Category: Neurology
Keywords: migraine, headache, opioids, dopamine antagonist (PubMed Search)
Posted: 8/26/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Status migrainosus is a migraine that lasts more than 72 hours, and can be rather challenging to control. A few tips to tackle this are:
1. Adequately hydrate all patients (IV fluids are usually required, especially with severe nausea/vomiting)
2. Establish realistic expectations for the patient. A patient with chronic daily headaches will not be pain-free in the ED.
3. Use IV nonopioid medications for pain control
1st Line:
- Dopamine Antagonists: in increasing efficacy
- Metoclopramide
- Phenothiazines: prochlorperazine, promethazine and chlorpromazine
- Butyrophenones: droperidol and haloperidol
- NSAIDs: such as Ketorolac IV or IM
2nd Line:
- Corticosteroids: Do not treat the migraine in the ED, but prevent headache recurrence within 72 hours.
- Magnesium Sulfate: Has shown mixed efficacy. More likely to have a sustained benefit in patient with serum magnesium level of 1.3mg/dL or less.
- Valrpoic Acid: Be careful of combining it with Topiramate.
- Vasoconstrictors: Triptans, ergotamine, dihydroergotamine. Effective, but use is limited by contraindications.
- Opioids: Last resort
Category: Neurology
Keywords: insular ribbon sign, MCA stroke, early CT sign of stroke (PubMed Search)
Posted: 8/12/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
Neuroimaging Tip - Loss of the Insular Ribbon Sign
Category: Neurology
Keywords: antiplatelet, stroke, MI, Eptifibatide (PubMed Search)
Posted: 7/22/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Given the similarity in pathophysiology, pharmacologic treatments for ischemic stroke have been modeled after those for acute myocardial infarction, such as the use of antiplatelets and thrombolytic agents. Have you ever wondered, why don't we give glycoprotein IIb/IIIa inhibitors (GPIs) as well?
A Cochrane review answers this question; GPIs increase morbidity in acute ischemic stroke (in the form of intracranial hemorrhage), with no evidence of benefit (improvement in Rankin Scale).
The systematic review looked at randomized clinical trials of GPIs in patients with ischemic stroke of 6 hours or less, alone or in combination with thrombolytics.
Ciccone A, Motto C, Abraha I, et al. Glycoprotein IIb/IIIa Inhibitors for Acute Ischaemic Stroke. Cochrane Database Syst Rev. 2014;3
Category: Neurology
Keywords: CSF shunts, VP shunt, VA shunt, LP shunt (PubMed Search)
Posted: 7/8/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Cerebrospinal Fluid (CSF) Shunts
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: psych, conversion, nonorganic, physical exam (PubMed Search)
Posted: 6/25/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Stone J, Carson A. Functional Neurologic Disorders. Continuum 2015;21(3):818 837
Category: Neurology
Keywords: Guidelines, intracerebral hemorrhage, ICH score, communication (PubMed Search)
Posted: 6/10/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
What is the ICH Score?
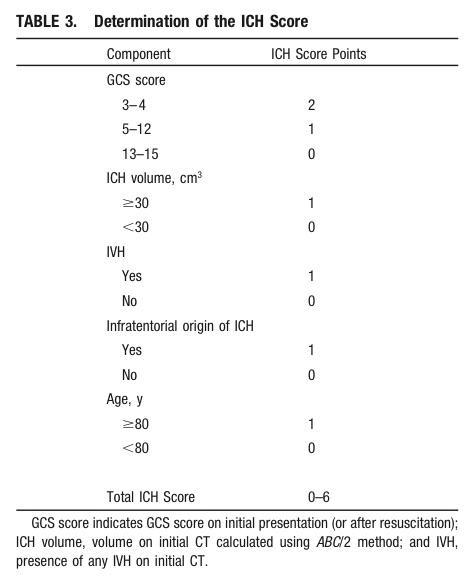
Take Home Point: Communicate the severity of your ICH patient by using either the composite ICH Score or by including details such as the patient's GCS, estimated volume of ICH, presence of IVH, and supra- vs. infratentorial origin.
1) Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015 May 28. [Epub ahead of print]
2) Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32(4):891-897.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: lumbar puncture, LP, obesity (PubMed Search)
Posted: 5/27/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
We all dread performing lumbar punctures on the obese patient. The traditional standard length spinal needle (9 cm) is becoming increasingly inadequate in reaching the subdural space in our overweight society.
Abe et al developed a formula for selecting the proper needle length to reach the middle of the spinal canal from the skin using retrospective CT data from 178 patients.
Length of needle (cm) = 1+ 17 x Weight (kg)/ Height (cm)
Given the average height of the American woman (163 cm or 5’4’’) our standard length spinal needle will FAIL to reach the mid-thecal space if a woman weighs more than 170 lb (75 kg)!!!
Paul Blart Mall Cop, and King of Queens star Kevin James (5’8’’, 285 lb) would require a 13.7 cm spinal needle. This means even our long spinal needles (12.7 cm) would FAIL by 1 cm.
Note that this formula resulted in selection of needles too small (6%) and too long (31%) of the time. Abe’s linear correlation had an R value of 0.81, (p<.001)
Bottom-Line: Consider use of a long spinal needle (12.7 cm) or IR guided LP in overweight /obese patients and the above formula to guide your depth of insertion
Category: Neurology
Keywords: Glasgow Coma Scale, GCS, traumatic brain injury, TBI, survey (PubMed Search)
Posted: 5/13/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Are We Using the Glasgow Coma Scale Reliably?
| Reported by Responders | |
| Patient population in which GCS is used | Traumatic brain injury (96%) Other neurological disorders (78%) |
| Intended purpose of GCS | Classification of severity of injury (51%) Serial evaluation of patient over time (33%) Clinical decision making (44%) Prognostication (17%) |
| Application of stimulus | Both arms and legs (62%) Only arms (37%) |
| Type of stimuli used | Nail bed pressure (57%) Lateral side of finger (22%) Supra-orbital nerve pressure (52%) Trapezius or pectoralis pinch (50%) Sternal rub (53%) Retromandibular stimulation (24%) Earlobe stimulation (16%) |
| Reporting of GCS | Description in words, e.g. no eye opening, no motor (19%) Numerical report, e.g. E1V1M1 (46%) Sum score, e.g. EVM=3 (35%) |
Bottom line: There are variations in the application, assessment, and reporting of the GCS. A standardized approach is needed for it to be a reliable assessment and communication tool.
Reith FCM, Brennan PM, Maas AIR, Teasdale GM. Lack of standardization in the use of the Glasgow Coma Scale: Results of international surveys. J Neurotrauma. 2015; May 7. [Epub ahead of print]
Category: Neurology
Keywords: tumor, seizure, stroke (PubMed Search)
Posted: 4/23/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Some medical issues arise in patients with brain tumors:
// Steroids are used to decrease vasogenic edema, especially preop or during radiation therapy. Patients are ideally gradually weaned off steroids. Dexamethasone is most commonly used. 1-2% of patients are at risk for adrenal suppression.
// Infections: Post-op wound infections can be delayed up to months, especially in patients on steroids.
// Antiepileptics: Although technically not recommended in patients with brain tumors who have not had seizures (American Academy of Neurology 2010), many surgeons continue to prescribe antiepileptics preoperatively and then discontinue them by 1 month postop if the patients remain seizure-free. Levetiracetam is emerging as the drug of choice due to favorable side effect profile.
// Thromboembolism: Brain tumors are considered very high risk for venous thromboembolism. Low-molecular-weight heparin is the treatment of choice, with warfarin being an acceptable substitute.
// Arterial thrombosis and ischemic stroke: Risk is increased with certain medications, and thrombolysis is contraindicated.
Pruitt AA. Medical Management of Patients with Brain Tumors. Continuum 2015;21(2):314 331
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH score, prognostication, early decisions to limit medical treatment (PubMed Search)
Posted: 4/8/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
Prognostication in intracerebral hemorrhage - A self-fulfilling prophecy?
The ICH Score is a validated outcome prediction model for intracerebral hemorrhage (ICH) developed from clinical and neuroimaging characteristics on presentation.
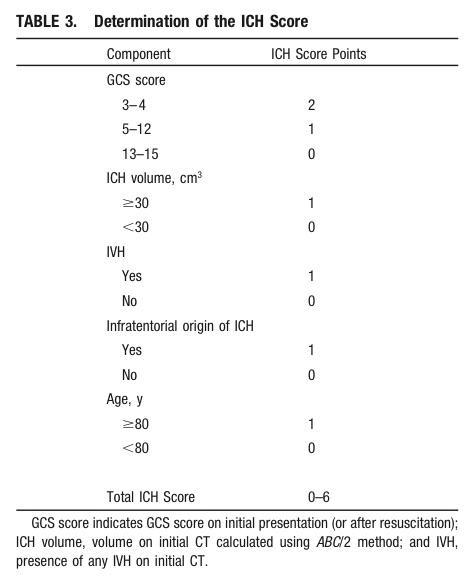
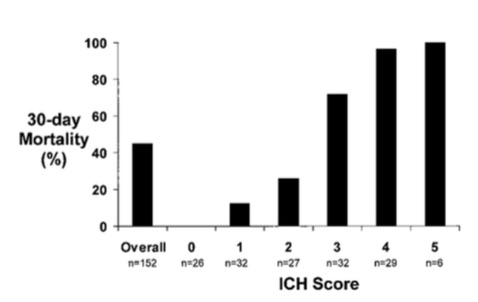
While predictive models are often used in clinical care for prognostication, is it a self-fulfilling prophecy to make early decisions to limit medical treatments based on these models?
Morgenstern et al. conducted an observational study across 5 hospitals looking at 30-day mortality of patients with ICH with initial GCS <12 who received full medical care for at least 5-days following symptom onset.
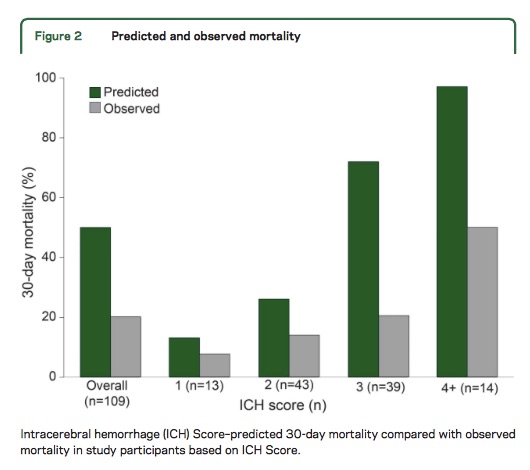
Take Home Point: The ICH Score is a useful tool for stratifying patient severity, but one should be cautious in using the model to provide specific numerical values as outcome predictions.
Hemphill JC, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score. A simple, reliable grading scale for intracerebral hemorrhage. Stroke 2001;32:891-897.
Morgenstern LB, Zahuranec DB, Sanchez, BN, et al. Full medical support for intracerebral hemorrhage. Neurology 2015;84:1-6.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: spinal cord, numbness, herpes, CSF (PubMed Search)
Posted: 3/25/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Elsberg syndrome is sacral radiculitis caused by a viral infection, most commonly herpes simplex virus type 2 (HSV-2) - whether a primary infection or a reactivation. The typical patient is a young sexually active woman presenting wtih acute transient urinary retention and sensory lumbosacral symptoms, such as dull pain in anorectal region, paresthesias, loss of sensation or flaccid paresis of leg muscles. Patients can also have constipation or erectile dysfunction.
The presence of inguinal lymphadenopathy and/or anogenital rash can be important clues but are not necessary for diagnosis. CSF may show mild to moderate pleocytosis, with a mild elevation in proteins. Herpes PCR in the CSF may be positive as well. The MRI may show varying degrees of root or lower spinal cord edema with hyperintensity of T2-weighted images.
In immunocompetent patient, the disease usually self limiting, usually resolving in 4-10 days, but can be progressive and ascending in patients with immunocompromise, such as HIV or cancer. Antiviral treatment may shorten the duration of illness in cases with confirmed herpes, either oral or IV.
Eberhardt O, K ker W, Dichgans J, Weller M. HSV-2 sacral radiculitis (Elsberg syndrome). Neurology 63(4), 24 August 2004, 758-759
Category: Neurology
Keywords: back pain, spinal cord (PubMed Search)
Posted: 3/12/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Cauda Equina Syndrome is a true neurologic and surgical emergency. Unfortunately, no constellation of symptoms or exam findings is 100% sensitive. In fact, no single symptoms predicts the radiographic finding of cauda equina syndrome with an accuracy greater than 65%.
The most common symptoms are sciatica (96%), micturition dysfunction (89%), saddle anesthesia or hypoethesia (81%) and defecation dysfunction (47%).
Tarulli AW. Disorders of the Cauda Equina. Continuum Lifelong Learning Neurol 2015;21(1):146 158
Category: Neurology
Keywords: cardiac arrest, subarachnoid hemorrhage, intracerebral hemorrhage, ischemic stroke, seizure (PubMed Search)
Posted: 2/25/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Neurologic causes of cardiac arrest have not been well described. Two recent retrospective studies looked at the epidemiology and clinical features of these patients.
Hubner P. et al.
Arnaout M. et al.
Neurologic causes of cardiac arrest are uncommon presentations that may be difficult to distinguish from cardiac etiology of cardiac arrest. If history and clinical presentation suggests a neurologic cause, obtain a non-contrast head CT for evaluation.
Hubner P, Meron G, Kurkciyan I, et al. Neurologic causes of cardiac arrest and outcomes. J Emerg Med. 2014;47(6):660-667.
Arnaout M, Mongardon N, Deye N, et al. Out-of-Hospital Cardiac Arrest from Brain Cause: Epidemiology, Clinical features, and Outcome in a Multicenter Cohort. Crit Care Med. 2015;43(2):453-460.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: acute ischemic stroke, magnesium, neuroprotectant, IMAGES, FAST-MAG (PubMed Search)
Posted: 2/12/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Magnesium, another failed neuroprotectant?
Stroke is a leading cause of adult disability and the second leading cause of death worldwide. Currently available therapies for acute ischemic stroke are based on restoring perfusion to the ischemic penumbra. However, they are only moderately effective.
A series of pathological cascades leading to neuronal death are triggered in acute ischemia. Thus it may be logical to suggest that if one can interrupt the propagation of these cascades, perhaps part of the brain tissue can be protected and salvaged.
Magnesium has been shown in various animal models to have pluripotent neuroprotective properties. It is also widely available, simple to administer, and has a favorable risk profile. A prior study of magnesium in acute ischemic stroke (IMAGES) did not show a benefit when the agent was administered a median 7.4 hours after symptom onset. However, a subgroup of patients treated within 3 hours of symptom onset showed possible benefit.
The Field Administration of Stroke Therapy - Magnesium (FAST-MAG) trial, funded by the NIH, looked at magnesium administered within 2 hours after symptom onset on the degree of disability at 90 days after stroke as measured by the modified Rankin scale.
Magnesium was not found to have any benefit in functional outcome at 90 days.
This study was unique in several ways:
However, despite this study being very well executed, demonstrating the feasibility of conducting a phase 3 trial with targeted intervention within the hyperacute window, it is another neuroprotective agent that failed to translate from the laboratory bench to the clinical realm.
Potential explanations for the discrepancies between preclinical and clinical outcomes of neuroprotective agents thus far include discrepancies on outcome measures, functional assessments, pre-morbid conditions, therapeutic windows, and drug-dosing schedules between animal studies and clinical trials.
Take Home Point: Magnesium does not have any clear benefit in acute ischemic stroke at this time.
Muir KW, Lees KR, Ford I, et al. Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): a randomised controlled trial. Lancet. 2004;363(9407):439-445.
Saver JL, Starkman S, Eckstein M, et al. Prehospital use of magnesium as neuroprotection in acute stroke. N Engl J Med. 2015;372(6):528-536.
Cheng YD, Al-Khoury L, Zivin JA. Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx. 2004;1(1):36-45.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Myasthenia gravis, myopathy, iatrogenic (PubMed Search)
Posted: 1/29/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Patients with myasthenia gravis (MG) may be seen in the emergency department for symptoms that are not related to their MG, such as an upper respiratory tract infection or chest pain, for example.
The emergency physician should be careful in prescribing new medications to patients with MG, as that can precipitate a myasthenic crisis (and therefore cause significant morbidity and mortality). Below is a list of medications that are commonly implicated; an extensive list can be found on www.myasthenia.org/docs/MGFA_medicationsandmg.pdf)
Sanders DB, Guptill JT. Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome. Continuum. 2014 Oct;20(5)
Category: Neurology
Keywords: traumatic brain injury, progesterone, neuroprotectant, clinical trials, PROTECT III, SYNAPSE (PubMed Search)
Posted: 1/14/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Is progesterone yet another disappointing neuroprotectant?
Traumatic brain injury (TBI) affects more than 1.7 million persons in the U.S. annually. The incidence of TBI is increasing globally, especially in developing countries. Despite improvement in trauma systems and critical care, the morbidity and mortality associated with severe TBI remain high.
Progesterone has been shown in preclinical and phase 2 randomized clinical trials to have pluripotent neuroprotective properties and improve mortality in TBI.
Two multicenter phase 3 trials were recently completed and published in the December 25th issue of the New England Journal of Medicine. However, their results were disappointing.
Both studies used the Glasgow Outcome Scale (GOS) or Extended Glasgow Outcome Scale (GOS-E) at 6 months as their primary outcome. The GOS and GOS-E capture the degree of recovery from brain injury in terms of disability, stratified into levels by death, vegetative state, severe disability, moderate disability, and good recovery.
Progesterone was not found to have any benefit in functional outcome at 6 months.
Both of these studies were well designed and conducted. However, they were based on small effect sizes of the phase 2 trials. In addition, they had very favorable outcome rates in the placebo group, thereby making it hard to demonstrate a benefit by their sample sizes.
There has been a long history of failed neuroprotectant trials likely due to the complex and variable injury mechanisms involved in TBI. The currently available outcome measures are also insensitive to the targeted mechanistic endpoints. More research is needed to understand not only potential therapies but also how to select appropriate patients for these therapies.
Take Home Point: Progesterone does not have any clear benefit in TBI at this time.
Wright DW, Yeatts SD, Silbergleit R, et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371(26):2457-2466.
Skolnick BE, Maas AI, Narayan RK, et al. A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med. 2014;371(26):2467-2476.
Category: Neurology
Keywords: delirium, geriatric, elderly, pitfall (PubMed Search)
Posted: 12/25/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Delirium has long been recognized as a common disorder of the geriatric ED population (seen in up to 20% of patients above the age of 65 years), but how good are we at detecting it?
Studies show that the diagnosis of delirium is made in the ED in only 11-46% of patients, which means that more than half go undiagnosed. The problem is, the risk of death at 3 months increases by 11% for every 48 hours of delirium the patient experiences, and so does their length of stay and functional decline. It is mostly missed in patients who have a baseline cognitive dysfunction, such as dementia.
So what can we do about that?
Treat delirium as a neurolgical emergency; be vigilant about diagnosing it and treating it. There are a lot of neurocognitive tests that can be used for diagnosis (such as the mini-mental status exam), but they are usually too cumbersome to use in an ED setting. The CAM (Confusion Assessment Method) has been extensively studied and has a sensitivity and specifity of about 95% to diagnose delirium. It includes the acuity of onset, fluctuant course, inattention (the hallmark), disorganized thinking and/or altered level of consciousness.
Bottom Line? Don't forget to screen your elderly patients for delirium and treat them accordingly!
1. Wilber ST, Han JH. Altered Mental Status in the Elderly. Geriatric Emergency Medicine Principles and Practice. Edited by Kahn JH, Maguaran Jr BG, Olshaker JS. New York: Cambridge University Press; 2014: 102-113
2. Barron EA, Holmes J. Delirium within the emergency Care setting, occurence and detection: a systematic review. EMJ 2013; 30(4) 263-268
3. Wei LA, BA, Fearing MA et al. The Confusion Assessment Method: A Systematic Review of Current Usage J Am Geriatr Soc 56:823 830, 2008
Category: Neurology
Keywords: clinical decision support, clinical decision rules, head CT, mild traumatic brain injury (PubMed Search)
Posted: 12/10/2014 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Does clinical decision support help reduce head CT utilization in mild traumatic brain injury related ED visits?
Are we utilizing clinical decision rules adequately to help us appropriately select patients for CT imaging?
Can clinical decision support (CDS) help us reduce head CT utilization in mTBI related ED visits?
Take Home Point:
Clinical decision support may be a useful tool to help reduce CT utilization in mild TBI related ED visits.
Ip IK, Raja AS, Gupta A, et al. Impact of clinical decision support on head CT use in patients with mild traumatic brain injury in the emergency department. Am J Emerg Med 2014; Nov 13 [epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: pseudotumor cerebri, visual loss, shunt (PubMed Search)
Posted: 11/27/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
There are a few available options for treatment of visual loss due to idiopathic intracranial hypertension (IIH). The Idiopathic Intracranial Hypertension Treatment Trial (IIHTT), the first randomized, prospective, placebo-controlled trial for the treatment of patients with visual loss from IIH, which results were published earlier this year, provided substantial evidence for the first 2 options.
1. Weight loss
2. Carbonic anhydrase inhibitors, such as Acetazolamide
3. Therapeutic lumbar puncture (reserved for pregnant patients or for occasional flare-ups)
4. Surgery:
a. Optic nerve sheath fenestration (ONSF): visual acuity and fields improve in most cases, but symptoms may recur. Benefit? No hardware!
b. Shunts: ventriculoperitoneal (VP) and lumboperitoneal (LP) shunts are the most frequently used. No clear benefit for one over the other. VP shunts may be programmable.
c. Cerebral venous stenting: endovascular stenting of the transverse sinus may improve the symptoms in some people.
BONUS PEARL: The headache does not correlate with the lumbar opening pressure, degree of papilledema or amount of visual loss. None of the above-mentioned management strategies is meant for the treatment of the headache alone. For that, medical management with standard symptomatic treatments, avoiding opiates and barbiturates, is recommended. Surgery is not recommended for headache alone.
Friedman DI. Papilledema and idiopathic intracranial hypertension. Continuum. 2014 Aug;20(4 Neuro-ophthalmology)
Category: Neurology
Keywords: anisocoria, Horner syndrome, third nerve palsy, tonic pupil (PubMed Search)
Posted: 11/12/2014 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Anisocoria, or unequal pupil sizes, is a common condition. Approximately 20% of the normal population have physiologic anisocoria. However, pathologic anisocoria indicates disease of the iris, parasympathetic pathway or sympathetic pathway. A systematic approach to the evaluation of anisocoria can help differentiate between etiologies that range from benign to life threatening.
The most important question in the evaluation of anisocoria is whether both pupils are normally reactive to light or is one (or both) poorly reactive. If both pupils are reactive, the smaller pupil is abnormal and the lesion is likely in the sympathetic pathway because pupillary constriction (parasympathetic pathway) is intact. If one pupil is poorly or non-reactive (and there is no relative afferent pupillary defect), the larger pupil is abnormal and the lesion is likely in the parasympathetic pathway.
DDx of anisocoria with normally reactive pupils:
DDx of anisocoria with poorly or non-reactive pupil:
Kedar S, Biousse V, Newman NJ. Approach to the patient with anisocoria. In: UpToDate, Brazis, PW (Ed), UpToDate, Waltham, MA, 2014. (Accessed on November 12, 2014.)
Lam BL, Thompson HS, Corbett JJ. The prevalence of simple anisocoria. Am J Ophthalmol 1987;104(1):69-73.
