Category: Neurology
Keywords: syncope, vasovagal, orthostatic, blood pressure (PubMed Search)
Posted: 5/24/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Vasovagal syncope is a subtype of neurally mediated syncope, and it is distinctly different from orthostatic hypotension.
Patients with orthostatic syncope have severe orthostatic hypotension that results in transient loss of consciousness immediately or within moments of standing up. This is different from neurally mediated syncope, which develops gradually under conditions of prolonged orthostatic stress such as standing for several minutes. Tilt table testing is useful for true orthostatic syncope, but not for neurally mediated syncope. In addition, checking for “orthostatic hypotension” may not capture patient with orthostatic syncope, because the hypotension occurs so quickly after standing up. Of note, patients may still have orthostatic tachycardia or intolerance with neurally mediated syncope.
Category: Neurology
Keywords: syncope, vasovagal, seizures, orthostatic, blood pressure (PubMed Search)
Posted: 5/10/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Cheshire WP. Syncope. Continuum 2017;23(2):335–358.
Category: Neurology
Keywords: vasogenic cerebral edema, white matter, blood-brain-barrier, steroids (PubMed Search)
Posted: 4/26/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Case image courtesy of Dr David Cuete, Radiopaedia.org, rID: 23178
Follow me on Twitter @EM_NCC!
Category: Neurology
Keywords: Glasgow Coma Scale, GCS, motor GCS, mGCS, Simplified Motor Scale, SMS (PubMed Search)
Posted: 4/12/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The motor GCS and Simplified Motor Scale (SMS) have similar discrimination when compared with the total GCS, and may be easier to use.
Chou R, Totten AM, Carney N, et al. Predictive Utility of the Total Glasgow Coma Scale Versus the Motor Component of the Glasgow Coma Scale for Identification of Patients with Serious Traumatic Injuries. Ann Emerg Med. 2017 Jan 11. [Epub ahead of print].
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: CT, MRI, tPA, peripartum, PRES (PubMed Search)
Posted: 3/22/2017 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Majerisk JJ. Inherited and Uncommon Causes of Stroke. Continuum 2017;23(1):211–237.
Category: Neurology
Keywords: headache, migraine, intravenous fluids, IVF (PubMed Search)
Posted: 3/8/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: stroke, alcohol, substance abuse, mimics (PubMed Search)
Posted: 2/22/2017 by Danya Khoujah, MBBS
(Updated: 2/1/2026)
Click here to contact Danya Khoujah, MBBS
Category: Neurology
Keywords: aphasia, fluency, comprehension, repetition, Broca's aphasia, Wernicke's aphasia, conduction aphasia (PubMed Search)
Posted: 2/8/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Types of aphasia [Online image]. Retrieved February 8, 2017 from https://www.aphasia.org/
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: weakness, ptosis (PubMed Search)
Posted: 1/25/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Patients may present to the ED with new onset weakness due to myasthenia gravis (MG). A group that is frequently missed is late-onset MG, which occurs after the age of 50. It is frequently misdiagnosed as a stroke or transient ischemic attach (TIA).
Two cardinal features:
Bonus pearl: Ocular symptoms are present in up to 85% of patients with MG, with unilateral ptosis or asymmetric bilateral ptosis being the most common presentations.
Nicolle MW. Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome. Continuum. 2016;22(6):1978–2005
Category: Neurology
Keywords: concussion, driving performance, cognitive impairment (PubMed Search)
Posted: 1/11/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Schmidt JD, Hoffman NL, Ranchet M, et al. Driving after concussion: Is it safe to drive after symptoms resolve? J Neurotrauma. 2016 Dec 13. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: pharmacist, thrombolysis, door-to-needle time, acute ischemic stroke (PubMed Search)
Posted: 12/14/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Impact of an ED pharmacist on time to thrombolysis in acute ischemic stroke
Montgomery K, Hall AB, Keriazes G. Impact of an emergency medicine pharmacist on time to thrombolysis in acute ischemic stroke. Am J Emerg Med 2016;34:1997-9.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: subarachnoid hemorrhage, mimic, pseudosubarachnoid hemorrhage, cerebral edema (PubMed Search)
Posted: 11/9/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Patient found pulseless after submersion in water for 20 minutes. After ROSC, patient’s GCS was 3 and pupils are dilated and nonreactive.

Kim JM, Eom TH. The pseudosubarachnoid hemorrhage: clinical implications of subarachnoid hemorrhage misdiagnosis. Pediatr Emerg Care. 2016 May 12. [Epub ahead of print]
Category: Neurology
Keywords: contrast, epidural, multiple sclerosis (PubMed Search)
Posted: 10/26/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Magnetic resonance imaging (MRI) is the method of choice for imaging the spine for the suspicion of non-traumatic disorder, such as multiple sclerosis (MS), transverse myelitis, epidural abscess, spinal cord infarcts, and spondylotic myelopathy (changes in the spinal cord due to disk herniation or osteophytes in degenerative joint disease).
If the differential diagnosis includes infection, neoplasm, demyelination or inflammation, then IV contrast should be administered.
Singh K, Mechtler LL and Klein JP. Imaging of Spinal Cord Disorders. Continuum 2016;22(5):1595 1612
Category: Neurology
Keywords: Brain Trauma Foundation, BTF, guideline, traumatic brain injury, TBI (PubMed Search)
Posted: 10/12/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Updated Guidelines for Traumatic Brain Injury
The Brain Trauma Foundation (BTF) Guidelines for the Management of Severe Traumatic Brian Injury (TBI) was recently updated and published in September 2016.
Updated recommendations include:
For the executive summary and complete guidelines, go to https://braintrauma.org/guidelines/guidelines-for-the-management-of-severe-tbi-4th-ed#/
Category: Neurology
Keywords: lumbar puncture, meningitis, INR, warfarin, spinal, bleeding (PubMed Search)
Posted: 9/28/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
You have a patient in whom you suspect meningitis, but he is on warfarin for a history of pulmonary embolism. You started empirical antibiotics. His INR is 2.6, and you want to do a lumbar puncture (LP) to confirm your diagnosis. Can you use Prothrombin Complex Concentrate to lower his INR and safely perform the LP?
Take Home Point:
Using PCC to lower INR to enable LP is relatively safe and effective in patients on vitamin K antagonists. The dose used was individually determined by the physician according to initial INR.
Limitation:
This is a retrospective study, with no control group. One patient (2.7%) had a myocardial infarction that was “possibly related” to the PCC administration.
In Depth:
This is a retrospective study, with no control group. However, it is the largest study to date that was specifically designed to answer this clinical question, including 37 patients over a 10-year period, with the following results:
- PCC was effective 90% of patients
- The median INR was 2.2 before, and 1.3 after (checked immediately after the infusion)
- The median time from starting the infusion and LP was 135 minutes.
- None of the patients had a spinal hemorrhage or allergic reaction.
- Some patients were started on vitamin K according to the physician’s discretion, with variable starting times of anticoagulation after the procedure (if at all).
Laible M, Beynon C, Sander P, et al. Treatment with Prothrombin Complex Concentrate to Enable Emergency Lumbar Puncture in Patients Receiving Vitamin K Antagonists. Ann Emerg Med. 2016 Sep;68(3):340-4
Category: Neurology
Keywords: eyelid apraxia, eye opening apraxia (PubMed Search)
Posted: 9/14/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Category: Neurology
Keywords: cerebellar disease, tremor, nystagmus (PubMed Search)
Posted: 8/24/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Ataxia is an important clinical sign of cerebellar pathology, but how is it actually described?
Stance ataxia: inability to stand with feet together for more than 30 seconds
Gait ataxia
Sensory ataxia: the first 2 elements, in addition to a positive Romberg sign
Truncal ataxia: oscillation of body while sitting or standing
Limb ataxia: functional impairment in performing actions such as writing or buttoning and improves with slowing down the movement
Dysdiadokinesia: impairment of rapidly alternating movement
Intention tremor: tested by finger-to-nose and heel-to-shin.
Dysmetria: pastpointing or undershooting on finger-chasing or shin-tap.
Dysarthria: irregular and slow speech with unnecessary hesitation
Nystagmus and other ocular disturbances, such as ocular flutter and opsoclonus.
The first 3 are present in both cerebellar pathology and loss of proprioceptive input, the rest are usually due to cerebellar pathology or ataxic syndrome.
Ashizawa T and Xia G. Ataxia. Continuum 2016;22(4):1208-1226
Category: Neurology
Keywords: Uncal herniation, ipsilateral hemiplegia, Kernohan's notch, Kernohan's sign (PubMed Search)
Posted: 8/10/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD

Diagram modified from "Localised Neurological Disease and Its Management A Intracranial". clinicalgate.com/localised-neurological-disease-and-its-management-a-intracranial/. Accessed 10 Aug 2016.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: SAH, headache, LP, CTA (PubMed Search)
Posted: 7/27/2016 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Clinical Guidelines for the Emergency Department Evaluation of Subarachnoid Hemorrhage. Meurer WJ, Walsh B, Vilke GM and Coyne CJ. JEM 2016; 50(4) 696-701
Category: Neurology
Keywords: Large vessel occlusion stroke, endovascular intervention, Field Assessment Stroke Triage for Emergency Destination, FAST-ED, NIHSS, Rapid Arterial Occlusion Evaluation, RACE, Cincinnati Prehospital Stroke Severity scale, CPSS (PubMed Search)
Posted: 7/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
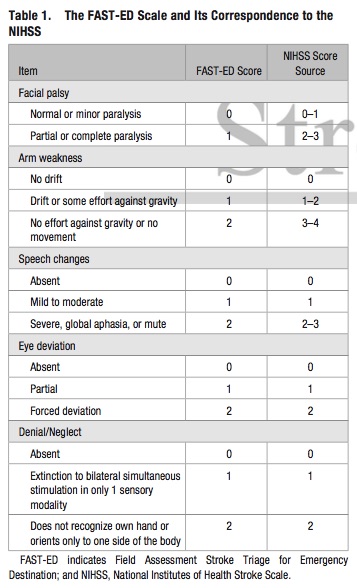
Bottom Line: Additional assessment of gaze deviation, aphasia and neglect, as included in the FAST-ED scale, increases the accuracy of predicting LVOS.
Follow me on Twitter @EM_NCC
