Category: Critical Care
Keywords: accidental hypothermia, rewarming, ecmo, artic sun (PubMed Search)
Posted: 2/11/2014 by Feras Khan, MD
(Updated: 2/2/2026)
Click here to contact Feras Khan, MD
A 50yo man found dow in the snow was brought into our ER last week in cardiac arrest with a bladder temperature of 21° C. Let’s warm him up!
We were able to get ROSC with CPR and ACLS and then used Artic Sun to re-warm successfully.
Other tips/tricks:
Category: Visual Diagnosis
Posted: 2/9/2014 by Haney Mallemat, MD
(Updated: 2/10/2014)
Click here to contact Haney Mallemat, MD
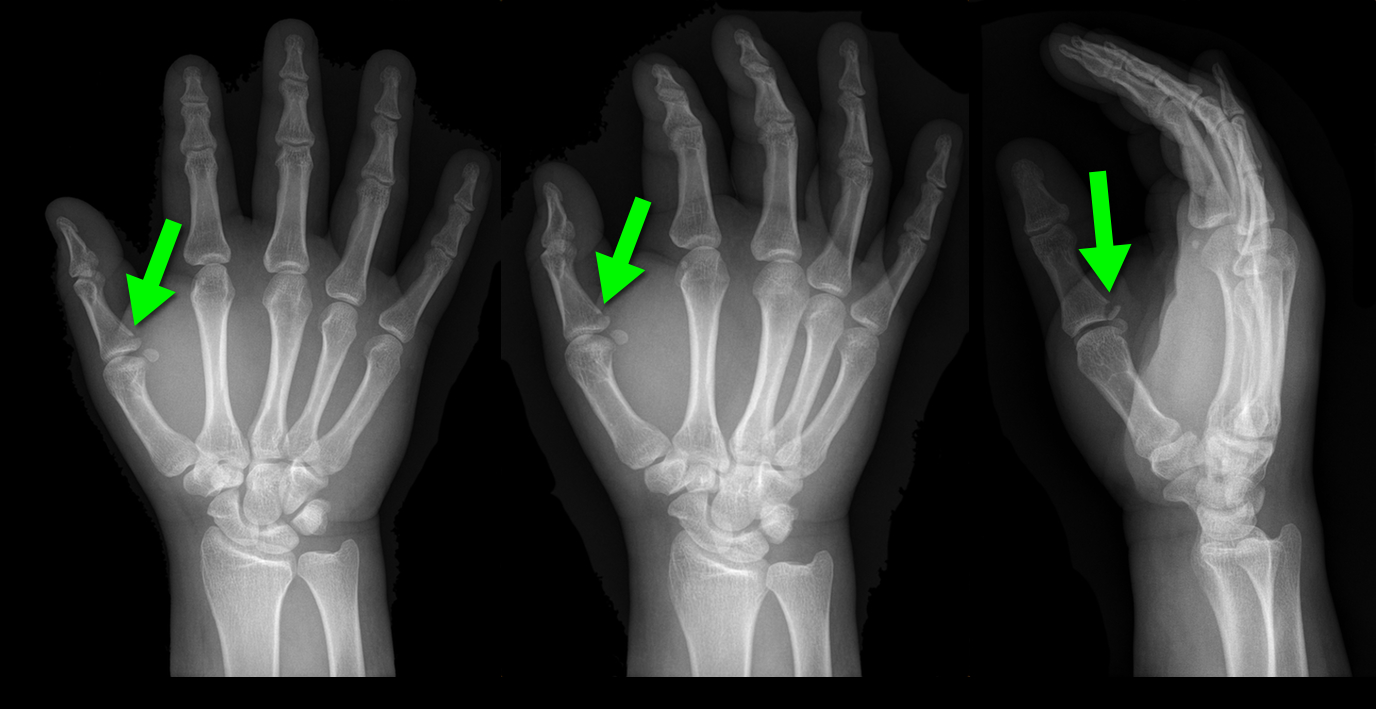
25 year-old male presents after falling off his bicycle. He complains of pain in his right-hand (he is right-hand dominant). What's the diagnosis?

Answer: Gamekeeper's thumb or Skier's thumb
Injury to the ulnar collateral ligament (UCL) secondary
Called “Gamekeeper Thumb” because injury was originally described in gamekeepers who job was to break the necks of captured game (or animals). The act of breaking necks led to a repetitive stress and injury secondary to the valgus forces on the thumb.
UCL can become torn or avulsed from the insertion on the proximal phalanx; the UCL is an important stabilizer of the thumb; improper management can lead to future disability.
Treatment is with a short-arm thumb-spica cast and follow up with a hand surgeon to determine whether management will be conservative or operative.
Chuter GS, Muwanga CL, Irwin LR (June 2009). "Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience". Injury 40 (6): 652–6 Wheeless' Textbook of Orthopaedics Online: Surgical treatment of acute gamekeeper's thumb
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: ECG, STEMI, aVL (PubMed Search)
Posted: 2/9/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
The importance of new ST-segment depressions (STD) and/or T wave inversions (TWI) in lead aVL have not been emphasized or well recognized across specialties. Computer-assisted ECG readings typically report these findings as normal or nonspecific.
There is growing evidence that changes in lead aVL are abnormal, and that paying attention to that lead can be clinically useful. Reciprocal changes presenting as STD or TWI in lead aVL may be indicative of a significant coronary artery lesion and can sometimes be the only ECG manifestation of acute MI.
STD in lead aVL is considered a sensitive marker for early inferior STEMI, and has been shown to help differentiate STEMI from pericarditis. Another recent retrospective study suggests that TWI in aVL might be associated with significant LAD lesions.
Bottom Line: Paying close attention to subtle changes and abnormalities in lead aVL may help in early identification and initiation of therapy for patients who are having an acute MI.
Hassen GW, Costea A, Smith T, et al. The Neglected Lead on Electrocardiogram: T Wave Inversion in Lead aVL, Nonspecific Finding or a Sign for Left Anterior Descending Artery Lesion?. Journal of Emergency Medicine. 2014;46(2):165–170.
Category: Orthopedics
Keywords: Overtraining syndrome, exercise (PubMed Search)
Posted: 2/8/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Overtraining syndrome
A maladaptive response to excessive exercise without adequate functional rest
-Results in disturbances of multiple body systems (neurologic, endocrinologic, immunologic and psychologic).
- May be caused by systemic inflammation and resultant neurohormonal changes
- Multiple hypotheses exist
-Symptoms
Parasympathetic alterations: fatigue, depression, bradycardia
Sympathetic alterations: insomnia, irritability, agitation, tachycardia, hypertension, restlessness
Other: anorexia, weight loss, poor concentration, anxiety
Usual presentation is prolonged underperformance despite adequate rest and recovery (weeks to months).
Category: Pediatrics
Posted: 2/7/2014 by Rose Chasm, MD
(Updated: 2/2/2026)
Click here to contact Rose Chasm, MD
Cruz AT, Perry AM, Williams EA, et al. Implementaion of Goal-Directed Therapy for Children With Suspected Sepsis in the Emergency Department. Pediatrics 2011;127;e758.
Category: Toxicology
Keywords: ondansetron, dystonia (PubMed Search)
Posted: 2/6/2014 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
Ondansetron (Zofran) is a great anti-emetic that, since it has gone generic, is also inexpensive. High dose ondansetron has been reported to cause QT prolongation and that practice is largerly discontinued now in the oncology world. Another uncommon adverse drug reaction may be dystonia. Though we think of ondansetron as a 5-HT3 blocker and should not cause the dystonic reaction like we see in metoclopramide, there are case reports of this reaction occurring.
Category: Pharmacology & Therapeutics
Keywords: anterior epistaxis, tranexamic acid, antifibrinolytic (PubMed Search)
Posted: 2/6/2014 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Tranexamic Acid (TXA) topically applied was compared to anterior nasal packing in 216 patients with acute anterior epistaxis. Cotton pledgets (15 cm) soaked in injectable TXA (500 mg/5 ml) were inserted into the bleeding nostril and removed after bleeding had arrested. This was compared to standard anterior packing.
RESULTS
| TXA Anterior packing |
| % pts bleeding stopped in 10 min: 71% 31.2% |
| Discharge after 2 hours 95.3% 6.4% |
| Rebleeding in 24 h hours 4.7% 11% |
| Satisfaction scores 8.5 4.4 |
Bottom line: topical tranexamic acid looks promising for control of uncomplicated anterior epistaxis.
Zahed R, Moharamzadeh P, AlizadeArasi S, Ghasemi A, Saeedi M. A new and rapid method for epistaxis treatment using injectable form of tranexamic acid topically: a randomized controlled trial. AJEM 2013 (31):1389-92.
Category: International EM
Keywords: road traffic accidents, international, global, public health (PubMed Search)
Posted: 2/5/2014 by Andrea Tenner, MD
(Updated: 2/2/2026)
Click here to contact Andrea Tenner, MD
General Information:
Area of the world affected:
Relevance to the US physician:
Bottom Line:
VRU traffic injuries are the greatest challenge of today's worldwide road safety.
University of Maryland Section of Global Emergency Health
Author: Terrence Mulligan DO, MPH
http://www.who.int/gho/road_safety/en/
http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1000228
http://www.grsproadsafety.org/our-knowledge/safer-road-users/vulnerable-road-users
Category: Critical Care
Keywords: VV-ECMO, mechanical ventilation, ultra-lung protective ventilation (PubMed Search)
Posted: 2/4/2014 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Mechanical Ventilation During ECMO
Schmidt M, et al. Mechanical ventilation during extracorporeal membrane oxygenation. Crit Care 2014;18:203.
Category: Visual Diagnosis
Posted: 2/3/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
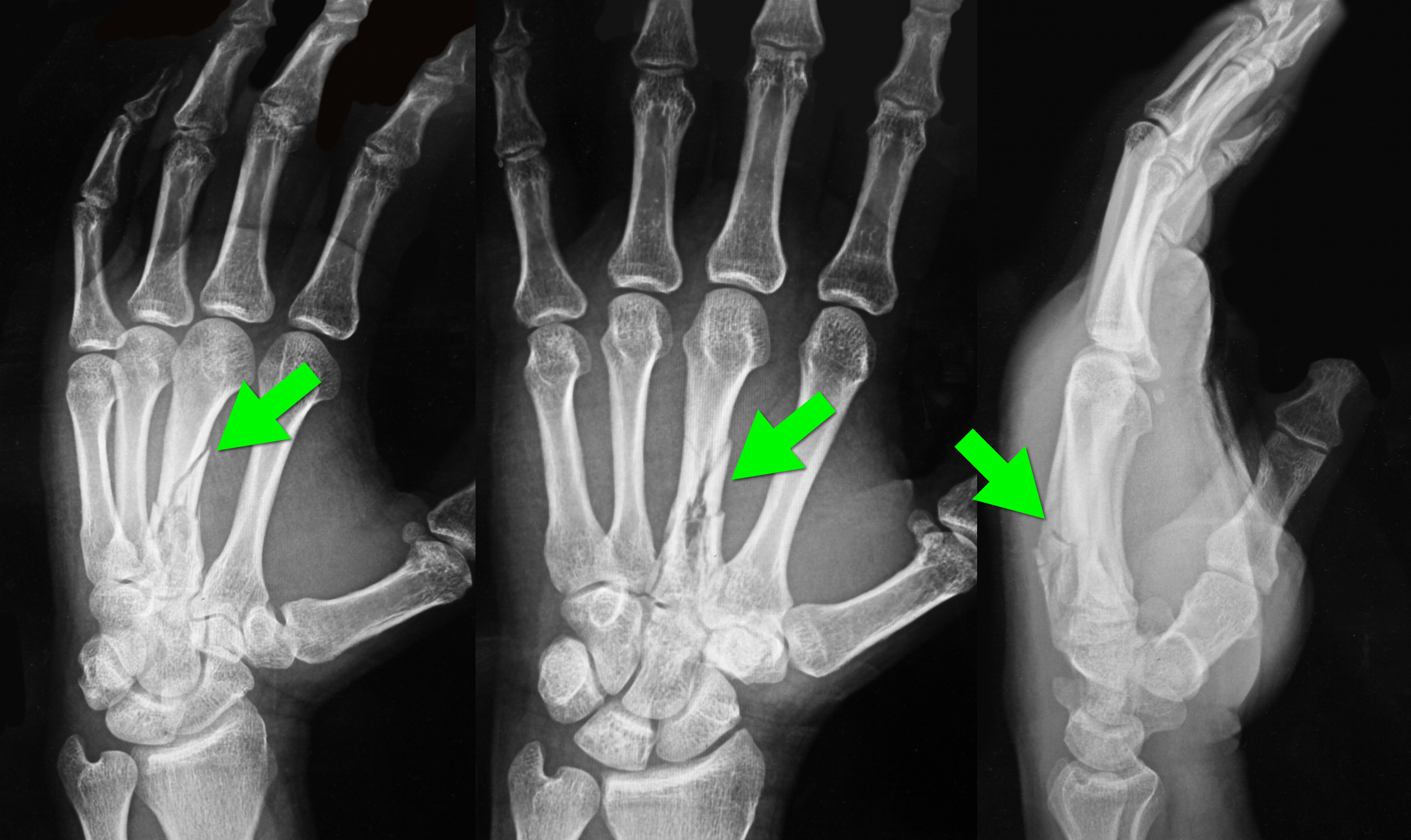
34 year-old left-hand dominant male sustained injury to left hand after his pressurized greasing-gun discharged into the palm of his hand. He has a small lac to the hand but is in extreme pain. On exam his hand is very puffy and he is neurovascularly intact (XR below) What is the next step in management?

Metacarpal fracture; emergent surgical consult is required
High-Pressure Injection Injuries (HPI) injuries
HPI devices (e.g., grease, paint guns, etc.) may cause injury when the device accidently discharges, typically into the operator’s dominant hand during attempts to clean the nozzle.
Injuries may initially appear benign, however injuries should be considered surgical emergencies because they often require debridement / washout of materials injected into deeper tissues.
Tissue damage is multi-factorial and includes direct injury (e.g., high-pressure tissue damage, vascular compression, etc.) and indirect injury from material injected into tissues (e.g., chemical inflammation / injury, granuloma formation, deep-tissue infections, etc.).
Radiographs may assist surgical planning by identifying subcutaneous air, debris, or unanticipated fractures.
Treatment:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 2/2/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Myocardial Infarction in Women After Childbirth
World Health Organization reports that obesity is the 5th leading cause of global death with the highest impact on women <65 years of age
The association of obesity and cardiovascular risk in young women is currently being researched
A recent nationwide cohort looking at obesity and future cardiovascular risk looked at Danish women giving birth (2004-2009) and followed them a median time of 4.5 years
This study grouped women via pre-pregnancy body mass index (BMI)
1. Underweight (BMI <18.5)
2. Normal weight (BMI <25)
3. Overweight (BMI <30)
4. Obese (BMI >30)
Data revealed that healthy women of fertile age, pre-pregnancy obesity alone was associated with increased risk of myocardial infarction in the years after childbirth
Schmiegelow M, Andersson C, Kober L, et al. Prepregnancy Obesity and Associations With Stroke and Myocardial Infarction in Women in the Years After Childbirth. Circulation 2014;129:330-337.
Category: Pharmacology & Therapeutics
Keywords: methadone, withdrawal (PubMed Search)
Posted: 1/23/2014 by Bryan Hayes, PharmD
(Updated: 2/1/2014)
Click here to contact Bryan Hayes, PharmD
In most situations (dependant on state laws and institutional policies), methadone-maintained patients enrolled in a drug abuse program are best managed by continuing methadone at the usual maintenance levels with once-a-day oral administration.
Pearl: In the event the methadone clinic is closed and/or the dose cannot be verified, 30-40 mg (10-20 mg IM) is generally enough to prevent withdrawal in most patients.
This is only a short-term measure and some patients may require additional methadone. Full doses of methadone should be reinstituted as soon as possible.
Fultz JM, et al. Guidelines for the management of hospitalized narcotic addicts. Ann Intern Med 1975;82(6):815-8. [PMID 1138596]
Alford DP, et al. Acute pain management for patients receiving maintenance methadone or buprenorpine therapy. Ann Intern Med 2006;144(2):127-34. [PMID 16418412]
Freedman DX, et al. Methadone treatment of heroin addiction. Annu Rev Med 1973;24:153-64. [PMID 4575849]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: dexmedetomidine, alcohol withdrawal (PubMed Search)
Posted: 1/30/2014 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
Category: International EM
Keywords: Virus, Fever, West Nile, Dengue (PubMed Search)
Posted: 1/29/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Case Presentation: A 63 year old woman from Texas with no recent international travel presents to the ED with persistent fatigue which onset a month ago and is associated with anorexia and occasional fevers and chills. She has been to her family doctor who tested her for a number of viral illnesses and was told she had West Nile virus.
Clinical Question:
What other febrile illness could this be?
Answer:
This patient had dengue. Dengue is now endemic in the US, and locally-acquired cases have been reported in Florida, Texas and Hawaii. The fatigue and anorexia are typical and can last for weeks after other symptoms have resolved.
West Nile virus testing may be falsely positive when another flavivirus is present such dengue, yellow fever or Japanese encephalitis.
Bottom Line:
Other possible illnesses like dengue should be considered in patients who have tested positive for West Nile virus.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD, MPH
Sharp TM, et al. Fatal hemophagocytic lymphohistiocytosis associated with locally acquired dengue virus infection - New Mexico and Texas, 2012. MMWR Morb Mortal Wkly Rep. 2014 Jan 24;63(3):49-54. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6303a1.htm?s_cid=mm6303a1_w
Centers for Disease Control and Prevention. Dengue and Dengue Hemorrhagic Fever: Information for Health Care Practitioners. http://www.cdc.gov/dengue/resources/Dengue&DHF%20Information%20for%20Health%20Care%20Practitioners_2009.pdf
Category: Critical Care
Posted: 1/28/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
NSSTIs occur secondary to toxin-secreting bacteria; NSSTIs are surgical emergencies with a high-morbidity / mortality
Risk factors: immunocompromised host (DM, AIDS, etc.), intravenous drug use, malnourishment, peripheral vascular disease
Type I (polymicrobial; most common), Type II (monomicrobial; typically clostridia, streptococci, staph, or bacteroides), Type III (Vibrio vulnificus; seawater exposure)
Signs / Symptoms: pain out of proportion to exam (occasionally no pain at all), skin findings (blistering / bullae, gray-skin discoloration, or “Dishwater-like” discharge), or systemic toxicity (altered mental status, elevated lactate, etc.)
Diagnostic radiology
Treatment is emergent surgical debridement with simultaneous hemodynamic resuscitation PLUS broad-spectrum antibiotics; consider clindamycin becuase it has anti-toxin activity
Adjunctive therapies include Intravenous intraglobulin (neutralizes toxins secreted by bacteria) and hyperbaric oxygen
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/27/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
32 year-old with diabetes presents with fever, erythema, and warmth of his lower extremity; his leg is not particularly painful. He is diagnosed with cellulitis, started on antibiotics, and admitted to the hospital. While boarding in the Emergency Department he becomes rigorous and hypotensive. An ultrasound of his cellulitis is performed and is shown below. What’s the diagnosis?
"Cobblestoning" of subcutaneous tissue consistent with cellulitis. There are also areas of subcutaneous air raising the concern for necrotizing fasciitis.
Special thanks to Dr. Mike Mallin from the Ultrasound Podcast for the clip. Want to see more amazing ultrasound clips? Check out Sonocloud
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Wide complex tachycardia, ventricular tachycardia (PubMed Search)
Posted: 1/26/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
A 48 year old woman has acute chest pain and palpitations over the past several hours. She has felt similar palpitations in the past but never sought medical attention. She arrives to your ED alert and anxious. HR = 270, BP=130/100. ECG is below. What’s the diagnosis and treatment?
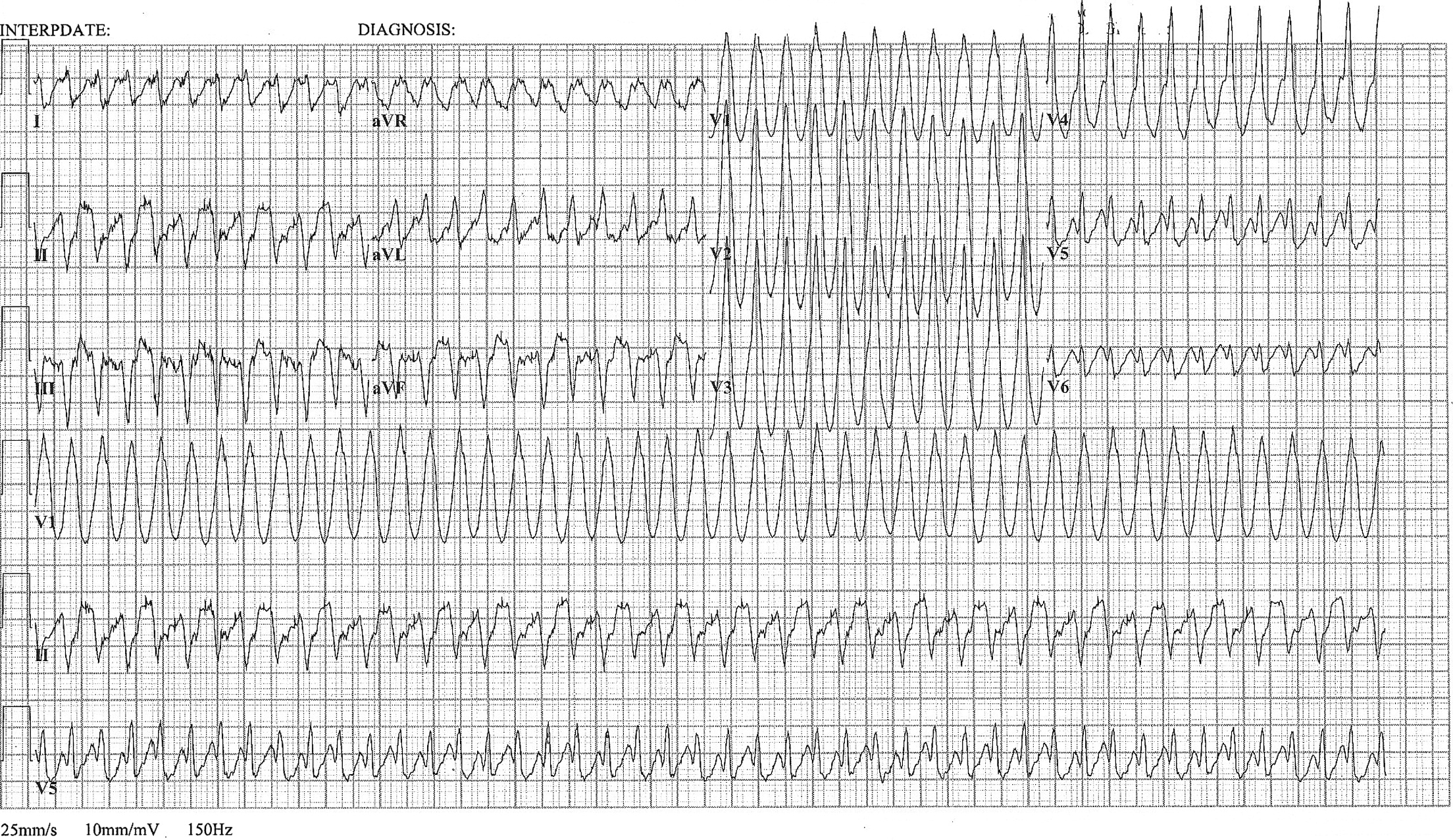
Most wide complex regular tachycardias are ventricular tachycardia (VT). However, supraventricular tachycardias can also cause wide complexes through aberrant conduction and accessory pathways.
Nelson JG, Zhu DW. Atrial Flutter with 1:1 Conduction in Undiagnosed Wolff-Parkinson-White Syndrome. The Journal of Emergency Medicine. January 2014. Pubmed Link
Category: Orthopedics
Keywords: MCL, knee, (PubMed Search)
Posted: 1/17/2014 by Brian Corwell, MD
(Updated: 1/25/2014)
Click here to contact Brian Corwell, MD
Pelllegrini-Stieda lesion
Ossified post-traumatic lesions at the MCL adjacent to the femoral attachment site of the medial femoral condyle.
Mechanism is likely from an avulsion injury that subsequently calcifies after the initial trauma.
Often an incidental finding on plain films.
If symptomatic, refer to ortho as an outpatient
If not symptomatic, no treatment is indicated
http://images.radiopaedia.org/images/30076/b62e61e83241e30f2da693901edcdc_gallery.jpg
http://www.imageinterpretation.co.uk/images/knee/PELLEGRINI%20STIEDA2.jpg
Category: Toxicology
Keywords: pharmacology (PubMed Search)
Posted: 1/23/2014 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
Everyone has admitted an altered mental status, patient or bradycardic patient and all of your test results are coming back normal except for a mild increase in creatinine. Take a look at the medication list. Creatinine is a poor indicator of renal function and GFR may be severely impaired even with a mild elevation of creatinine. If you have a predominantly renally excreted drug, you can see toxic effects of a drug even if administered at therapeutic levels.
Common bradycardia inducing medication that is renally cleared: atenolol (very high renal excretion) and digoxin (70%).
Altered Mental Status and on Keppra? Keppra is 100% renally cleared!
Ask your pharmacist for help with the medication list with renal or hepatic insufficiency.
Category: International EM
Keywords: International, snake, venom, (PubMed Search)
Posted: 1/22/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
98% of venomous snake bites in the US are due to pit vipers. Occasionally a snake bite is from an exotic venomous snake being kept as a pet. In 2005, 142 exotic poisonous snakes were reported to poison control. It can be very challenging to find antivenom for these exotic animals.
Antivenom is usually specific to a family or subfamily, so the snake must be identified. Most exotic snake owners will know the common name and possibly the scientific name of the animal.
The WHO database of venomous snakes can help with identification of the species and will list antivenom available globally.
Poison centers are essential to help locate the antivenom and assist with treatment.
Relevance to the EM Physician:
When a patient presents with an exotic snake envenomation, the WHO website below can be helpful to identify the species and possible antivenom.
http://apps.who.int/bloodproducts/snakeantivenoms/database/
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg
C Lubich and EP Krenzelok. Exotic snakes are not always found in exotic places: how poison centres can assist emergency departments.” Emerg Med J. 2007 November; 24(11): 796–797.
Melisa W. Lai, et al. 2005 Annual Report of the American Association of Poison Control Centers’ National Poisoning and Exposure Database. Clinical Toxicology, 44:803–932, 2006
http://www.who.int/neglected_diseases/diseases/snakebites/en/index.html
