Category: Critical Care
Keywords: Hyponatremia (PubMed Search)
Posted: 11/12/2020 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Baek SH, Jo YH, Ahn S, et al. Risk of overcorrection in rapid intermittent bolus vs slow continuous infusion therapies of hypertonic saline for patients with symptomatic hyponatremia: the salsa randomized clinical trial. JAMA Intern Med. Published online October 26, 2020.
Category: Critical Care
Keywords: airway management, cardiac arrest, COVID-10, SARS-CoV-2, cardiopulmonary resuscitation, CPR (PubMed Search)
Posted: 11/3/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
As the number of COVID-19 cases rises worldwide, prehospital and emergency department healthcare workers remain at high risk of exposure and infection during CPR for patients with cardiac arrest and potential SARS-CoV-2.
Existing evidence supports similar cardiac arrest outcomes in airways managed with a supraglottic airway (SGA) compared to endotracheal intubation (ETT).1 It is generally accepted that the best airway seal is provided with endotracheal intubation + viral filter, but how well do SGAs prevent spread of aerosols?
In CPR simulation studies:
Category: Critical Care
Keywords: NAC, Liver Failure, n-acetylcysteine (PubMed Search)
Posted: 10/20/2020 by Mark Sutherland, MD
(Updated: 2/1/2026)
Click here to contact Mark Sutherland, MD
N-acetylcysteine (NAC) is well known as the accepted antidote for acute acetaminophen (tylenol/paracetamol) overdose and is well studied for this indication. While the literature base is not nearly as strong in other causes of acute liver failure, NAC is increasingly used in these scenarios as well. In the emergency department in particular, the cause of fulminant hepatic failure is often not known. NAC may have some protective benefit in non-acetaminophen acute liver failure. Existing data do not show a mortality benefit to NAC in non-acetaminophen acute liver failure, but do show improvement in transplant-free survival. The AASLD guidelines (last revised in 2011) do not comment on NAC in non-acetaminophen acute liver failure. A common practice is to continue NAC until the INR is < 2 and AST/ALT have decreased at least 25% from their peak values.
Patients in fulminant liver failure should also be strongly considered for transfer to a center that does liver transplant, if presenting to a non-transplant center. The King's College criteria is the most commonly used prognostic score for determining need of transfer to a transplant center, but in addition to calculating a King's College score providers should generally consider consultation with a transplant hepatologist for any fulminant liver failure patient to discuss the risks/benefits of transfer for transplant evaluation.
Bottom Line: While not as strongly indicated as it is in acute acetaminophen induced liver failure, NAC should be considered in both non-acetaminophen liver failure and liver failure of unknown etiology. In addition, strongly consider consultation with a transplant hepatologist in any case of fulminant hepatic failure.
Teriaky A. The role of N-acetylcysteine in the treatment of non-acetaminophen acute liver failure. Saudi J Gastroenterol. 2017;23(3):131-132.
October 2020 EMRAP: Critical Care Mailbag
MDCalc King's College Criteria: https://www.mdcalc.com/kings-college-criteria-acetaminophen-toxicity
Category: Critical Care
Posted: 10/13/2020 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Blood Pressure Management in Acute Ischemic Stroke
Herpich F, et al. Management of acute ischemic stroke. Crit Care Med. 2020; 48(11):1654-1663.
Category: Critical Care
Keywords: Cardiac arrest, transport, EMS (PubMed Search)
Posted: 9/29/2020 by Lindsay Ritter, MD
Click here to contact Lindsay Ritter, MD
Historically, there has been debate on transporting outside hospital cardiac arrests, as well a trauma, with the question of whether to "scoop and run" or "stay and play".
Could hasty transportation of cardiac arrest patients put a damper on resuscitation quality?
A recent propensity-matched study in JAMA analyzed 192 EMS agencies across 10 N American sites.
Methods:
-Resuscitation Outcomes Consortium Cardiac Epidemiologic Registry, which counted 43,969 consecutive cases of nontraumatic adult EMS-treated OHCA (median age 67, 37% of whom were women) in 2011-2015.
-25% of these patients were transported to the hospital
-Matched 1:1 with patients in refractory arrest who were resuscitated on scene
-Primary outcome was survival to hospital discharge, secondary outcome survival to hospital discharge with a favorable neurological status
Results:
-Duration of out-of-hospital resuscitation was only 6 minutes longer in the intra-arrest transport group (29.1 and 22.9 minutes; not a statistically significant difference)
-Survival to hospital discharge was 3.8% for patients who underwent intra-arrest transport and 12.6% for those who received on-scene resuscitation
-In the propensity-matched cohort, which included 27,705 patients, survival to hospital discharge occurred in 4.0% of patients who underwent intra-arrest transport vs 8.5% who received on-scene resuscitation (risk difference, 4.6% [95% CI, 4.0- 5.1])
-Favorable neurological outcome occurred in 2.9% of patients who underwent intra-arrest transport vs 7.1% who received on-scene resuscitation (risk difference, 4.2% [95% CI, 3.5%-4.9%])
-Intra-arrest transport during resuscitation was associated with worse odds of survival to hospital discharge compared to on-scene resuscitation (4% vs 8.5%, RR 0.48, CI 0.43-0.54)
-Findings persisted across subgroups of initial shockable rhythm vs. non-shockable rhythms (most common initial rhythm was aystole), as well as EMS witness arrests vs. unwitnessed arrests
Conclusion:
-This study does not support the routine transportation of patients in cardiac arrest during rescuscitation.
-The neurologically intact survival benefit associated with on-scene resuscitation is both impressive and intriguing.
-However, what implications could this have on ECPR?
Limitations:
-Potential bias due to observational nature of study
-Duration of resuscitations very similar, unknown exactly how long transport times were or if this was in urban or rural populations
-External validity not generalizable due to heterogeneity of patient populations and EMS systems
-Further randomized clinical trials are required
Grunau B, Kime N, Leroux B, et al. Association of Intra-arrest Transport vs Continued On-Scene Resuscitation With Survival to Hospital Discharge Among Patients With Out-of-Hospital Cardiac Arrest. JAMA. 2020;324(11):1058–1067. doi:10.1001/jama.2020.14185
Category: Critical Care
Keywords: IPH, blood pressure management, outcome (PubMed Search)
Posted: 9/22/2020 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
A retrospective study analyzed data from 757 patients with spontaneous intraparenchymal hemorrhage.
Within the first 6 hours of admission, patients who had systolic blood pressure reduction between 40 – 60 mm Hg (OR 1.9, 95% CI 1.1-3.5) or reduction ≥ 60 mm Hg (OR 1.9, 95%CI 1.01-3.8) were associated with almost double likelihood of poor discharge functional outcome (defined as modified Rankin Scale 3-6).
Additionally, large systolic blood pressure reduction ≥ 60 mm Hg in patients with large hematoma (≥ 30.47 ml) was associated with higher likelihood of very poor functional outcome (mRS 5-6).
Take home points: while more studies are still needed to confirm these observations, perhaps we may not want to drop blood pressure in patients with spontaneous intraparenchymal hemorrhage too much and too fast.
The Magnitude of Blood Pressure Reduction Predicts Poor In-Hospital Outcome in Acute Intracerebral Hemorrhage.
Afshin A Divani, Xi Liu, Alexander Petersen, Simona Lattanzi, Craig S Anderson, Wendy Ziai, Michel T Torbey, Tom J Moullaali, Michael L James, Alibay Jafarli, Stephan A Mayer, Jose I Suarez, J Claude Hemphill, Mario Di Napoli.
Neurocrit Care. 2020 Oct;33(2):389-398. doi: 10.1007/s12028-020-01016-z.
Category: Critical Care
Posted: 9/18/2020 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Systematic review and meta-analysis of 5 studies with a total of 929 patients comparing early vs. late initiation of norepinephrine in patients with septic shock
Primary outcome:
Secondary outcome:
Caveat:
Take home point:
Early norepinephrine usage may improve mortality in septic shock
Li Y, Li H, Zhang D. Timing of norepinephrine initiation in patients with septic shock: a systematic review and meta-analysis. Crit Care. 2020;24(1):488.
Category: Critical Care
Keywords: resuscitation, ultrasound, VExUS, venous congestion (PubMed Search)
Posted: 9/8/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
While the invasive monitoring of central venous pressure (CVP) in the critically ill septic patient has gone the way of also transfusing them to a hemoglobin of 10 mg/dL, it remains that an elevated CVP is associated with higher mortality1,2 and renal failure.2,3
Extrapolating from existing data looking at hepatic vein, portal vein, and renal vein pulsatility as measures of systemic venous hypertension and congestion,4,5,6 Beaubien-Souligny et al. developed the venous excess ultrasound (VExUS) grading system incorporating assessment of all 3, plus the IVC, using US to stage severity of venous congestion in post-cardiac surgery patients.7 They evaluated several variations, determining that the VExUS-C grading system was most predictive of subsequent renal dysfunction.
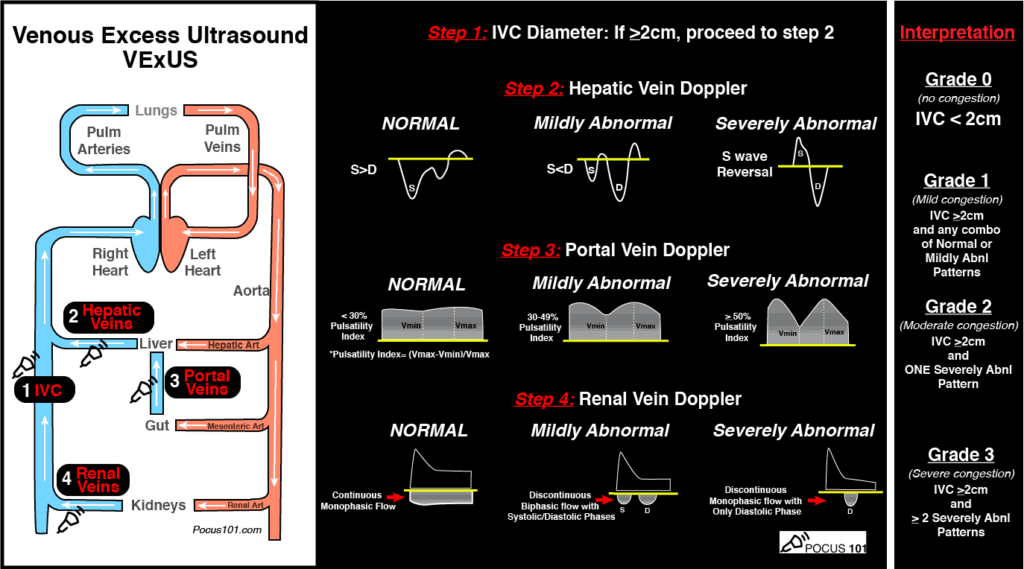
(Image from www.pocus101.com)
High Points
VExUS Grade 3 (severe) venous congestion:
Caveats
Clinical Uses
A great how-to can be found here:
https://www.pocus101.com/vexus-ultrasound-score-fluid-overload-and-venous-congestion-assessment/
1. Li DK, Wang XT, Liu DW. Association between elevated central venous pressure and outcomes in critically ill patients. Ann Intensive Care. 2017;7(1):83. doi:10.1186/s13613-017-0306-1
2. Chen KP, Cavender S, Lee J, et al. Peripheral Edema, Central Venous Pressure, and Risk of AKI in Critical Illness. Clin J Am Soc Nephrol. 2016;11(4):602-608.
3. Chen CY, Zhou Y, Wang P, Qi EY, Gu WJ. Elevated central venous pressure is associated with increased mortality and acute kidney injury in critically ill patients: a meta-analysis. Crit Care. 2020;24(1):80. doi:10.1186/s13054-020-2770-5
4. Iida N, Seo Y, Sai S, et al. Clinical Implications of Intrarenal Hemodynamic Evaluation by Doppler Ultrasonography in Heart Failure. JACC Heart Fail. 2016;4(8):674-682. doi:10.1016/j.jchf.2016.03.016
5. Ikeda Y, Ishii S, Yazaki M, et al. Portal congestion and intestinal edema in hospitalized patients with heart failure. Heart Vessels. 2018;33(7):740-751. doi:10.1007/s00380-018-1117-5.
6. Beaubien-Souligny W, Benkreira A, Robillard P, et al. Alterations in Portal Vein Flow and Intrarenal Venous Flow Are Associated With Acute Kidney Injury After Cardiac Surgery: A Prospective Observational Cohort Study. J Am Heart Assoc. 2018;7(19):e009961. doi:10.1161/JAHA.118.009961
7. Beaubien-Souligny W, Rola P, Haycock K, et al. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12(1):16. doi:10.1186/s13089-020-00163-w
Category: Critical Care
Keywords: Renal Replacement Therapy (PubMed Search)
Posted: 9/1/2020 by Kim Boswell, MD
(Updated: 2/1/2026)
Click here to contact Kim Boswell, MD
STARRT-AKITrial
The Standard versus Accelerated initiation of Renal Replacement Therapy in Acute Kidney Injury
The development of acute kidney injury (AKI) in the critical care setting portends a greater morbidity and mortality for patients. Additionally, it places the patient at high risk of complications and requires a greater use of resources. Several studies in the past have examined if the timing of initiation of renal replacement therapy (RRT) would result in a mortality benefit, but have failed to demonstrate consistent outcomes.
The STARRT-AKI trial was a multinational, randomized controlled trial designed to determine if early initiation of RRT in critically ill adult patients with AKI lowered the risk of 90-day mortality. The Kidney Disease Improving Global Outcomes (KDIGO) classification was used to define AKI and over 2900 patients were randomly assigned to two groups over a 4 year period. Exclusion criteria included: recent RRT, a renal transplant within the preceding year, advanced CKD, an overdose necessitating RRT, or a strong suspicion of obstruction or autoimmune/vascular cause of their AKI.
Groups:
Outcomes/Results:
Take home points:
Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. STARRT-AKI Investigators; Canadian Critical Care Trials Group, the Australian and New Zealand Intensive Care Society Clinical Trials Group, the United Kingdom Critical Care Research Group, the Canadian Nephrology Trials Network, and the Irish Critical Care Trials Group, Bagshaw SM, Wald R, Adhikari NKJ, et al. N Engl J Med. 2020 Jul 16;383(3):240-251.
Category: Critical Care
Posted: 8/25/2020 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Ketamine In the Critically Ill Patient
Hurth KP, et al. The reemergence of ketamine for treatment in critically ill adults. Crit Care Med. 2020; 48:899-911.
Category: Critical Care
Keywords: COVID-19, ARDS, Pneumonia, Steroids (PubMed Search)
Posted: 8/17/2020 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Another week, another COVID-19 study...
On August 12th, the Metcovid study was e-published ahead of print in Clinical Infectious Diseases. This was another study looking at steroids in COVID-19 pneumonia, this time performed in Brazil. Metcovid was a parallel, double-blind, randomized, placebo-controlled phase IIb clinical trial which enrolled 416 patients at a single academic center for the evaluation of methylprednisolone (MP; 0.5 mg/kg BID x 5 days) vs placebo. As with all COVID studies, Metcovid has some significant limitations, and some equivocal findings. However, Metcovid was largely in line with RECOVERY and other trials looking at steroids in COVID-19, which lends it some face validity. Metcovid found no significant difference in the primary outcome (mortality at day 28), but did find a difference in mortality in patients over 60 years old (a post-hoc analysis). Metcovid was probably underpowered (sample size was based on a 50% reduction in mortality), and did have a very small trend towards reduced mortality in the MP group (37.1% vs 38.2%, p=0.629).
Bottom Line:
Category: Critical Care
Keywords: gastrointestinal bleeding, TXA (PubMed Search)
Posted: 7/30/2020 by Lindsay Ritter, MD
(Updated: 8/4/2020)
Click here to contact Lindsay Ritter, MD
Prior to this study, a Cochrane review and meta-analysis of TXA for upper GI bleeds with 7 trials (1654 patients), showed a large reduction in mortality with TXA (RR 0.61, 95% CI 0.42-0.98, p=0.01)
Design:
-Randomized, international, multicentre, placebo-controlled trial at 164 hospitals in 15 countries Juy 2013-2019
->16/18 years old with upper or lower GI bleeding
-1 g TXA IV over 10 minutes followed by maintenance dose 3 g TXA over 24 hours
Results:
-Main outcome death due to bleeding within 5 days
-4% (222/5994) died in TXA group vs 4% (226/5981) placebo risk ratio RR 0.99, 95% CI 0.82-1.18
-Arterial thromboembolic events MI/CVA similar in both groups (0.7% vs 0.8%)
-Venous thromboembolic events PE/DVT higher in TXA group (0.8% vs 0.4%)
Pitfalls:
-Initially calculated all cause mortality until realization that over half deaths were due to non-bleeding causes, changed to death related to bleeding, allowing study appropriate power to detect difference
-Majority of patients had UGIB/variceal bleeding due to liver disease, over 75% deaths in those with liver disease
-Only 16% patients randomized in <3 hours, most >8 hours (CRASH-2 trial found benefit TXA in trauma patients only <3 hrs to administration)
Takeaway:
-TXA should not be used in the management of GI bleeds
-Increased venous thromboembolic events associated with TXA administration for GI bleeds
HALT-IT Trial Collaborators. Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT-IT): an international randomised, double-blind, placebo-controlled trial. Lancet. 2020;395(10241):1927-1936. doi:10.1016/S0140-6736(20)30848-5
Gluud LL, Klingenberg SL, Langholz E. Tranexamic acid for upper gastrointestinal bleeding. Cochrane Database Syst Rev. 2012;1
Category: Critical Care
Keywords: albumin, crystalloids, sepsis (PubMed Search)
Posted: 7/25/2020 by Quincy Tran, MD, PhD
(Updated: 7/28/2020)
Click here to contact Quincy Tran, MD, PhD
Patient
Single Center, double-blinded, randomized trial.
Patients with cancer and septic shock
Intervention
4% albumin + lactate ringer bolus in 10 minutes
180 patients
Comparison:
Lactate ringer bolus in 10 minutes
180 patients
Outcome:
Primary: Any mortality within 7 days of randomization.
Secondary: Mortality within 28 days, renal replacement therapy (RRT)
Results:
7-day mortality: 46 (25%) for LR + albumin vs. 40 (22%) for LR only
28-day mortality: 96 (53%) for LR + albumin vs. 83 (46%) for LR only
RRT: 16 (9%) for LR + albumin vs. 12 (7) for LR only
Conclusion:
Adding albumin for early resuscitation to crystalloids did not improve mortality in cancer patients with septic shock.
Lactated Ringer's Versus 4% Albumin on Lactated Ringer's in Early Sepsis Therapy in Cancer Patients: A Pilot Single-Center Randomized Trial.
Crit. Care Med. 2019 Oct;47(10):e798-e805.
Category: Critical Care
Posted: 7/21/2020 by Caleb Chan, MD
(Updated: 2/1/2026)
Click here to contact Caleb Chan, MD
Design
-Two-center prospective observational study with 157 patients admitted to the ICU for pneumonia and being treated with HFNC
-ROX (Respiratory rate-OXygenation) index = ratio of SpO2/FIO2 to RR
Results:
-ROX index ≥4.88 at 12 hours after HFNC onset with a sensitivity of 70.1%, a specificity of 72.4%, PPV of 89.4%, NPV of 42%, LR+ of 2.54, and LR- of 0.41 in predicting treatment failure
Validation study: Roca, 2019
-results similar, but ROX index ≥4.88 at 12 hour with LR+ of only 1.82
-also found that a ROX index of <3.85 at 12 hours had a sensitivity of 23.5%, specificity of 98.4%, PPV of 88.9, NPV 69.9, LR+ of 14.47, and LR- 0.78
Pitfalls:
-decision to intubate was not made based on ROX index
-criteria for intubation was also part of the ROX index
-NIV was not part of their treatment algorithm
-created and validated prior to current COVID-19 pandemic
Takeaways:
- The ROX index can be a tool to help predict whether a patient with pneumonia on HFNC may need mechanical ventilation or higher level of care
- May be most helpful with patients with pneumonia on HFNC boarding in the ED
- At 12 hours of HFNC, ROX index of >4.88 suggests patient likely to succeed with HFNC vs. <3.85 which suggests likely need for mechanical ventilation
Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016;35:200-5.
Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am J Respir Crit Care Med. 2019;199(11):1368-1376.
Category: Critical Care
Keywords: dexamethasone, steroids, respiratory failure, COVID-19, SARS-CoV-2, RECOVERY (PubMed Search)
Posted: 7/14/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
The RECOVERY (Randomized Evaluation of COVid-19 thERapY) investigators recently published a non-peer reviewed article on their findings utilizing dexamethasone to treat patients with COVID-19.
Rx: Dexamethasone 6mg daily* x 10 days (PO or IV) *or steroid equivalent
Primary outcome: All-cause mortality at 28-days
Secondary outcomes:
Results:
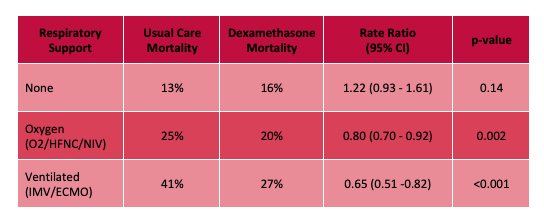
Limitations:
Bottom Line: Strongly consider admininstering dexamethasone to your patients with known COVID-19 who require respiratory support, and look for the peer-reviewed publication from the RECOVERY Trial investigators.
Horby P, Lim WS, Emberson et al. Effect of Dexamethasone in Hospitalized Patients with COVID-19: Preliminary Report. https://www.medrxiv.org/content/10.1101/2020.06.22.20137273v1 (Accessed July 14th, 2020)
Category: Critical Care
Keywords: Contrast induced nephropathy; acute kidney injury; consensus statement (PubMed Search)
Posted: 7/7/2020 by Kim Boswell, MD
Click here to contact Kim Boswell, MD
We all know the frustration that comes with the phone call from radiology asking if you “really want IV contrast” for your patient’s CT because the creatinine is elevated…
Recently, a joint statement was published between the American College of Radiology and the National Kidney Foundation regarding the safety of IV contrast in patients with kidney disease. The recommendations are based on GFR and apply to those with both chronic kidney disease as well as those who have an acute kidney injury. Summary points of the statement are below:
Every decision to use contrast should be made based on clinical need for contrast as well as individual patient risk factors and underlying disease processes.
Use of Intravenous Iodinated Contrast Media in Patients With Kidney Disease: Consensus Statements From the American College of Radiology and the National Kidney Foundation. Radiology. 2020 Mar;294(3):660-668. doi: 10.1148/radiol.2019192094. Epub 2020 Jan 21.
Category: Critical Care
Keywords: Neutrophils, Lymphocytes, NLR, ANC, ALC, Sepsis, COVID (PubMed Search)
Posted: 6/30/2020 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
As has been previously noted, the white blood cell count is "the last refuge of the intellectually destitute." However, within a CBC (especially if a differential is obtained), there is information that can sometimes be of value. One measure, which was noted before COVID but has come under increasing attention in the current pandemic, is the Neutrophil-To-Lypmhocyte Ratio (NLR). Because physiologic stress typically causes the Absolute Neutrophil Count (ANC) to increase and the Absolute Lymphocyte Count (ALC) to decrease, the ratio of the two values (NLR = ANC/ALC) should increase when the body is under stress. Similar to the WBC however, it should be noted that ANY source of physiologic stress can cause abnormalities of the NLR, and thus this is not limited strictly to infectious etiologies.
With that caveat in mind, the NLR can sometimes be a clue to the degree of physiologic stress the patient is under. As lymphopenia is a frequent finding in COVID, the NLR has come under particular interest in the setting of COVID and appears to have prognostic value in COVID+ patients.
It should be kept in mind that inflammatory stressors (e.g. sepsis) are likely to disproportionately raise the NLR relative to noninflammatory stressors (e.g. pulmonary embolism), so a septic patient with an NLR of 10 might not be all that ill, whereas a PE patient with an NLR of 10 may be sicker. As with any single lab, and particularly one so nonspecific, there are no hard and fast cutoffs, and the NLR has to be interpreted in the context of other clinical data (it is very much possible to have a high NLR and not be that sick, or to have a low NLR and be sick... this is only one datapoint and does have pitfalls associated with it). As a rough guide however, a Pulmcrit post by Josh Farkas from 2019 suggested the following interpretation of the NLR:
1-3: Normal
6-9: Mild stress (e.g. uncomplicated appendicitis)
9-18: Moderate stress, may be associated with critical illness
>18: Severe stress, commonly associated with critical illness
The post (see references below) provides an excellent overview of NLR, further information on the uses and pitfalls of NLR, and several additional sources on the subject. It's a very worthwhile read.
Bottom Line: The Neutrophil-To-Lymphocyte Ratio (NLR = ANC/ALC) is one indicator of the degree of physiologic stress, and may be used in conjuction with other clues to determine how sick your patient is.
Category: Critical Care
Keywords: ICH, stroke, hemorrhagic, platelet, DDAVP, desmopressin (PubMed Search)
Posted: 6/23/2020 by Robert Brown, MD
Click here to contact Robert Brown, MD
Mortality is high in intracranial hemorrhage, and even higher for anti-platelet associated ICH (AP-ICH). The Platelet Transfusion Versus Standard Care After Acute Stroke Due to Spontaneous Cerebral Hemorrhage Associated with Antiplatelet Therapy (PATCH) trial was shocking: it demonstrated platelet transfusion was associated with worse outcomes, excluding those patients who were planned to go to surgery in the next 24 hours. SCCM and the Neurocritical Care Society recommend AGAINST platelet transfusion in non-operative ICH, but encourage a dose of DDAVP.
But who knows who will go to surgery? If you've been giving platelets and DDAVP to non-operative AP-ICH, you're not alone. So in the July Issue of Crit Care Medicine, the authors of the PATCH trial published a retrospective study of 140 patients, excluding those who immediately had surgery. In this group in which a quarter eventually had decompressive craniectomy and a fifth had an external ventricular drain placed, half received platelets and DDAVP instead of DDAVP alone.
The result? Still no benefit to platelet transfusion (despite the inclusion of patients who went on to have surgery). We all WANT to give platelets to AP-ICH, but there is NO evidence of BENEFIT and we may cause HARM. A test of platelet function (like the TEG) should be performed at the very least to select for patients with actual platelet dysfunction, and transfusion should be limited to patients going to surgery.
Mengel A, Stefanou M, Hadaschik K, et al. Early Administration of Desmopressin and Platelet Transfusion for Reducing Hematoma Expansion in Patients With Acute Antiplatelet Therapy Associated Intracerebral Hemorrhage. Crit Care Med 2020; 48:1009-1017
Baharoglu M, Cordonnier C, Al-Shahi R, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): A randomised, open-label, phase 3 trial. Lancet 2016; 387:2605-2613
Frontera J, Lewin J, Rabinstein A, et al. Guideline for reversal of antithrombotics in intracranial hemorrhage: A statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care 2016; 24:6-46
Category: Critical Care
Posted: 6/16/2020 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Analgesics & Sedatives in the Critically Ill Obese Patient
Erstad BL, Barletta JF. Drug dosing in the critically ill obese patient - a focus on sedation, analgesia, and delirium. Crit Care. 2020; 24:315.
Category: Critical Care
Keywords: Covid-19, hydroxychloroquine, prophylaxis (PubMed Search)
Posted: 6/9/2020 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
Patient
· A North America multicenter study involving 821 asymptomatic patients who had exposure to Covid-19-positive patients. The study was double-blind, placebo-controlled randomized trial.
Intervention
· Within 4 days of exposure, participants were randomized to receive hydroxychloroquine. Dose of hydroxychloroquine was 800 mg once then 600 mg in 6-8 hours then 600 mg daily for 4 more days.
· There were 414 patients in this arm. Median age 41 years [IQR 33-51]
Comparison:
· Placebo treatment. There were 407 patients in this arm. Median age 40years [IQR 32-50]
Outcome:
· Incidence of either laboratory-confirmed Covid-19 or Covid-19 symptoms within 14 days.
Results:
· 49 (11.8%) patients with treatment had Covid-19 findings (positive tests or symptoms)
· 58 (14.3%) patients with placebo had Covid-19 findings (p=0.35).
· The absolute difference was -2.4%. The number need to treat (NNT) to prevent one infection is 42 patients. Number needed to harm is 50 patients.
· Symptoms were fatigue (49.5%), cough (44.9%), sore throat (40.2%) myalgia (37.4%), fever (34.6%), anosmia (23.4%), shortness of breath (18.7%).
Conclusion:
Hydroxychloroquine prophylaxis did not prevent post-exposure Covid-19 infection.
A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19.
Boulware DR, Pullen MF, Bangdiwala AS, Pastick KA, Lofgren SM, Okafor EC, Skipper CP, Nascene AA, Nicol MR, Abassi M, Engen NW, Cheng MP, LaBar D, Lother SA, MacKenzie LJ, Drobot G, Marten N, Zarychanski R, Kelly LE, Schwartz IS, McDonald EG, Rajasingham R, Lee TC, Hullsiek KH.
N Engl J Med. 2020 Jun 3. doi: 10.1056/NEJMoa2016638. Online ahead of print.
PMID: 32492293
