Category: Critical Care
Keywords: Pressors, Vasopressin, Sepsis, Septic Shock (PubMed Search)
Posted: 5/31/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Norepinephrine is widely considered the first-line vasopressor for patients in septic shock. Vasopressin is often added to norepinephrine in patients requiring escalating doses, but when to add vasopressin, and what exactly the benefit is (as opposed to just further titrating up the norepinephrine) remain unclear. Given the limited evidence for a patient-oriented benefit and the increasing cost of vasopressin, some centers are becoming more judicious in the use of vasopressin. A systematic review in AJEM October 2021 examined the literature on early (< 6 hours of diagnosis) addition of vasopressin to the management of septic shock patients, compared to either no vasopressin or starting it after 6 hours.
Improved with early vasopressin: Need for renal replacement therapy (RRT; secondary outcome)
No difference: mortality, ICU length of stay, hospital length of stay, new onset arrhythmias
Bottom Line: When, and if, to start vasopressin in patients requiring escalating doses of norepinephrine remains controversial. Based on the prior VASST trial, many providers will start vasopressin when norepi doses reach ~ 5-15 mcg/min (approx 0.1-0.2 mcg/kg/min), but there remains limited data to support this practice, and either starting vasopressin or continuing to titrate the norepinephrine as needed are both reasonable approaches in most patients.
1) Huang H, Wu C, Shen Q, Xu H, Fang Y, Mao W. The effect of early vasopressin use on patients with septic shock: A systematic review and meta-analysis. Am J Emerg Med. 2021 May 6;48:203-208. doi: 10.1016/j.ajem.2021.05.007. Epub ahead of print. PMID: 33975132.
2) Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008 Feb 28;358(9):877-87. doi: 10.1056/NEJMoa067373. PMID: 18305265.
3) Lam SW, Barreto EF, Scott R, Kashani KB, Khanna AK, Bauer SR. Cost-effectiveness of second-line vasopressors for the treatment of septic shock. J Crit Care. 2020 Feb;55:48-55. doi: 10.1016/j.jcrc.2019.10.005. Epub 2019 Oct 23. PMID: 31706118.
Category: Critical Care
Posted: 5/25/2021 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Refractory Anaphylaxis
Krishnaswamy G. Critical care management of anaphylaxis: A conside definitive review. Crit Care Med. 2021.
Category: Critical Care
Keywords: COVID-19, tocilizumab, ICU, mechanical ventilation (PubMed Search)
Posted: 5/11/2021 by Lindsay Ritter, MD
(Updated: 2/1/2026)
Click here to contact Lindsay Ritter, MD
RECAP: RECOVERY trial is a large, randomized, open label, adaptive trial studying different treatments on COVID-19. Most well known is the use of dexamethasone which reduced mortality by 1/3 in COVID patients requiring mechanical ventilation and by 1/5 in those requiring oxygen, with no benefit on those patients not requiring oxygen.
They recently published results in the Lancet on the use of tocilizumab.
Population:
Inclusion:
Outcomes:
Results:
Conclusion:
RECOVERY Collaborative Group Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021; 397: 1637-1645
Category: Critical Care
Keywords: cardiac arrest, massive pulmonary embolism, Venoarterial, ECMO (PubMed Search)
Posted: 5/4/2021 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
Background:
Cardiac arrest from massive pulmonary embolism (PE) can be up to 90% (1). A recent systemic review evaluated the efficacy of Venoarterial-Extracorporeal Membrane Oxygenation (VA-ECMO) for PE-related cardiac arrest.
Results:
The authors screened 1115 articles and included 77 articles, including gray literature. The authors performed a quantitative analysis of a total of 301 patients.
Overall, 183/301 (61%) patients survived to hospital discharge, a significant improvement from 90%.
Patients who were cannulated during chest compression were associated with 7x higher odds of death (OR, 6.84; 95% CI, 1.53–30.58; p = 0.01), compared to those who were cannulated after ROSC. However, cannulation in the ED was not associated with improved outcomes, compared with other cannulation site.
No increased risk of death among patients who received tPA prior to VA-ECMO vs. those who did not (OR, 0.78; 95% CI, 0.39–1.54; p = 0.48).
Patients whose age > 65 years of age were associated with 3X risk of death, compared to those with age < 65 years (OR, 3.56; 95% CI, 1.29–9.87; p = 0.02).
Take-home points
Please consider “early” VA-ECMO for eligible patients who have cardiac arrest from massive PE. However, it will take great convincing to push the PERT team to cannulate for VA-ECMO while the patient is still receiving chest compression.
1.Lavonas EJ, Drennan IR, Gabrielli A, et al: Part 10: Special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132:S501–S518.
2. Scott JH, Gordon M, Vender R, Pettigrew S, Desai P, Marchetti N, Mamary AJ, Panaro J, Cohen G, Bashir R, Lakhter V, Roth S, Zhao H, Toyoda Y, Criner G, Moores L, Rali P. Venoarterial Extracorporeal Membrane Oxygenation in Massive Pulmonary Embolism-Related Cardiac Arrest: A Systematic Review. Crit Care Med. 2021 May 1;49(5):760-769. doi: 10.1097/CCM.0000000000004828. PMID: 33590996.
Category: Critical Care
Keywords: cardiac arrest, massive pulmonary embolism, Venoarterial, ECMO (PubMed Search)
Posted: 5/4/2021 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Background:
Cardiac arrest from massive pulmonary embolism (PE) can be up to 90% (1). A recent systemic review evaluated the efficacy of Venoarterial-Extracorporeal Membrane Oxygenation (VA-ECMO) for PE-related cardiac arrest.
Results:
The authors screened 1115 articles and included 77 articles, including gray literature. The authors performed a quantitative analysis of a total of 301 patients.
Overall, 183/301 (61%) patients survived to hospital discharge, a significant improvement from 90%.
Patients who were cannulated during chest compression were associated with 7x higher odds of death (OR, 6.84; 95% CI, 1.53–30.58; p = 0.01), compared to those who were cannulated after ROSC. However, cannulation in the ED was not associated with improved outcomes, compared with other cannulation sites.
No increased risk of death among patients who received tPA prior to VA-ECMO vs. those who did not (OR, 0.78; 95% CI, 0.39–1.54; p = 0.48).
Patients whose age > 65 years of age were associated with 3X risk of death, compared to those with age < 65 years (OR, 3.56; 95% CI, 1.29–9.87; p = 0.02).
Take-home points
Please consider “early” VA-ECMO for eligible patients who have cardiac arrest from massive PE. However, it will take great convincing to push the PERT team to cannulate for VA-ECMO while the patient is still receiving chest compression.
1.Lavonas EJ, Drennan IR, Gabrielli A, et al: Part 10: Special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132:S501–S518.
2. Scott JH, Gordon M, Vender R, Pettigrew S, Desai P, Marchetti N, Mamary AJ, Panaro J, Cohen G, Bashir R, Lakhter V, Roth S, Zhao H, Toyoda Y, Criner G, Moores L, Rali P. Venoarterial Extracorporeal Membrane Oxygenation in Massive Pulmonary Embolism-Related Cardiac Arrest: A Systematic Review. Crit Care Med. 2021 May 1;49(5):760-769. doi: 10.1097/CCM.0000000000004828. PMID: 33590996
Category: Critical Care
Keywords: COPD, emphysema, acute respiratory failure, hypoxia, oxygen saturation (PubMed Search)
Posted: 4/20/2021 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Supplemental oxygen therapy is frequently required for patients presenting with acute respiratory distress and COPD exacerbation. Over-oxygenation can derail compensatory physiologic responses to hypoxia,1 resulting in worsening VQ mismatch and, to a lesser degree, decreases in minute ventilation, that cause worsened respiratory failure.
The 2012 DECAF (Dyspnea, Eosinopenia, Consolidation, Acidaemia, and Atrial Fibrillation) score was found to predict risk of in-hospital mortality in patients admitted with acute COPD exacerbation.2,3 Data from the DECAF study’s derivation and external validation cohorts were examined specifically to look at outcome associated with varying levels of oxygen saturation.
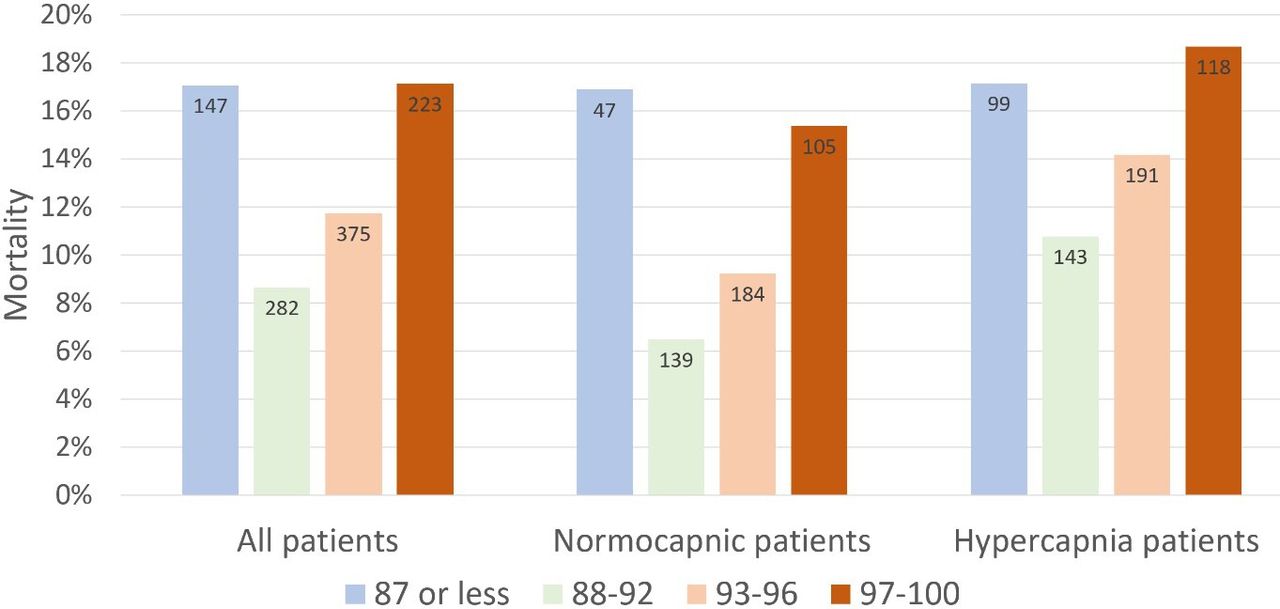
Bottom Line
In patients presenting to the ED with acute COPD exacerbation requiring oxygen supplementation, a target oxygen saturation of 88-92% is associated with the lowest in-hospital mortality, and higher oxygen saturations should be avoided independent of patients' PCO2 levels.
Category: Critical Care
Keywords: COVID-19, Anticoagulation, Thromboembolism (PubMed Search)
Posted: 4/7/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Two items from the recent INSPIRATION trial UMEM pearl were very well pointed out by our own Dr. Michael Scott and require clarification. Thank you to all our readers for their close attention, and please know that we always appreciate you reaching out with questions/comments.
Category: Critical Care
Keywords: COVID-19, Anticoagulation, Thromboembolism (PubMed Search)
Posted: 4/7/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
COVID-19 is generally regarded as a hypercoagulable state, and the role of pulmonary emboli and other VTE in COVID remains unclear. As a result, how to optimally provide prophylactic anticoagulation in COVID-19 patients who are not known to have VTE has been a point of debate.
The INSPIRATION trial looked at 600 patients admitted to academic ICUs in Iran, and compared what is often-referred to as "intermediate-dose" prophylaxis (in this case 1 mg/kg daily of enoxaparin) to standard dose prophylaxis (40 mg/day of enoxaparin). The study utilized a combined endpoint of venous thromboembolism, arterial thromboembolism, need for ECMO, or mortality. As a reminder, composite endpoints can skew results. However, the dose and type of anticoagulant chosen is similar to many academic centers around the world, and pharmacy guidelines often recommend providing this type of "intermediate-dose" prophylaxis in COVID-19 patients, sometimes based on clinical status, d-dimer or other coagulation-related patient-data. As with many things with COVID-19, this practice is based on limited data.
There was no significant difference between groups in the primary outcome (45.7% in intermediate ppx group vs 44.1% in standard group), and while safety outcomes were similar (major bleeding in 2.5% in the intermediate ppx group vs 1.4% in standard group), the intermediate regimen failed to demonstrate non-inferiority to the standard regimen for major bleeding.
Intermediate vs standard-dose ppx was similar in this study with a small, but statistically significant increase in major bleeding in the intermediate-dose group.
Bottom Line: Although this study had methodologic flaws and there are external validity concerns, the INSPIRATION trial supports the notion that standard dose (e.g. 40 mg/g/kg/day enoxaparin) and intermediate-dose (e.g. 1 mg/kg/day enoxaparin) VTE prophylaxis are equivalent in critically ill COVID-19 patients who do not already have a known VTE in terms of preventing negative VTE outcomes. Intermediate-dose may be associated with increased bleeding. As more critically ill patients require ED boarding, the dose of VTE prophylaxis may remain controversial, but the need to start it remains an important consideration.
INSPIRATION Investigators, Sadeghipour P, Talasaz AH, Rashidi F, Sharif-Kashani B, Beigmohammadi MT, Farrokhpour M, Sezavar SH, Payandemehr P, Dabbagh A, Moghadam KG, Jamalkhani S, Khalili H, Yadollahzadeh M, Riahi T, Rezaeifar P, Tahamtan O, Matin S, Abedini A, Lookzadeh S, Rahmani H, Zoghi E, Mohammadi K, Sadeghipour P, Abri H, Tabrizi S, Mousavian SM, Shahmirzaei S, Bakhshandeh H, Amin A, Rafiee F, Baghizadeh E, Mohebbi B, Parhizgar SE, Aliannejad R, Eslami V, Kashefizadeh A, Kakavand H, Hosseini SH, Shafaghi S, Ghazi SF, Najafi A, Jimenez D, Gupta A, Madhavan MV, Sethi SS, Parikh SA, Monreal M, Hadavand N, Hajighasemi A, Maleki M, Sadeghian S, Piazza G, Kirtane AJ, Van Tassell BW, Dobesh PP, Stone GW, Lip GYH, Krumholz HM, Goldhaber SZ, Bikdeli B. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit: The INSPIRATION Randomized Clinical Trial. JAMA. 2021 Mar 18. doi: 10.1001/jama.2021.4152. Epub ahead of print. PMID: 33734299.
Category: Critical Care
Posted: 3/30/2021 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Improving Compliance with Lung-Protective Ventilation
Tallman CMI, et al. Impact of provding a tape measure on the provision of lung-protective ventilation. West J Emerg Med. 2021; 22:389-93.
Category: Critical Care
Posted: 3/16/2021 by Lindsay Ritter, MD
Click here to contact Lindsay Ritter, MD
The PARAMEDIC2 trial in NEJM 2018 studied the outcomes of the use of epinephrine in outside hospital cardiac arrest (OHCA) on survival and neurological outcome.
Methods: Conducted in Britain, randomized 8007 patients to receive either epinepherine 1mg (n=4012) or placebo (n=3995) as part of standard CPR for out-of-hosptial arrest. Their primary outcome was survival at 30 days and their secondary outcomes included length of stay as well as neurological outcomes at 30 days and 3 months.
Results: The epinepherine group had improved survival to hospital admission (23% vs. 8%), at 30 days (3.2% vs. 2.4%) or at 3 months (3% vs. 2.2%). Favourable neurological outcomes, however, had no statistical difference at both hospital discharge and at 3 months.
Bottom line: Epinephrine improves ROSC, though with poor neurological outcomes.
Important facts:
Recently, a follow up of the PARAMEDIC2 trial was completed in Resuscitation.
They reported long-term survival, quality of life, functional and cognitive outcomes at 3, 6 and 12-months.
Results: At 6 months, 78 (2.0%) of the patients in the adrenaline group and 58 (1.5%) of patients in the placebo group had a favourable neurological outcome (adjusted odds ratio 1.35 [95% confidence interval: 0.93, 1.97]). 117 (2.9%) patients were alive at 6-months in the adrenaline group compared with 86 (2.2%) in the placebo group (1.43 [1.05, 1.96], reducing to 107 (2.7%) and 80 (2.0%) respectively at 12-months (1.38 [1.00, 1.92]). Measures of 3 and 6-month cognitive, functional and quality of life outcomes were reduced, but there was no strong evidence of differences between groups.
Bottom line: Epinephrine improves survival at 12 months, but poor neurological outcomes remain.
Haywood KL, Ji C, Quinn T, Nolan JP, Deakin CD, Scomparin C, Lall R, Gates S, Long J, Regan S, Fothergill RT, Pocock H, Rees N, O'Shea L, Perkins GD. Long term outcomes of participants in the PARAMEDIC2 randomised trial of adrenaline in out-of-hospital cardiac arrest. Resuscitation. 2021 Mar;160:84-93. doi: 10.1016/j.resuscitation.2021.01.019. Epub 2021 Jan 30. PMID: 33524488.
Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O'Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R; PARAMEDIC2 Collaborators. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018 Aug 23;379(8):711-721. doi: 10.1056/NEJMoa1806842. Epub 2018 Jul 18. PMID: 30021076.
Category: Critical Care
Keywords: sepsis recognition, antibiotics administration, mortality, (PubMed Search)
Posted: 3/10/2021 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
Background:
The association between time intervals of ED antibiotic administration and outcome has been controversial. While single studies showed there was increased mortality associated with delayed antibiotic administration (1-3). A meta-analysis of 13 studies and 33000 patients showed that there was no mortality difference between septic patients receiving immediate Abx (< 1 hour) vs. those receiving early abx (1-3 hours) (4).
Since delay in recognition of sepsis (defined as ED triage to Abx order) and delay in antibiotics delivery (Abx order to administration) contribute to total delay of Abx administration, a new retrospective study (3) attempted to investigate the contributions of either factor to hospital mortality.
Results:
The study used generalized linear mixed models and involved 24000 patients.
For All patients and outcome of hospital mortality:
Recognition delay (ED triage to Abx order): OR 2.7 (95% CI 1.5-4.7)*
Administration delay at 2-2.5 hours (Abx order to administration): OR 1.5 (1.1-2.0)
These results was associated with non-statistical significance in patients with septic shocks.
Conclusion:
Delayed recognition of sepsis was associated with higher hospital mortality. Longer delay of abx administration was also associated with increased risk of hospital mortality.
1.Kumar A, Roberts D, Wood KE, et al: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006; 34:1589–1596
2. Ferrer R, Martin-Loeches I, Phillips G, et al: Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: Results from a guideline-based performance improvement program. Crit Care Med 2014; 42: 1749–1755
3. Seymour CW, Gesten F, Prescott HC, et al: Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 2017; 376:2235–2244.
4. Rothrock SG et al. Outcome of immediate versus early antibiotics in severe sepsis and septic shock: A systematic review and meta-analysis. Ann Emerg Med 2020 Jun 24; [e-pub]. (https://doi.org/10.1016/j.annemergmed.2020.04.042)
Category: Critical Care
Posted: 3/2/2021 by Caleb Chan, MD
(Updated: 2/1/2026)
Click here to contact Caleb Chan, MD
Clinical Question:
Methods:
Results:
Take-home points:
Hughes CG, Mailloux PT, Devlin JW, et al. Dexmedetomidine or propofol for sedation in mechanically ventilated adults with sepsis. N Engl J Med. Published online February 2, 2021:NEJMoa2024922.
Category: Critical Care
Keywords: HACOR, NIV, noninvasive ventilation, acute respiratory failure (PubMed Search)
Posted: 2/2/2021 by Kami Windsor, MD
(Updated: 2/23/2021)
Click here to contact Kami Windsor, MD
Background: In respiratory failure due to COPD and cardiogenic pulmonary edema, noninvasive positive pressure ventilation decreases need for intubation and improves mortality,1 while its utility in other scenarios such as ARDS and pneumonia has yet to be proven.1,2 We know that patients on NIV with delays to needed intubation have a higher mortality,1,3 but intubation and mechanical ventilation come with risks that it is preferable to avoid if possible.
So how and when can we determine that NIV is not working?
The HACOR (Heart rate, Acidosis, Consciousness, Oxygenation, Respiratory rate) score at 1 hour after NIV initiation has been demonstrated to be highly predictive of NIV failure requiring intubation.4,5
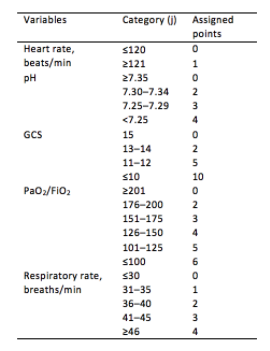
Initial development/validation: Score > 5 after 1 hour of NIV corresponds to >80% risk of NIV failure4
Earlier intubation (before 12 hours) in these patients = better survival
External validation: Score > 8 after 1 hour of NIV most predictive of eventual NIV failure 5
Average score @ 1-hour of patients with NIV success = 3.8
Score remained predictive at 6, 12, 24, 48 hours as well & mortality worsened as delay to intubation time increased
Baseline, pre-NIV score not predictive
Better predictive agreement in pneumonia and ARDS
Bottom Line:
Patients on NIV require close reassessment to prevent worsened survival due to intubation delay should invasive mechanical ventilation be indicated.
A HACOR score >8 after 1 hour of NIV should prompt intubation in most instances, with strong consideration given to a score >5.
*Note: ABGs were obtained for PaO2 assessment in the above studies -- the use of SpO2 was not evaluated -- but we are often not obtaining ABGs in our ED patients with acute respiratory failure. The following chart provides an estimated SpO2 to PaO2 conversion.
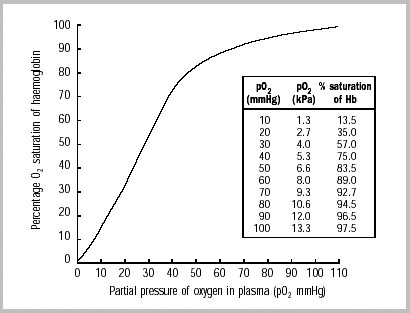
WHO 2001
Caveats:
Category: Critical Care
Keywords: Oxygenation, Mechanical Ventilation, Critical Care (PubMed Search)
Posted: 2/9/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Optimal oxygenation targets and the possible, theoretical, benefits of hyperoxygenating critically ill patients have long been points of controversy. Multiple studies have suggested harm in pursuing aggressive hyperoxygenation amongst critical patients with various conditions ranging from myocardial infarction to sepsis to neurologic conditions. In addition, oxygen toxicity is a known mechanism causing ARDS.
The HOT-ICU trial adds to the list of arguments against hyperoxygenation, by looking at 2928 ICU patients on high levels of supplemental oxygen and targeting a paO2 of 60 mm Hg (low oxygen group) vs paO2 of 90 mm Hg (high oxygen group). There was no difference in mortality, or other significant difference in outcomes.
Bottom Line: A lower paO2 goal of 60 (correlates to an O2 sat of 90%) is noninferior to a higher paO2 goal of 90 (O2 sat of approximately 96%). When titrating oxygen, targeting a pulse ox of 90-96% is reasonable in critically ill patients. Be sure to include an upper limit on the sat goal, beware an O2 sat of 100%, and titrate down supplemental oxygen when the spO2 is above goal, as the paO2 may be dangerously high.
Schjørring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, Bäcklund M, Keus F, Laake JH, Morgan M, Thormar KM, Rosborg SA, Bisgaard J, Erntgaard AES, Lynnerup AH, Pedersen RL, Crescioli E, Gielstrup TC, Behzadi MT, Poulsen LM, Estrup S, Laigaard JP, Andersen C, Mortensen CB, Brand BA, White J, Jarnvig IL, Møller MH, Quist L, Bestle MH, Schønemann-Lund M, Kamper MK, Hindborg M, Hollinger A, Gebhard CE, Zellweger N, Meyhoff CS, Hjort M, Bech LK, Grøfte T, Bundgaard H, Østergaard LHM, Thyø MA, Hildebrandt T, Uslu B, Sølling CG, Møller-Nielsen N, Brøchner AC, Borup M, Okkonen M, Dieperink W, Pedersen UG, Andreasen AS, Buus L, Aslam TN, Winding RR, Schefold JC, Thorup SB, Iversen SA, Engstrøm J, Kjær MN, Rasmussen BS; HOT-ICU Investigators. Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. N Engl J Med. 2021 Jan 20. doi: 10.1056/NEJMoa2032510. Epub ahead of print. PMID: 33471452.
Category: Critical Care
Posted: 2/2/2021 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Mechanical Ventilation in COPD
Demoule A, et al. How to ventilate obstructive and asthmatic patients. Intensive Care Med. 2020; 46:2436-2449.
Category: Critical Care
Posted: 1/19/2021 by Lindsay Ritter, MD
Click here to contact Lindsay Ritter, MD
| Ever wonder what to tell the families regarding prognosis of the sickest COVID-19 patients you intubate in the ED or ICU? Introduction: Case fatality rates (CFR) for COVID-19 patients requiring invasive mechanical ventilation have been widely variable. A study in the Blue Journal (AJRCCM) examined patients requiring intubation in a systemic review and meta-analysis. The case fatality risk of an infection is represented by the proportion of patients who die among all infected cases in a population over a period of time. Methods: 69 studies axross 23 countries for a total of 57,420 patients with COVID-19 who required mechanical ventilation were included in analysis. Results: Overall case fatality rate was 45%, or about 1 death for every two intubated patients.. Among studies that included age stratification, pooled estimates of CFR were 47.9% in patients <40 (CI 46.4-49.4%) and 84.4% in patients >80 (CI 83.3-85.4%). Overall heterogeneity is high (I 2 .90%), In early COVID epicenters, CFR was 70% among patients aged more than 60 years of age. CFR increased exponentially with increasing age. Specifically in the US across 21 studies (3,811 intubated patients), CFR was 47% (95% CI, 36–57%). Studies from New York reported a CFR of 54% (95% CI, 36–72%) whereas other regions in the United States reported a CFR of 41% (95% CI, 30–53%). Definitive hospital CFR (aka for those with hospital discharge outcomes, 13,120 patients) was 56% (CI 47-65%). Conclusion: Almost half of patients with COVID-19 receiving IMV died based on the reported CFR. The reported CFR was higher in older patients and in early pandemic epicenters, which may be influenced by limited ICU resources. Limitations: Overall CFR of 45% still included patients in the hospital. Definitive hospital outcomes were only for 13,120 patients (36.6%). Significant variation in CFR exists between studies. |
Lim ZJ, Subramaniam A, Ponnapa Reddy M, Blecher G, Kadam U, Afroz A, Billah B, Ashwin S, Kubicki M, Bilotta F, Curtis JR, Rubulotta F. Case Fatality Rates for Patients with COVID-19 Requiring Invasive Mechanical Ventilation. A Meta-analysis. Am J Respir Crit Care Med. 2021 Jan 1;203(1):54-66.
Angriman F, Scales DC. Estimating the Case Fatality Risk of COVID-19 among Mechanically Ventilated Patients. Am J Respir Crit Care Med. 2021 Jan 1;203(1):3-4.
Category: Critical Care
Keywords: COVID-19, Awake proning, intubation (PubMed Search)
Posted: 1/12/2021 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
A single center (Nebraska, USA), retrospective analysis investigated the prevalence of intubation during hospital stay for 105 patients who had COVID-19 between March 24 to May 5, 2020 (1). 40 patients underwent awake proning vs. 60 patients did not undergo awake proning.
After adjusting for either SOFA or APACHE scores, patients with awake proning were associated with lower Hazard Ratios of intubation for SOFA (HR 0.30, 95% CI 0.09-0.96, p=0.043) and APACHE (HR 0.30, 95%CI 0.1-0.91, p=0.034).
Discussion
While this US study seemed promising, another Brazilian study being published earlier in July 2020 showed no difference in the prevalence of intubation between COVID-19 patients with proning or without proning (2).
These 2 studies highlighted the nature of this disease: high practice variability, uncertainty of therapeutic modalities. However, the complications from awake proning had been very low.
Conclusion:
Awake proning for hypoxic COVID-19 patients is a promising intervention but we will need more studies. In the meanwhile, we can try this therapeutic modality as the risk is low.
Category: Critical Care
Posted: 1/6/2021 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Study Question: What is the association of relative hypotension (degree and duration of MPP deficit) in patients with vasopressor-dependent shock with the incidence of new significant AKI and major adverse kidney events (MAKE)?
Methods:
Results:
Take-aways:
Panwar R, Tarvade S, Lanyon N, et al. Relative hypotension and adverse kidney-related outcomes among critically ill patients with shock. A multicenter, prospective cohort study. Am J Respir Crit Care Med. 2020;202(10):1407-1418.
Category: Critical Care
Posted: 12/8/2020 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
PEEP in the Intubated Obese Patient
De Jong A, et al. How to ventilate obese patients in the ICU. Intensive Care Med. 2020; 46:2423-35.
Category: Critical Care
Keywords: vasopressor, peripheral IV, safety (PubMed Search)
Posted: 11/17/2020 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
Summary
Our group performed a meta-analysis to assess whether it is safe to infuse vasopressor through peripheral venous catheters. We identified 9 studies with a total of 1835 patients. The prevalence of complications among the pooled patient population was 9%. Up to 96% of the complications was extravasation and almost no complications required any treatment.
A few studies reported safe infusion of norepinephrine up to 0.1 mcg/kg/min for up to 24 hours.
In exploratory meta-regression, catheter size 20 or larger was negatively associated with the rate of complications.
We also observed that studies that were published within the past 5 years reported significantly lower rate of complications from older studies. This suggested that with careful planning and monitoring, it is safe to start vasopressor through peripheral IV.
Limitation
most of the included studies were observational. No studies had enough power to statistically analyze any variables that could predict complications.
Bottom line: we should start vasopressor as soon as indicated, if we have good, reliable IV access.
Complication of vasopressor infusion through peripheral venous catheter: A systematic review and meta-analysis
Quincy K Tran, Gaurika Mester, Vera Bzhilyanskaya, Leenah Z Afridi, Sanketh Andhavarapu, Zain Alam, Austin Widjaja, Brooke Andersen, Ann Matta, Ali Pourmand.
Am J Emerg Med. 2020 Sep 28;S0735-6757(20)30842-1. doi: 10.1016/j.ajem.2020.09.047. Online ahead of print.
