Category: Toxicology
Keywords: Methemoglobenima, methylene blue, adverse effects (PubMed Search)
Posted: 5/21/2014 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Methylene blue is an extremely effective antidote for acquired methemoglobinemia but has important adverse effects if given in excess of recommended dose.
Below is the usual dose of methylene blue for treatment of methemoglobinemia
1-2 mg/kg of 1% solution IV with a repeat dose given if there is inadequate response to the first one
Adverse effects include:
Lo, J et al. A review of methylene blue treatment for cardiovascular collapse. 2014 J Emerg Med 46(5):670-679.
Category: International EM
Keywords: Mesoamerican, Nephropathy, Central America, Nicaragua, El Salvador, (PubMed Search)
Posted: 5/21/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Area of the world affected:
Relevance to the US physician:
Bottom Line:
University of Maryland Section of Global Emergency Health
Author: Emilie J.B. Calvello, MD, MPH & Alex Skog
Correa-Rotter R, Wesseling C, Johnson RJ. CKD of unknown origin in Central America: the case for a Mesoamerican nephropathy. Am J Kidney Dis. 2014 Mar;63(3):506–20.
Category: Critical Care
Keywords: Carbapenem Resistant Organisms, CRE, Pseudomonas, Infectious Diseases, Antimicrobial Stewardship (PubMed Search)
Posted: 5/15/2014 by John Greenwood, MD
(Updated: 5/20/2014)
Click here to contact John Greenwood, MD
We've all heard Dr. Bryan Hayes warn us that, "Vanc & Zosyn is NOT the Answer for Everything" but things just got a little more serious, on a whole 'nother level...
Within the past few months, 2 cases of NDM-producing carbapenem-resistant pseudomonas have been reported in the area - one in Delaware and one in Pennsylvania. Previously, the only reported cases were found in Europe.
Few treatment options are currently available for carbapenem resistant organisms.
Appear to have retained some in vitro activity against these organisms, but are generally used as, "drugs of last resort".
Know it exists, take a good history, & know your local antibiogram. Prior to selecting a broad spectrum antimicrobial regimen, try to obtain previous antimicrobial culture data for patients with resistant organism infectious risk factors.
For more critical care pearls, follow me on Twitter: @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 5/19/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A patient presents with the rash shown below and is treated with penicillin. Fever, headache, and myalgia develop four hours later. What’s the diagnosis?

Answer: Jarisch-Herxheimer reaction
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: lisfranc, fracture (PubMed Search)
Posted: 5/17/2014 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
Lisfranc Fracture:
Typically consists of a fracture of the base of the second metatarsal and dislocation, though it can also be associated with fractures of a cuboid. Common current mechanism of injury is when a person steps into a hole and twists the foot. The original mechanism of injury that was described was when a horseman would fall of their horse with their foot still trapped in a stirrup.
Diagnosis should be considered if patient has difficultly weight bearing with pain on palpation over the 2nd and 3rd metacarpal head with an appropriate mechanism.
Pearls:

Category: Pediatrics
Keywords: Psychiatric clearance, pediatric (PubMed Search)
Posted: 5/16/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Mental health-related visits account for 1.6–6% of ED encounters. Patients with acute psychosis are often brought to the ED for clearance prior to psychiatric evaluation. Is this necessary?
Background: Several adult studies have shown that only 0–4% of patients with isolated psychiatric complaints have organic diagnoses requiring urgent treatment. Routine ED laboratory testing in adults is low yield still, with one study identifying abnormalities in only 2 of 352 patients—both mild hypokalemia. A pediatric study found that 207 of 209 patients were medically cleared.
This study was a retrospective review of pediatric psychiatric patients presenting to a an urban California hospital. They examined 798 patients who had an involuntary psychiatric hold placed by a psychiatric mobile response team.
The authors concluded that few pediatric patients brought to the ED on an involuntary hold required a medical screen and perhaps use of basic criteria in the prehospital setting to determine who required a medical screen (altered mental status, ingestion, hanging, traumatic injury, unrelated medical complaint, sexual assault) could have led to significant savings.
Santillanes, G et al. Is Medical Clearance Necessary for Pediatric Psychiatric Patients? J Emerg Med. 2014 Mar 15. pii: S0736-4679(13)01455-8. [Epub ahead of print]
Category: Toxicology
Keywords: dabigatran, dabigatran-Fab, PCC (PubMed Search)
Posted: 5/14/2014 by Hong Kim, MD
Click here to contact Hong Kim, MD
Currently, no effective reversal agent for new oral anticoagulants (e.g. direct thrombin inhibitor, dabigatran, and factor Xa inhibitors: rivaroxaban and apixaban) exists for emergent management of hemorrhagic complications.
Boehringer Ingelheim, the manufacturer of dabigatran, is developing an antibody fragment (Fab) against dabigatran as a reversal agent.1
A small ex-vivo porcine study demonstrated partial reversal of anticoagulation effects, measured by PT, aPTT, clotting time, clot formation time and maximum clot firmness, of dabigatran by PCC and activated PCC, while dabigatran-Fab achieved complete reversal. Recombinant fVIIa did not reverse the anticoagulation effect of dabigatran.2
Caution should be exercised when interpreting these finding as reversal of laboratory values does not necessarily correlate with clinical effect/outcome. However, dabigatran-Fab holds promise as an effective reversal agent of dabigatran.
Dabigatran-Fab is still under development and is not available/approved for clinical use.
Category: International EM
Keywords: rabies, global, video, international, infectious disease (PubMed Search)
Posted: 5/14/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Clinical Presentation
Rabies is, initially, a clinical diagnosis. To see what a patient with rabies looks like, check out this 3 minute YouTube video: (There is a bit of commentary by the person who posted it at the beginning that you might want to skip through.)
https://www.youtube.com/watch?v=EZbrNN9KeUI
Bottom Line
Rabies, while a rare disease in the US, can occur through either contact with infected animals (especially while traveling) or via organ transplantation. Recognizing the clinical syndrome is key to diagnosis.
University of Maryland Section for Global Emergency Health
Author: Andi Tenner, MD, MPH, FACEP
http://www.cdc.gov/rabies/location/usa/surveillance/human_rabies.html
Category: Critical Care
Posted: 5/13/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Prior literature has demonstrated the safety and feasibility of placing subclavian lines with ultrasound guidance; here's a link to a short educational video describing the technique.
The literature has been varied, however, as to which approach is best for venous cannulation with ultrasound; the supraclavicular (SC) or infraclavicular (IC) approach (see references below)
A recent study evaluated both approaches in healthy volunteers in order to determine which approach is superior for cannulation using ultrasound.
98 patients were prospective evaluated by Emergency Medicine physicians with training in ultrasound. In each patient, both SC and IC views were evaluated on both the left and right sides; each view was given a grade for ease of favorability (no patients were actually cannulated)
Overall, it was found that the SC view was significantly more favorable compared to the IC view; the right SC was non-significantly preferred compared to the left SC.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Stachura, M. et al. A Comparison of the Supraclavicular and Infraclavicular Views for Imaging the Subclavian Vein with Ultrasound. The American Journal of Emergency Medicine (in press)
Fragou, M., Gravvanis, A., and Vasilios, D. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study. Crit Care Med. 2011; 39: 1607–1612
Mallin, M., Louis, H., and Madsen, T. A novel technique for ultrasound-guided supraclavicular subclavian cannulation. Am J Emerg Med. 2010; 28: 966–969
Czarnik, T., Gawda, R., Perkowski, T. et al. Supraclavicular approach is an easy and safe method of subclavian vein catheterization even in mechanically ventilated patients. analysis of 370 attempts. Anesthesiology. 2009; 111:334–339
Category: Orthopedics
Keywords: Concussion, recovery, head injury (PubMed Search)
Posted: 4/6/2014 by Brian Corwell, MD
(Updated: 5/10/2014)
Click here to contact Brian Corwell, MD
Risk Modifiers for Concussion and Prolonged Recovery
A history of prior concussion is a risk factor for future concussion (>2x risk).
For individual sports, boxing has the highest risk.
For team sports, football, ice hockey and rugby have the highest risk.
Women’s soccer confers the highest risk for female athletes.
Younger age confers increased risk.
Female sex confers higher risk when comparing similar sports with similar rules.
Those with migraine headaches may be at increased risk.
Risk of prolonged concussion
Most athletes have symptom resolution within one week
Post traumatic amnesia (both retrograde and anterograde) predict increased number and longer duration of symptoms.
Younger age also predicts pronged recovery.
Other studies have found associations with headache lasting greater than 60 hours, fatigue, “fogginess,” or greater than 3 symptoms at initial presentation. Cognitive studies have identified deficits in visual memory and process speed as predictors of prolonged recovery.
Risk modifiers for concussion and prolonged recovery.
Sports Health. 2013 Nov;5(6):537-41
Category: Toxicology
Keywords: dexmedetomidine, cocaine, sympathomimetic (PubMed Search)
Posted: 5/6/2014 by Bryan Hayes, PharmD
(Updated: 5/8/2014)
Click here to contact Bryan Hayes, PharmD
A placebo-controlled treatment trial in 26 cocaine-addicted subjects aimed to determine whether dexmedetomidine reverses MAP and HR increases after intranasal cocaine (3 mg/kg).
In a low nonsedating dose, dexmedetomidine may be a potential (adjunct) treatment for cocaine-induced acute hypertension. However, higher sedating doses can increase blood pressure unpredictably during acute cocaine challenge and should be avoided.
Generous benzodiazepine should remain first-line therapy.
Kontak AC, et al. Dexmedetomidine as a Novel Countermeasure for Cocaine-Induced Central Sympathoexcitation in Cocaine-Addicted Humans. Hypertension 2013;61(2):388-94. [PMID 23283356].
Follow me on Twitter (@PharmERToxGuy) and Google Plus (+bryanhayes13)
Category: International EM
Keywords: Polio, Vaccine, Eradication (PubMed Search)
Posted: 5/7/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Relevance to the EM Physician:
Bottom Line:
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD
Category: Critical Care
Keywords: HFNC, vapotherm, high flow, nasal cannula, hypoxemia (PubMed Search)
Posted: 5/7/2014 by Feras Khan, MD
(Updated: 2/2/2026)
Click here to contact Feras Khan, MD
High Flow Nasal Cannula
What is it?
Benefits
Who to use it on
How to set it
-15-30 L per minute
-100% oxygen (wean as tolerated)
-temp 35-40 C
-when weaning decrease oxygen prior to flow
Bottom line: No evidence that it reduces intubation rates in patients with hypoxemic respiratory failure but may improve oxygenation issues while deciding on treatment options
Clinical evidence on high flow oxygen therapy and active humidification in adults
C. Goteraa, S. Di az Lobatoa,∗, T. Pintob, J.C. Winckb
March 2013, Portugese Journal of Pulmonology
Category: Visual Diagnosis
Posted: 5/5/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The clip below demonstrates normal right femoral anatomy. The structure with the asterisk is the right common femoral vein and the arrow is pointing to a branch of the right femoral vein. What is the name of the branch and what is its importance during lower extremity ultrasound?
Answer: Greater Saphenous Vein; it is one of the two regions that should be compressed when evaluating for a lower extremity DVT in the Emergency Department (the other is at the trifurcation of the popliteal vein).
Here is a podcast from the Ultrasound Podcast describing the entire bedisde DVT exam http://www.ultrasoundpodcast.com/2011/08/dvt/
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)a
Category: Pharmacology & Therapeutics
Keywords: dexmedetomidine, alcohol, ethanol, withdrawal (PubMed Search)
Posted: 4/28/2014 by Bryan Hayes, PharmD
(Updated: 5/3/2014)
Click here to contact Bryan Hayes, PharmD
Four small case series (one prospective, 3 retrospective) have concluded that dexmedetomidine (Precedex) may be a useful adjunct therapy to benzodiazepines for ethanol withdrawal in the ED or ICU. They are summarized on the Academic Life in EM blog.
A new randomized, double-blind trial evaluated 24 ICU patients with severe ethanol withdrawal.
Group 1: Lorazepam + placebo
Group 2: Lorazepam + dexmedetomidine (doses of 0.4 mcg/kg/hr and 1.2 mcg/kg/hr).
Mueller SW, et al. A randomized, double-blind, placebo-controlled, dose range study of dexmedetomidine as adjunctive therapy for alcohol withdrawal. Crit Care Med 2014;42(5):1131-9. [PMID 24351375]
Follow me on Twitter (@PharmERToxGuy) and Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: prescription drug abuse (PubMed Search)
Posted: 5/1/2014 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
A recent article showed that District of Columbia's Prescription Drug Monitoring program (PDMP) did not change the amount of opioids prescribed after conversion to MMEs (mg morphine equivalents). It is surprising to see a varying effect of PDMPs across the USA. Some have seen dramatic decreases up to 60% in Colorado versus an actual increase of over 50% in Connecticut. Usability, lack of interstate connectivity and quality of information have been seen as rate limiting factors in the efficacy of PDMPs.
PDMPs, by themselves, are not the answer to prescription drug abuse but are an excellent adjunct. Maryland ACEP and a committee chaired by Dr. Suzanne Doyon, Director of the Poison Center, have developed Opioid Prescribing Guidelines and a Discharge pamphlet that can utilized by hospitals to assist with this epidemic. The guidelines and pamphlet have been endorsed by MDPCC, MDACEP, DHMH and a multitude of other Maryland state agencies. I have attached the guidelines.
Prescription drug monitoring and dispensing of prescription opioids.
Brady JE, Wunsch H, DiMaggio C, Lang BH, Giglio J, Li G.
Public Health Rep. 2014 Mar-Apr;129(2):139-47.
Category: International EM
Keywords: Seizure, International, Valproate (PubMed Search)
Posted: 4/30/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Background Information:
ACEP has recently revised its 2004 policy on critical issues in the evaluation and management of adult patients with seizures in the emergency department.
Pertinent Study Design and Conclusions:
Bottom Line:
As an alternative to phenytoin or fosphenytoin, valproate may be considered for refractory convulsive status epilepticus if benzodiazepines fail.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
Category: Critical Care
Posted: 4/29/2014 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Antibiotic Timing in Severe Sepsis/Septic Shock
Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med 2014. [epub ahead of print]
Category: Visual Diagnosis
Posted: 4/28/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
66 year-old female presents with one week of epigastric and right flank pain. Urinalysis was normal. What’s the diagnosis?

Answer: Choledocholithiasis with pancreatitis secondary to 2.2 cm common bile duct stone
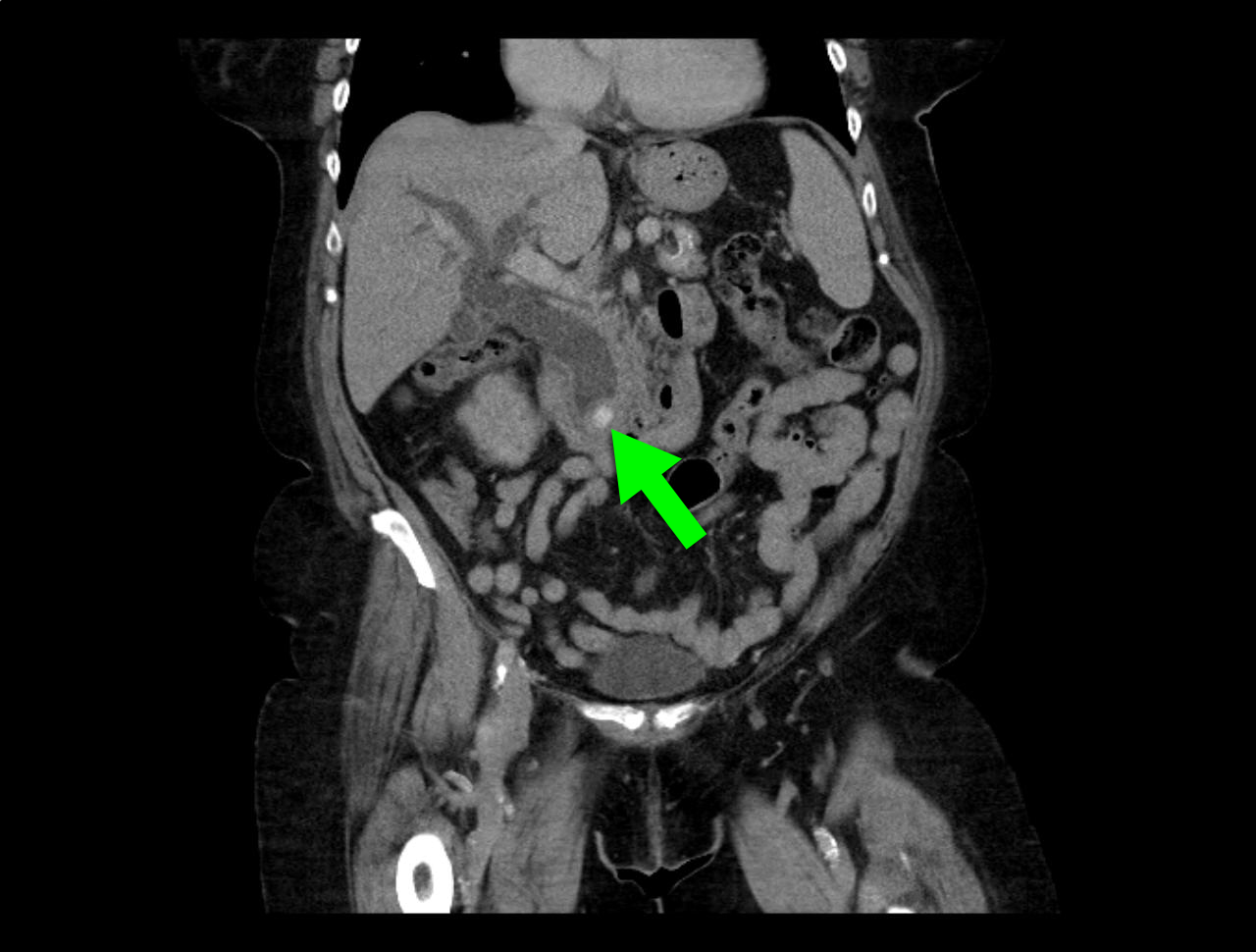
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Brain-heart syndrome, Neurogenic Stress Cardiomyopathy (PubMed Search)
Posted: 4/27/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
