Category: Critical Care
Keywords: critically ill, ED, boarding, outcome (PubMed Search)
Posted: 11/25/2025 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Settings: this is a meta-analysis of 17 observational studies about boarding of critically ill patients in US Emergency Departments. All studies were from urban, academic centers.
Participants:
Outcome measurement: all cause mortality, as reported by the authors of the original studies.
Study Results:
Discussion:
Conclusion:
Critically ill patients boarding in the U.S. Emergency Departments were associated with a non-statistically signi?cant increase in odds of mortality and hospital length of stay compared to non-boarded patients
Htet NN, Walker JA, Jafari D, Rech MA, Hintze T, Moran M, Bai J, Dinh K, Essaihi A, Wilairat S, Huddleson B, Tran QK. Outcomes of boarding critically ill patients in U.S. EDs: A systematic review and meta-analysis. Am J Emerg Med. 2025 Oct 17;99:339-347. doi: 10.1016/j.ajem.2025.10.036. Epub ahead of print. PMID: 41151219.
Category: Critical Care
Keywords: bicarbonate, metabolic acidosis, renal replacement therapy, acute kidney injury (PubMed Search)
Posted: 11/25/2025 by Jessica Downing, MD
Click here to contact Jessica Downing, MD
The role of sodium bicarbonate in the treatment of severe acidemia has been controversial, with some studies suggesting no benefit, and others indicating that it may help reduce need for renal replacement therapy (RRT) and even improve mortality. The BICARICU-2 Trial was an open-label multicenter RCT conducted in France that evaluated the impact of a bicarb infusion among patients with metabolic acidosis and moderate to severe AKI.
There was no difference in 90 day mortality, but patients in the bicarb group were less likely to be started on RRT (38% vs 47% in the control group) using pre-defined criteria for RRT initiation, and had a 50% lower rate of bloodstream infections. Patients in the bicarb group who were started on RRT met criteria for RRT later than those in the control group (median 31h vs 15.5h).
Study Details:
Patient Population:
Intervention:
RRT Triggers:
Jung B, Jabaudon M, De Jong A, Bitker L, Audard J, Klouche K, Sarton B, Guitton C, Lasocki S, Rieu B, Canet E, Jeantrelle C, Roquilly A, Mayaux J, Verdonk F, Pottecher J, Ferrandiere M, Riu B, Garcon P, Assefi M, Detouche P, Forel JM, Roger C, Bourenne J, Jacquier S, Bougon D, Rolle A, Corne P, Benchabane N, Richard JC, Asehnoune K, Chanques G, Reignier J, Belafia F, Fosset M, Huguet H, Futier E, Molinari N, Jaber S; BICARICU-2 Study Group. Sodium Bicarbonate for Severe Metabolic Acidemia and Acute Kidney Injury: The BICARICU-2 Randomized Clinical Trial. JAMA. 2025 Oct 29:e2520231. doi: 10.1001/jama.2025.20231. Epub ahead of print. PMID: 41159812; PMCID: PMC12573113.
Category: Infectious Disease
Keywords: Dalbavancin, bacteremia, antibiotics, transitions of care (PubMed Search)
Posted: 11/17/2025 by Lena Carleton, MD
(Updated: 11/24/2025)
Click here to contact Lena Carleton, MD
Treatment of Staphylococcus aureus bacteremia has traditionally required several weeks of intravenous antibiotics. This approach carries medical risks, such as catheter-associated infection or thrombosis, as well as significant social and financial burdens for patients. Dalbavancin, a long-acting intravenous lipoglycopeptide with activity against S. aureus (including MRSA), has been proposed as a more convenient alternative. This study evaluated the efficacy and safety of dalbavancin compared with standard therapy for S. aureus bacteremia.
Two hundred adults were enrolled in this open-label, randomized clinical trial, which was conducted in the United States and Canada. After blood cultures cleared, participants were randomized to complete therapy with dalbavancin (administered on Days 1 and 8) or with standard treatment (cefazolin for MSSA and vancomycin or daptomycin for MRSA).
The primary outcome was the Desirability of Outcome Ranking (DOOR) at Day 70, incorporating five domains: clinical success, infectious complications, safety events, mortality, and health-related quality of life.
Dalbavancin was not superior to standard therapy for treating S. aureus bacteremia, and adverse events were similar between groups. A key strength of this study was the inclusion of people who inject drugs, a population at high risk for S. aureus bacteremia and often underrepresented in trials. A major limitation was that the DOOR metric did not account for important social and economic factors, such as disposition (home versus skilled nursing facility), caregiver burden, or treatment cost.
Key Takeaway: Dalbavancin may be a suitable alternative to traditional therapy for Staphylococcus aureus bacteremia, offering less frequent dosing and a shorter treatment course. Further research is needed to identify which patients benefit most and to evaluate its impact on social and economic factors such as discharge disposition, caregiver burden, and treatment costs.
Turner NA, Hamasaki T, Doernberg SB, et al. Dalbavancin for Treatment of Staphylococcus aureus Bacteremia: The DOTS Randomized Clinical Trial. JAMA. 2025;334(10):866–877. doi:10.1001/jama.2025.12543
McCreary EK, Malani PN. New Pathways to Treat Staphylococcus aureus Bacteremia: Connecting the DOTS. JAMA. 2025;334(10):861–863. doi:10.1001/jama.2025.13717
Category: Trauma
Keywords: brain injury, score, prediction (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/23/2025)
Click here to contact Robert Flint, MD
In 252 mild traumatic brain injury patients seen at 3 level I centers that were given the Rivermead Post Concussion Symptoms Questionnaire within 24 hours of arrival, 3 month post concussive symptoms were significantly correlated with their score on the questionnaire. This questionnaire take 3 minutes to complete. This may be helpful in prognosticating who will have post-concussive symptoms and who will need additional follow up.
Gray, Samuel et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Orthopedics
Posted: 11/22/2025 by Brian Corwell, MD
(Updated: 2/1/2026)
Click here to contact Brian Corwell, MD
Turf Toe:
Increased recent attention due to injuries in high profile athletes
Sprain of the first MTP joint
Mechanism: Forced hyperextension of the great toe (most common)
https://briandorfman.com/wp-content/uploads/2015/11/b_12_3_6a.jpg
Causes injury to the MTP joint capsule and surrounding ligaments
Presents as pain, swelling, discoloration, tenderness to palpation, possible joint laxity
Pain with active and passive ROM (both flexion and extension)
Graded 1-3 (Sprain, partial rupture, significant/complete rupture)
Most commonly seen in athletes who compete on artificial turf.
More rigid than natural grass
Synthetic surfaces do not release cleats as easily as natural grass
Improved synthetic surfaces perform more similar to natural grass
Much higher incidence in games vs practices.
In football, quarterbacks and running backs at highest risk
Between 30 and 45% of professional football players claim that they have experienced a turf toe injury, with over 80% of those injuries occurring on artificial turf
The combination of more rigid synthetic surfaces and lighter, more flexible shoes, increase risk of hyperextension injuries
Treatment: usually non operative
Rest/ice/taping after acute swelling decreased/stiff sole shoe/crutches/NSAIDs.
Consider walking boot or short leg splint for severe injuries
Less than 2% of injuries require surgery
Category: Pediatrics
Keywords: Community EDs, pediatric patients, mortality (PubMed Search)
Posted: 11/21/2025 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
Children account for up to 20% of emergency department visits. In the US, up to 90% of children’s visits to emergency departments are to general EDs. The weighted pediatric readiness score (WPRS) was developed to assess the level of readiness of emergency departments to care for pediatric patients. The last assessment was in 2013 showed a mean score of 68.9. High readiness scores have been associated with decreased mortality. The same holds true for children with injuries presenting to trauma centers. The higher the WPRS score, the lower the risk of in hospital death. There was no difference if the patient presented in cardiac arrest. A 10 point increase in WPRS is associated with a lower odds of potentially avoidable transfers in both trauma and medical patients. More recent data has been collected, but has not yet been published. More information on pediatric readiness (for hospitals and EMS) can be found at: https://emscimprovement.center/domains/pediatric-readiness/.
Bottom line: Being Pediatric Ready improves the care of children.
Harper JA, Coyle AC, Tam C, Skakum M, Ragheb M, Wilson L, Lê ML, Klassen TP, Aregbesola A. Readiness of emergency departments for pediatric patients and pediatric mortality: a systematic review. CMAJ Open. 2023 Oct 17;11(5):E956-E968. doi: 10.9778/cmajo.20210337. PMID: 37848258; PMCID: PMC10586495.
Category: Geriatrics
Keywords: hip fracture, nerve block, mortality, delerium (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/20/2025)
Click here to contact Robert Flint, MD
In reviewing the limited literature available, the authors found that fascia iliaca blocks did not improve mortality but did improve hospital length of stay, decreased opiate use, and decreased delirium rates. More research is needed, however this tool should be added to our multimodal pain control toolbox.
Finch, Alexander S. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: EMS
Keywords: VF, AED, CPR, public health (PubMed Search)
Posted: 11/19/2025 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
Early defibrillation is a key step in the cardiac arrest chain of survival. Public Access AEDs may be available more readily than waiting for first responders. Outside of simple awareness of where AEDs are located, there are newer ways to become aware of public AEDs near a cardiac arrest including cell phone apps or information given by 911. A British study showed that only 5.9% of AEDs were within 100 meters of the patient and 35% were within 500 meters. The distance between the AED and arrest may be a barrier for bystander AED use. This study looked to determine the time required to retrieve an AED and they hypothesized that a distance > 400 meters would be longer than the EMS response times.
This study used 15 women and 15 men to perform different runs in various environments in different seasons, retrieving AEDs at 200m through 600m and bringing it back to the patient. In these scenarios, only the 200m distance (400 m round trip) times were deemed to allow enough time to apply and use the AED prior to EMS arrival. Barriers to AED retrieval included traffic lights, cars, weather and pedestrians.
Gramm ER, Gumucio JA, Flickinger K, Salcido DD, Menegazzi JJ. Improving Bystander Response: How Long Does It Take to Retrieve an AED From Varying Distances. Prehosp Emerg Care. 2025 Apr 1:1-5. doi: 10.1080/10903127.2025.2475323. Epub ahead of print. PMID: 40126392.
Category: Critical Care
Posted: 11/18/2025 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
This is an actual patient case:
65 y/o pt intubated for hemoptysis and started on nebulized transexamic acid. Overnight, the pt is found to have severe breath stacking/auto-PEEPing and consequently is started on neuromuscular blockade. The pt has no history of asthma or COPD and the ETT is clear without obstruction.
Ventilator waveforms are as shown. What is the issue?
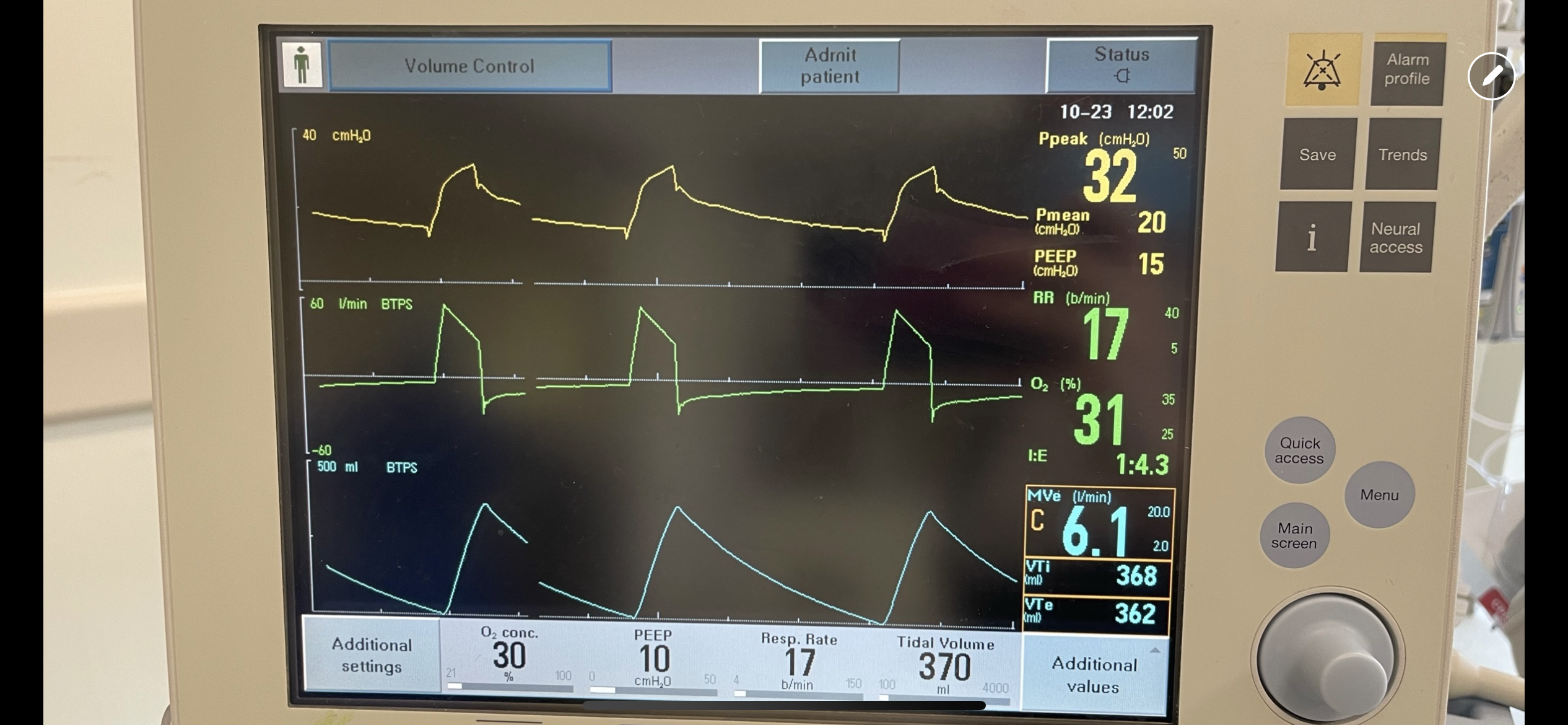
Explanation:
On expiration, the ventilator pressure (and the pressure curve waveform on the ventilator) should drop to the set PEEP (10 cm H2O in this case) immediately. This is true regardless of whether it is volume control, pressure control, PRVC etc. For this patient, the pressure curve is not dropping to the set PEEP immediately on expiration, rather, it slowly decays and does not even reach the set PEEP before the beginning of the next breath. This is not due to a patient issue, but rather an obstruction at the level of the ventilator. In particular, an obstruction in the expiratory limb of the tubing where flow returns to the ventilator from the patient. TXA is known to crystallize on the expiratory filter which can cause this type of obstruction if it is not changed frequently enough, preventing the pressure from dropping to PEEP and the patient from fully exhaling.
In this case, the obstruction was localized to the expiratory filter based on the ventilator waveforms and the filter was exchanged. The waveforms normalized, the patient had no obstruction or breath stacking, the neuromuscular blockade discontinued, and the patient was subsequently extubated without issue.
Category: Trauma
Keywords: rsi, neck injury, penetrating, airway (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/16/2025)
Click here to contact Robert Flint, MD
This group looked at 88 patients intubated for penetrating neck injury and found 95% received neuromuscular blocking agents, 73% were intubated using a bougie, and 95% were intubated on first pass.
The authors concluded; “Rapid sequence intubation with bougie use was an effective default approach to definitive airway management in ED patients with penetrating neck trauma.”
Lee, Daniel H. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Administration
Posted: 11/15/2025 by Kevin Semelrath, MD
(Updated: 2/1/2026)
Click here to contact Kevin Semelrath, MD
This abstract from ACEP's most recent research forum looked at the effect a patient's preferred language had on ED LOS, rate of admission, hospital length of stay and resource utilization both in the ED and the hospital.
Overall, those patients who spoke English as their primary language had lower ED LOS, less testing done in the ED, but if they got admitted they had the longest hospital LOS. Patients who preferred Spanish language had the shortest hospital LOS and were most likely to be discharged home with no services. Non-English/non-Spanish languages had the longest ED LOS and highest admission rates and had similar resource use as patients who preferred Spanish
This abstract opens the door for further research into what the underlying cause of these disparities are.
Zimmerman, T. et al.
Annals of Emergency Medicine, Volume 86, Issue 3, S3 - S4
Category: Pharmacology & Therapeutics
Keywords: andexanet alfa, 4F-PCC, Kcentra, ICH, thrombosis (PubMed Search)
Posted: 11/13/2025 by Wesley Oliver
(Updated: 2/1/2026)
Click here to contact Wesley Oliver
This pearl was adapted from a literature update presented by Castin Schulz, PharmD on November 13, 2025.
A 2025 study in the American Journal of Emergency Medicine provides new real-world data on the two most common reversal agents for factor Xa (fXa) inhibitor-related intracranial hemorrhage (ICH).
This national retrospective cohort study evaluated 350 Veterans who received either andexanet alfa (AA) or 4-factor prothrombin complex concentrate (4F-PCC) for fXa inhibitor-related ICH.
Key Findings (Propensity-Matched Analysis)
Clinical Takeaway
In this study of Veterans with fXa inhibitor-related ICH, andexanet alfa did not improve 90-day mortality compared to 4F-PCC. However, its use was associated with a significantly increased risk of 30-day thrombotic events, particularly ischemic stroke.
This study adds to a growing body of literature questioning the safety profile of AA. The authors conclude that the selection of AA should be carefully weighed against the patient's underlying risk of thrombotic events.
Rech MA, Budde E, Evans CT, et al. Andexanet alfa increases 30-day thrombotic events relative to four-factor prothrombin complex concentrate for factor Xa inhibitors-related intracerebral hemorrhage in veterans. Am J Emerg Med. 2025;97:97-102. doi:10.1016/j.ajem.2025.07.037
Category: Gastrointestional
Keywords: gastroenteritis, odansetron, prescription (PubMed Search)
Posted: 11/12/2025 by Neeraja Murali, DO, MPH
(Updated: 2/1/2026)
Click here to contact Neeraja Murali, DO, MPH
Anecdotally, we as emergency physicians are fairly comfortable prescribing odansetron to adults with nausea and vomiting. However, emergency physicians often treat pediatric gastroenteritis with a single dose of odansetron in the department. A recent study in NEJM examined effects of discharging with odansetron. Full details can be found in the study, but the take-home:
Sending children home with ondansetron after an emergency visit for gastroenteritis cut the rate of moderate-to-severe illness from 12.5% to 5.1% compared to placebo, with no uptick in adverse events. Those taking ondansetron experienced fewer vomiting episodes in the first 48 hours. Targeted, as-needed dosing helps the sickest children recover faster, while avoiding unnecessary medication for most kids.
Freedman SB, Williamson-Urquhart S, Plint AC, et al. Multidose Ondansetron after Emergency Visits in Children with Gastroenteritis. N Engl J Med. 2025;393(3):255-266. doi:10.1056/NEJMoa2503596
Category: Critical Care
Keywords: Critical Care, Surgical Critical Care, Fellowship, Training, Medical education, Emergency Medicine-Critical Care, EM-CC (PubMed Search)
Posted: 11/12/2025 by William Teeter, MD
Click here to contact William Teeter, MD
This study surveyed 111 emergency medicine (EM) trainees to identify factors influencing their choice of critical care (CC) fellowship pathways, particularly surgical critical care (SCC). Respondents included 42 fellows and 69 residents, with most pursuing anesthesiology or medicine CC; only 15 intended SCC.
Key determinants of pathway selection were:
Limited exposure to EM-SCC during residency was noted—only 28% had access to such fellowships, and 42% interacted with surgical intensivists, despite 41% envisioning SCC practice.
Intellectual appeal ranked highest for entering CC, above job prospects or lifestyle.
Fellowship components most valued were:
While descriptive, the authors noted many respondents cited the "preliminary surgical year" as a reason that the Surgical Critical Care pathway is less attractive.
The authors conclude that respondents pursued a career in CC for "intellectual appeal and desire for additional expertise" and that improving EM-SCC matriculation requires targeted interventions.
Hynes AM, Carver TW, Owodunni OP, et al. Attracting Emergency Medicine-Trained Residents to Surgical Critical Care: The Implications From a Nationwide Survey of Emergency Medicine Trainees Interested in Critical Care. Crit Care Med. 2025 Oct 31. doi: 10.1097/CCM.0000000000006935.
Category: Obstetrics & Gynecology
Keywords: miscarriage, antidepressants (PubMed Search)
Posted: 11/10/2025 by Jennifer Wang, MD
(Updated: 2/1/2026)
Click here to contact Jennifer Wang, MD
TLDR: Being on antidepressants (specifically SSRIs and SNRIs) does not increase the risk of miscarriage in the first trimester if started before pregnancy, while starting them during pregnancy might present a small increase in risk of miscarriage in that first trimester.
Researchers in the UK looked at patient data from 1996-2018, with almost a million pregnancies evaluated, to look for an association between antidepressant use and first trimester miscarriage, because studies in the past have been iffy about this whole thing. They looked at exposed patients, who were split into two categories: prevalent (started antidepressants at least 3 months prior to pregnancy) and incident (started antidepressants during pregnancy), and nonexposed patients.
The data was analyzed raw and then also after taking out what they felt like would be important confounders (including hx of miscarriage, smoking hx, antipsychotic/seizure medication use, age). Data analyzed after the confounders were taken out of the equation showed that there was no statistical difference in first trimester seizures among patients who were not exposed to SNRIs/SSRIs and prevalent users (or patients who started before pregnancy).
Among incident users, there was a small increase in risk, though the researchers noted that they were concerned about “reserve causation” or patients being started on antidepressants after they had had a miscarriage, which could have screwed with these numbers. The absolute increase in risk was 0.5% (13.1% in non-exposed, and 13.6% in exposed).
Takeaways: Given that we cannot ethically do RCTs on our pregnant patients, this is probably one of the largest population studies to date looking at this issue, and it provides reassuring data. For our patients who are on SSRIs/SNRIs before they get pregnant, you can reassure them that there is good data saying that they are not putting the fetus at increased risk of miscarriage in that first trimester. For patients who need to start on SSRIs/SNRIs during pregnancy, counsel closely, but let them know that our data shows a relatively small absolute risk increase for first trimester miscarriage.
Martin FZ, Madley-Dowd PC, Ahlqvist VH, et al. First trimester antidepressant use and miscarriage: a comprehensive analysis in the Clinical Practice Research Datalink GOLD. Br J Gen Pract. Published online August 7, 2025. doi:10.3399/BJGP.2025.0092
Category: Trauma
Keywords: primary care, hypertension, diabetes, trauma (PubMed Search)
Posted: 11/4/2025 by Robert Flint, MD
(Updated: 11/9/2025)
Click here to contact Robert Flint, MD
These authors followed 250 consecutive trauma activation patients over a one year period. In hospital elevated blood pressure and glucose level correlated with a new diagnosis of hypertension and diabetes respectively over that 1 year time line. Some of these patients also had a new diagnosis of HIV, substance use disorder and hepatitis C. Using their contact with the health system due to trauma can be a way to screen for undiagnosed medical problems such as diabetes and hypertension. Assuring outpatient follow up for these patients will have an effect on their long term morbidity and mortality.
Banks, Kian C. et al.
Journal of Emergency Medicine, Volume 0, Issue 0
Category: Orthopedics
Posted: 11/8/2025 by Brian Corwell, MD
(Updated: 2/1/2026)
Click here to contact Brian Corwell, MD
Chondrocalcinosis is a condition where calcium pyrophosphate crystals form in the joints (particularly the knee and wrist), leading to inflammation and pain.
Appears as a cloudlike radiopacity in the knee’s articular cartilage and meniscus on XR, reflecting abnormal calcium-based crystal deposition.
This can be distinguished from the radiolucent appearance of monosodium urate crystals of gout.
https://www.wikidoc.org/index.php/File:MSUandCPPD.png
These calcium crystals are common in end-stage knee osteoarthritis and have been associated with disease severity.
Due to this well-observed coexistence (chondrocalcinosis and knee osteoarthritis), chondrocalcinosis is commonly considered a manifestation of osteoarthritis pathology.
However, this does not explain the commonly encountered instances where chondrocalcinosis appears in radiographically normal knees. This raises questions of whether chondrocalcinosis is a cause or merely a consequence of end-stage osteoarthritis.
Population studies have identified that about 6.% of individuals have chondrocalcinosis in joints unaffected by osteoarthritis
In a recent analysis including more than 6400 middle-aged to older adults, individuals with knee chondrocalcinosis were 75% more likely to develop knee OA than those without the condition at baseline.
Chondrocalcinosis may contribute to the risk of osteoarthritis through inflammation. These deposited crystals could induce the production of inflammation markers, matrix-degrading enzymes and induce chondrocyte hypertrophy or chondrocyte death. These effects not only damage the joint but also form a positive feedback loop to produce more calcium crystals.
Individuals with chondrocalcinosis may represent a specific subgroup of patients, for which a treatment targeting chondrocalcinosis induced inflammation may present a viable strategy to prevent osteoarthritis in this patient subgroup.
This idea has some support from the 2023, LoDoCo2 trial, (approx. 5500 patients) which showed an association between the use of colchicine, 0.5 mg daily, with a lower incidence of total knee and total hip replacements.
Wu Y, Liew JW, et al. Chondrocalcinosis and incident knee osteoarthritis: findings from 2 large prospective cohorts with 20 years of follow-up. Ann Rheum Dis. 2025 Oct;84(10):1743-1751.
Category: Pediatrics
Posted: 11/7/2025 by Julie Kurek, MD
(Updated: 2/1/2026)
Click here to contact Julie Kurek, MD
A recent randomized control trial published in JAMA Pediatrics in January 2025 showed improvement in first attempt for IV access when using ultrasound in the pediatrics ED.
This trial was performed at a quaternary pediatric hospital in Australia with a total of 164 patients (ages 18 and younger). Median age of the patients was 24 months. There was computerized system that randomized patients into either getting an IV by standard procedure vs ultrasound-guided. Those placing the ultrasound-guided IV had extensive training. Overall, the first time success rate was higher in the ultrasound group with about 85.7% compared to 32.5% in the standard group.
Main point: US IV decreases the number of sticks a child has to experience for IV access with a higher first stick success rate. Consider US IV training in your Pediatric Emergency Department in the future. Also use ultrasound guidance with first attempt IV access for your chronically ill children or for very anxious parents.
Kleidon TM, Schults JA, Royle RH, et al. First-Attempt Success in Ultrasound-Guided vs Standard Peripheral Intravenous Catheter Insertion: The EPIC Superiority Randomized Clinical Trial. JAMA Pediatr. 2025;179(3):255–263. doi:10.1001/jamapediatrics.2024.5581
Ultrasound-Guided Pediatric PIVC Placement. AAP Grand Rounds May 2025; 53 (5): 58. https://doi.org/10.1542/gr.53-5-58
Category: Ultrasound
Keywords: Ultrasound, APPLES, bursa (PubMed Search)
Posted: 11/4/2025 by Kerith Joseph, MD
(Updated: 11/6/2025)
Click here to contact Kerith Joseph, MD
Summary:
This study evaluated whether the line-of-sight approach improves the speed and accuracy of ultrasound-guided needle placement into the subdeltoid bursa among novice operators, compared to the side approach. A secondary aim was to assess the usefulness of the APPLES mnemonic (Angle, Position, Perpendicular, Line up, Entry, Sweep) as a teaching aid.
Methods:
Medical students and residents were randomized to perform the procedure using both approaches in a crossover design. Two blinded reviewers measured procedure time, and participants completed a survey on their preferences and perceptions of APPLES. Statistical tests (paired t test, McNemar test) compared performance time and accuracy.
Results:
The line-of-sight approach significantly reduced procedure time (mean 14.4 s vs. 18.6 s; P = .00029).
Participants were more likely to hit the target within 30 s using the line-of-sight approach (P = .035).
72.7% preferred the line-of-sight approach.
88.2% found the APPLES mnemonic helpful.
Conclusions:
The operator’s positioning plays a key role in ultrasound-guided procedures. The line-of-sight approach improves both speed and accuracy for novice users, and the APPLES mnemonic is a valuable educational tool for teaching these techniques.
Kerith Joseph MD, RMSK
Clinical Associate Professor
University of Maryland School of Medicine
Baltimore Veterans Affairs Medical Center, Emergency Department
Category: Toxicology
Keywords: Cyanide, antidote, hydroxycobalmin, drug shortage (PubMed Search)
Posted: 11/5/2025 by Kathy Prybys, MD
(Updated: 2/1/2026)
Click here to contact Kathy Prybys, MD
Cyanide is one of the deadliest known poisons causing immediate toxic effects and lethality within seconds to minutes. Exposures are rare, most commonly by inhalational route (HCN gas) from structural fires due to combustion of synthetic materials or from ingestion of cyanide salts. Cyanide toxicity can also occur from dermal or parental (sodium nitroprusside) exposure.
The preferred first line antidote is hydroxycobalamin (vitamin B12) available as Cyanokit, which has higher affinity for cyanide than cytochrome oxidase and binds to form harmless cyanocobalamin and is renally excreted. Limited studies reveal good survival rates in noncardiac arrest patients. Hydroxycobalamin has minimal side effects (red skin and urine, increased BP) and is well-tolerated with safer and simpler mechanism of action than Nithiodote (original antidote), containing sodium nitrite (CN preferentially binds methemoglobin to form cyanomethemoglobin) and thiosulfate (provides sulfur to convert cyanide to thiocynate for excretion). Sodium nitrite has numerous adverse effects causing hypotension and methemoglobin (contraindicated in smoke inhalation victims due to concern for carbon monoxide poisoning, G6PD deficiency, preexisting amenia), and hypersensitivity reactions. Sodium thiosulfate has less side effects and augments cyanide excretion but is considered less effective due to its slow onset, short half-life, low volume of distribution, and poor intracellular penetration.
As of August 2025, the American Society of Health -System Pharmacists (ASHP) Drug Shortage lists Cyanokit as “limited availability” in the U.S. as manufacturing was suspended due to investigation of ongoing quality defect with concern for sterility and endotoxin content. Impacted batches were released and their numbers are listed in an FDA bulletin (see references). Healthcare providers should weigh the potential benefit of using Cyanokit against the risk of infection. Infusion set with 0.2 micron in line filter can be temporarily used for administration of Cyanokit 5 mg hydroxycobalmin to prevent potential infection.
Surviving Cyanide Poisoning: A case report highlighting the role of early antidote use. Hopes BC, Slob EM, et al. Toxicology Reports, Volume 15, December 2025.
Challenges in the diagnosis of acute cyanide poisoning. Parker-Cote JL, Rizer J, et al. Clin Toxicol. 2018 Jul:56(7):609-617.
American Society of Health -System Pharmacists (ASHP) Drug Shortage Detail-Hydroxocobalmin for injection 9/22/2025.
February 6, 2025 Manufacturer letter to healthcare professional https://www.fda.gov/media/185400/download
