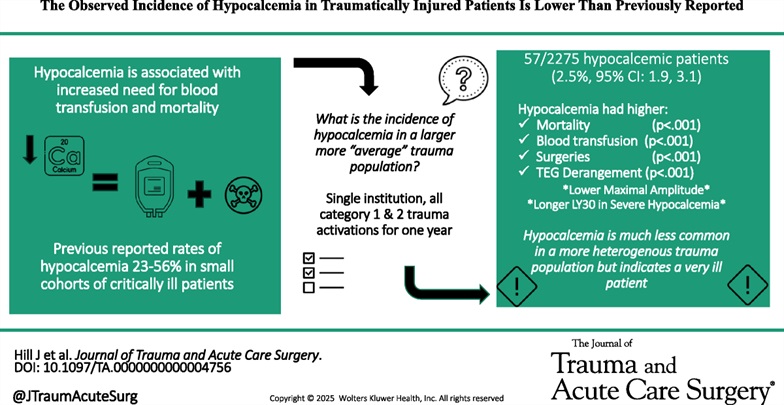
Hill, Joshua H. MD; Shah, Bhairav DO; Rady, Emily MD; Lieber, Michael MS; Lauria, Julia DO; Lee, Katarina DO; Wierzbicki, Katrina BS; Kashikar, Tanisha DO; Kincaid, Michelle MD. The observed incidence of hypocalcemia in traumatically injured patients is lower than previously reported. Journal of Trauma and Acute Care Surgery 99(6):p 920-927, December 2025. | DOI: 10.1097/TA.0000000000004756
Category: Geriatrics
Keywords: delirium, hip fracture, nerve block (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study is a reminder of the efficacy of regional nerve blocks for older patient's with hip fractures. The authors trained EM physicians for 2 hours then evaluated delirium levels in patients who did and did not receive nerve blocks for hip fractures.
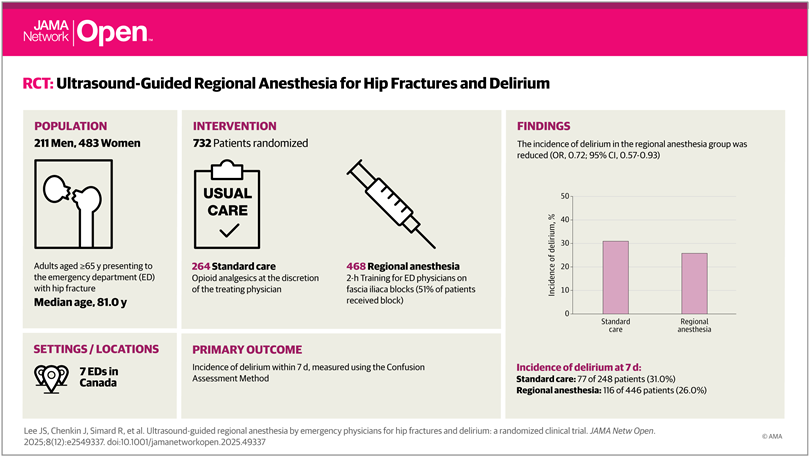
Lee JS, Chenkin J, Simard R, et al. Ultrasound-Guided Regional Anesthesia by Emergency Physicians for Hip Fractures and Delirium: A Randomized Clinical Trial. JAMA Netw Open. 2025;8(12):e2549337. doi:10.1001/jamanetworkopen.2025.49337
Category: Trauma
Keywords: prehospoital, blood, survival, unexpected (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/25/2025)
Click here to contact Robert Flint, MD
This study demonstrated that administration of prehospital blood to trauma patients lead to a higher rate of survival in patients whose initial ED vital signs or pre-hospital shock index would have predicted death.
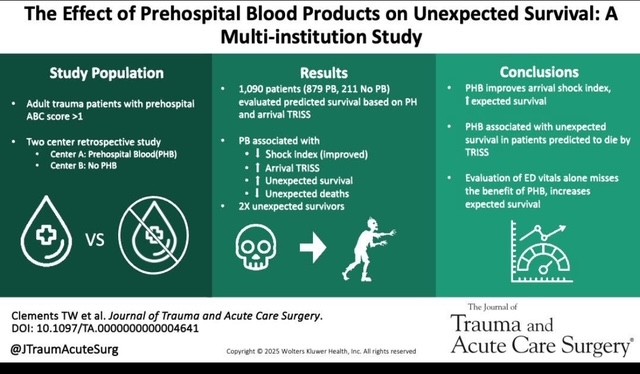
Clements TW, Van Gent JM, Krzyzaniak A, Campbell B, Carroll A, Mericle M, Sise M, Peck KA, Cotton BA. The effect of prehospital blood products on unexpected survival: A multi-institution study. J Trauma Acute Care Surg. 2025 May 2. doi: 10.1097/TA.0000000000004641. Epub ahead of print. PMID: 40312787.
Category: Trauma
Keywords: shock, CAB, resuscitation, trauma, circulation (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 12/14/2025)
Click here to contact Robert Flint, MD
This review article reminds us that circulation needs to be prioritized over airway in trauma patients. This means bleeding control (pressure on wound, tourniquet, surgery/IR intervention), correcting tension pneumothorax, correcting pericardial tamponade, as well as resuscitation to return physiologic homeostasis (blood products, vasopressors where needed, warm the patient, etc.) before intubation. Altered mental status/low GCS may be due more to hypoperfusion than neurologic injury. Correcting the hypotension may alleviate that need to intubate.
Ferrada, Paula MD, FACS, FCCM, MAMSE; Duchesne, Juan MD, FACS, FCCM, FCCP; Piehl, Mark MD, MPH. Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 679-683, November 2025. | DOI: 10.1097/TA.0000000000004618
Category: Infectious Disease
Keywords: sepsis, intrabdominal, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/30/2025)
Click here to contact Robert Flint, MD
Intraabdominal infections leading to sepsis can come from cholecystitis, small bowel perforation, gastric perforation, left sided colonic diverticulitis, right sided diverticulitis and appendicitis. When to initiate source control and antibiotics is controversial. These authors propose breaking patient populations into three groups:
From this they propose algorithms to treat these intraabdominal infections such as (note the different approach to right and left diverticulitis):
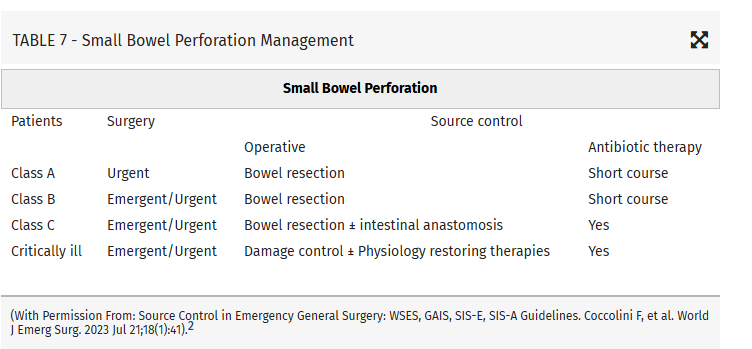
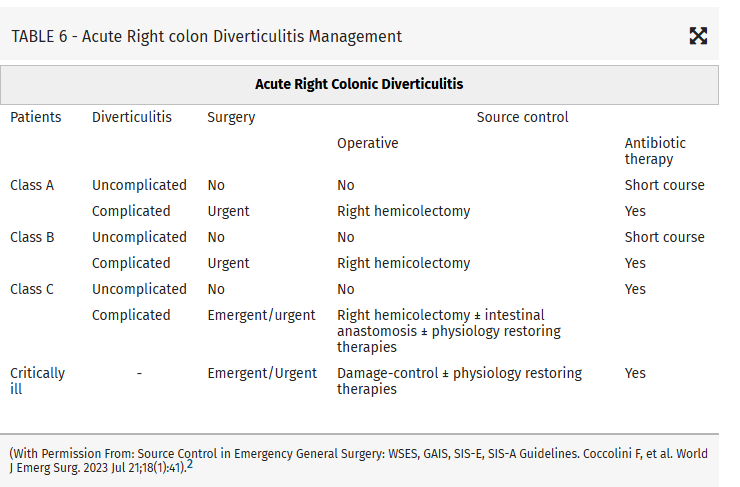
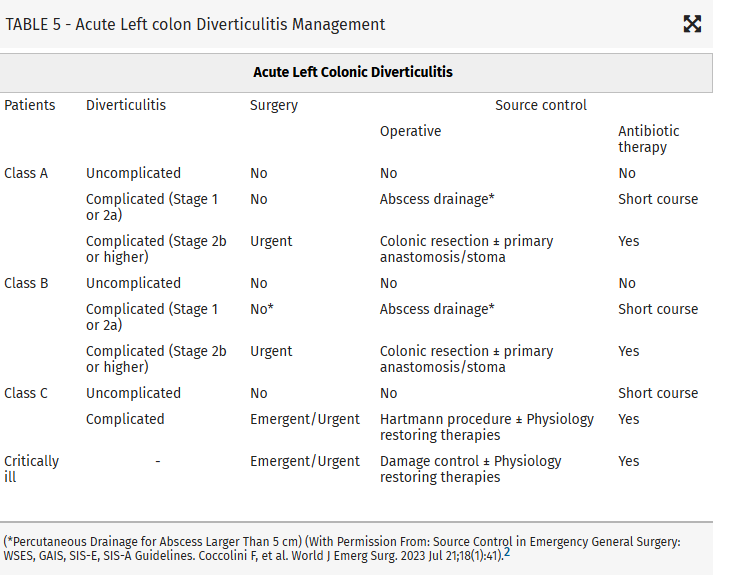
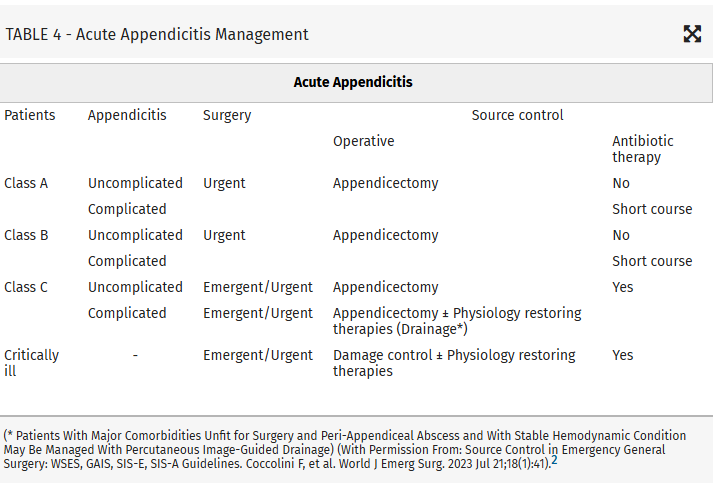
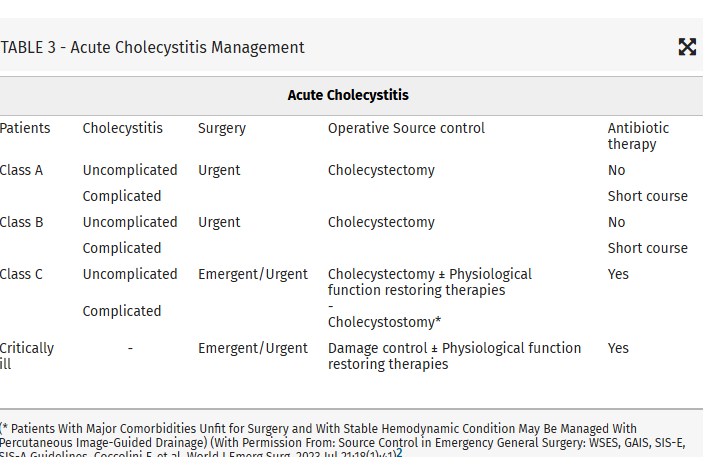
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Infectious Disease
Keywords: sepsis, intrabdominal source, source control (PubMed Search)
Posted: 11/28/2025 by Robert Flint, MD
(Updated: 11/29/2025)
Click here to contact Robert Flint, MD
This article looks at source control as it relates to intrabdominal sources for sepsis. Key take aways are:
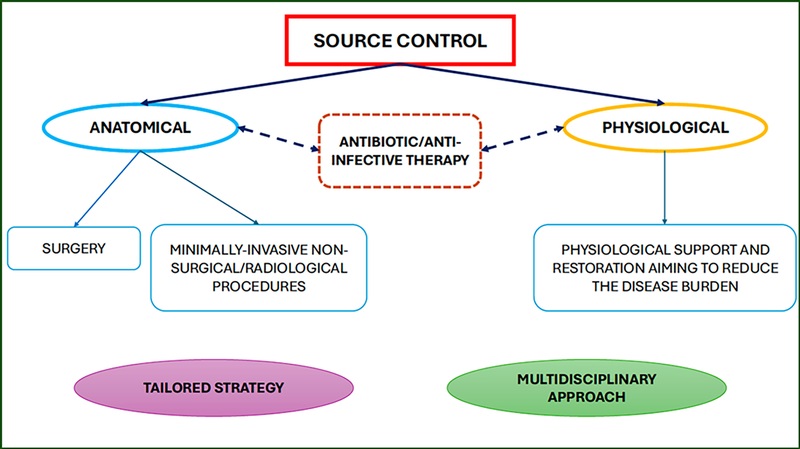
Those at high risk of morbidity and mortality from intraabdominal infection associated sepsis include:
Mild–moderate immune deficiency: Elderly (according to the age and general status of the patient), Malnourished, Diabetic, Burns, Trauma, Uremic, Active malignancy, not on chemotherapy, HIV with CD4+ count >200/mm3, Splenectomized, Severe immune deficiencyAIDS HIV with CD4+ count <200/mm3, Transplant (solid organ, bone marrow), High-dose steroids (more than 20 mg/day prednisone), Malignancy on chemotherapy, Neutrophil count <1,000/mm3
High-risk population (medical or surgical causes)Low serum albumin concentration Older age Obesity Smoking Diabetes mellitus Ischemia secondary to vascular disease or irradiation Prolonged or delayed/late procedures
Coccolini, Federico MD, PhD; Kirkpatrick, Andrew W. CD, MD, MHSc, FRCSC, FACS; Cremonini, Camilla MD, PhD; Sartelli, Massimo MD, PhD. Source control in intra-abdominal infections: What you need to know. Journal of Trauma and Acute Care Surgery 99(5):p 669-678, November 2025. | DOI: 10.1097/TA.0000000000004654
Category: Misc
Keywords: prescribing, racial, disparity (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/28/2025)
Click here to contact Robert Flint, MD
Comparing prescribing patterns from early 2000s to late 2010s in the National Hospital Ambulatory Medical Care Survey, these authors found we continue to under prescribe pain medications to non-white patients for traumatic injuries.
Day, Jessica et al.
Journal of Emergency Medicine, Volume 78, 184 - 191
Category: Geriatrics
Keywords: frail, frailty scale, geriatrics, critical care (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/27/2025)
Click here to contact Robert Flint, MD
A prospective cohort of South Korean patients over 65 years admitted from the ED with critical illness had Clinical Frailty Scale (CFS) performed on them. Those with a high CFS had increased 3 month mortality. CFS helps us prognosticate morbidity and mortality in our older critically ill patients.
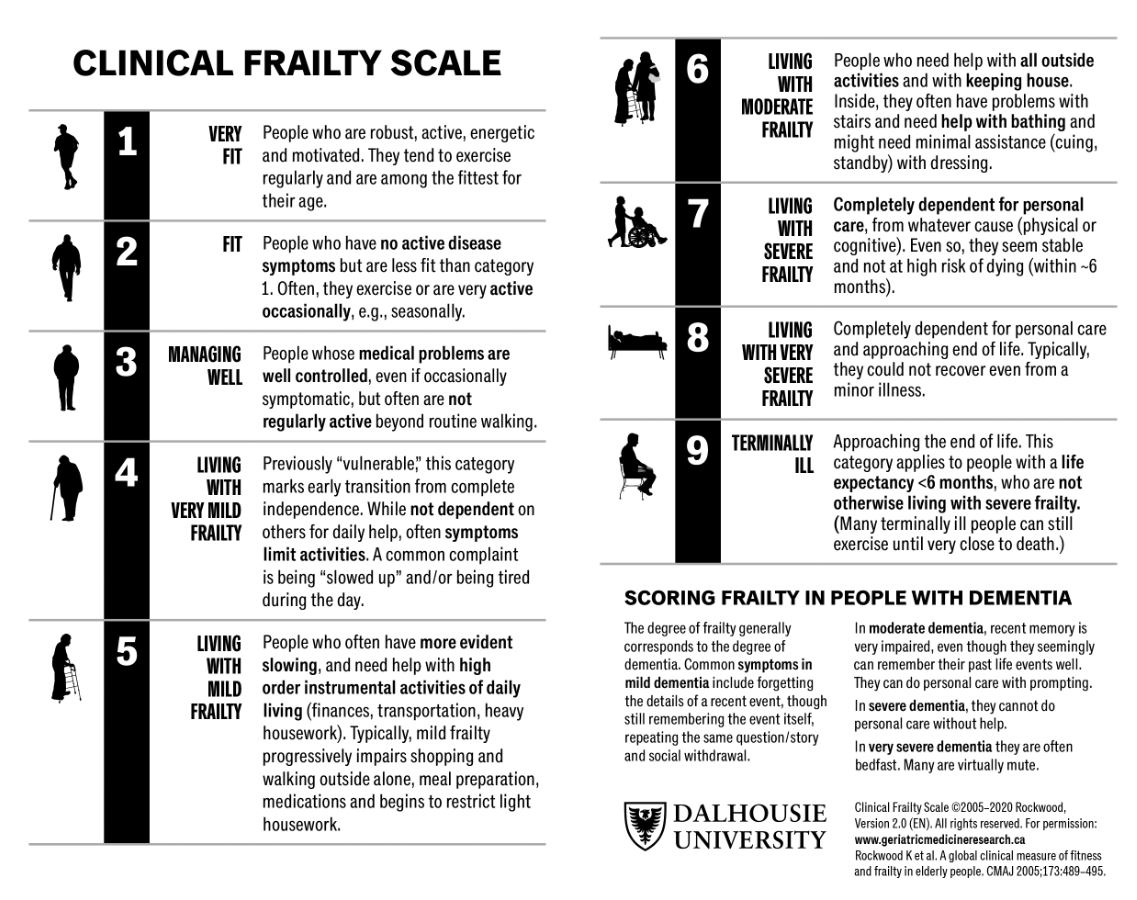
Um, Young Woo et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: brain injury, score, prediction (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/23/2025)
Click here to contact Robert Flint, MD
In 252 mild traumatic brain injury patients seen at 3 level I centers that were given the Rivermead Post Concussion Symptoms Questionnaire within 24 hours of arrival, 3 month post concussive symptoms were significantly correlated with their score on the questionnaire. This questionnaire take 3 minutes to complete. This may be helpful in prognosticating who will have post-concussive symptoms and who will need additional follow up.
Gray, Samuel et al.
Journal of Emergency Medicine, Volume 0, Issue 0
