Category: Trauma
Keywords: Stab wound, chest radiograph, pneumothorax (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
This small study from South Africa shows stab wounds to the chest with a pneumothorax less than 0.5 cm that were managed conservatively had completely resolved on 12 hour repeat chest X-ray. This could facilitate earlier discharge of these patients. It also supports conservative (non-tube placement) approach to asymptomatic small pneumothoraces from stab wounds.
Kong V, Cheung C, Lee D, et al. Defining the optimal timing of interval chest radiograph in conservatively managed small pneumothorax from thoracic stab wounds – a South African experience. Trauma. 2025;28(1):14-17. doi:10.1177/14604086251396434
Category: Geriatrics
Keywords: Tramadol, geriatrics (PubMed Search)
Posted: 1/29/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Tramadol has been viewed as a safer alternative for pain control than opioids. This study says differently.
“Tramadol use was associated with increased risk of multiple ER utilizations, falls/fractures, CVD hospitalizations, safety event hospitalizations, and mortality (new users only) compared to nonuse.”
Musich S, Wang SS, Schaeffer JA, Slindee L, Kraemer S, Yeh CS. Safety Events Associated with Tramadol Use Among Older Adults with Osteoarthritis. Popul Health Manag. 2021 Feb;24(1):122-132. doi: 10.1089/pop.2019.0220. Epub 2020
Category: Administration
Keywords: Communication, Teamwork (PubMed Search)
Posted: 1/28/2026 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
How well does your ED care team communicate? For some high yield strategies and reasons for improvement, read on…
To explore effective and ineffective communication in the ED and its impact of patient care, physician and nurses from several academic EDs completed an online anonymous survey, then attended focus group sessions. Responses highlighted the following themes:
1: Situations, built physical environment, and medium of communications all impact quality of communication.
2: Core elements of desired professional communication include respect, closed-loop communication, and attention, often conveyed through non-verbal behaviors.
3: Poor communication begets poor communication in later interactions
4: Effective communication is seen as fundamental to patient care but also has impacts beyond patient care
5: Clinician gender and gender dyads influence communication dynamics, age and experience dyads did not.
Do any of these themes resonate with you? What can you do within your department to improve physician-nurse communication and the care you provide?
Jones DC, Phillips J, Graveson A, et al. Emergency Physician and Emergency Nurse Communication in the Emergency Department: A Mixed-methods Study. West J Emerg Med. 2026;27(1)91–98.
Category: Critical Care
Keywords: OCHA, VF, ventricular fibrillation, cardiac arrest, shockable, Occult VF (PubMed Search)
Posted: 1/28/2026 by Kami Windsor, MD
(Updated: 2/1/2026)
Click here to contact Kami Windsor, MD
A crucial part of cardiac arrest management is identification of the underlying rhythm, with key aspects of management diverging depending whether shockable (pulseless ventricular tachycardia/pVT or ventricular fibrillation/VF) or unshockable (pulseless electrical activity/PEA or asystole).
A recent study prospectively evaluated adult atraumatic out-of-hospital-cardiac-arrests (OHCAs) presenting to the ED, to determine what percentage of cases had “Occult VF” – VF found point-of-care echocardiogram but not by ECG. The researchers only included cases with simultaneous ECG and echo assessments for the initial 3 pulse checks. Echo and ECG determinations for the study were adjudicated by research team members.
They found that:
Major limitations:
Bottom Line: Point-of-care echocardiogram continues to have value in the management of cardiac arrest, potentially changing management and affecting post-ROSC decisions. Ensuring high-quality CPR, with appropriate defibrillation and anti-arrhythmic strategies, remains paramount in management of shockable OHCA.
Gaspari R, Adhikari S, Gleeson T, et al. Occult Ventricular Fibrillation Visualized by Echocardiogram During Cardiac Arrest: A Retrospective Observational Study From the Real-Time Evaluation and Assessment for Sonography-Outcomes Network (REASON). J Am Coll Emerg Physicians Open. 2025;6(1):100028. doi: 10.1016/j.acepjo.2024.100028.
Category: Toxicology
Keywords: cannabinoids, liver enzymes, toxicology (PubMed Search)
Posted: 1/20/2026 by Lena Carleton, MD
(Updated: 1/26/2026)
Click here to contact Lena Carleton, MD
Consumer use of cannabidiol (CBD) products for medicinal and recreational purposes has increased in recent years. Regulatory barriers have limited randomized controlled trials examining the clinical and physiologic effects of cannabinoids in humans. This study aimed to evaluate the impact of daily cannabidiol oil use on liver enzymes and endocrine hormones in healthy adults.
In this double-blind, randomized, placebo-controlled study conducted at a clinical pharmacology unit in Wisconsin, 201 healthy adults were randomized to receive either oral CBD (2.5 mg/kg twice daily) or placebo. Laboratory testing was performed weekly.
Among participants receiving CBD (n = 151), 8 developed AST and ALT elevations greater than three times the upper limit of normal; 7 of these also had eosinophilia. No participants in the placebo group (n = 50) developed similar transaminase elevations. There were no significant differences between groups in measured endocrine hormones, including total testosterone, inhibin B, thyroid-stimulating hormone, total triiodothyronine, and free thyroxine.
Limitations included a modest sample size, unequal group sizes, and a relatively short duration of exposure and follow-up.
Key Takeaway: CBD use may be associated with elevations in AST and ALT. However, evidence remains limited, and abnormal liver enzymes should still prompt evaluation for alternative etiologies.
Florian J, Salcedo P, Burkhart K, et al. Cannabidiol and Liver Enzyme Level Elevations in Healthy Adults: A Randomized Clinical Trial. JAMA Intern Med. 2025;185(9):1070–1078. doi:10.1001/jamainternmed.2025.2366
Category: Trauma
Keywords: Pelvic fracture, EMS (PubMed Search)
Posted: 1/25/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
A reminder from a recent position paper on pelvic trauma that we should not be doing stability testing to evaluate pelvic trauma
“EMS clinicians should recognize the challenges in accurately identifying pelvic fractures by physical exam alone. Manual stability testing of the pelvis is neither sensitive nor specific and may cause harm.”
Lyng, J. W., Corsa, J. G., Raetzke, B. D., Wilson, B. R., McCoy, A., Patterson, S. C., … Bosson, N. (2025). Prehospital Trauma Compendium: Evaluation and Management of Suspected Pelvis Fractures – An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 1–35. https://doi.org/10.1080/10903127.2025.2540420
Category: Orthopedics
Posted: 1/24/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The recommended approach for patients with suspected septic arthritis is arthrocentesis with fluid analysis sent for: Gram stain, culture, WBC count with differential, and crystal analysis before starting antibiotics.
From a classic meta-analysis of 14 studies involving greater than 6,000 patients the only 3 findings that occur in more than 50% of patients with septic arthritis were
Joint pain (sensitivity, 85%; 95% confidence interval [CI], 78%-90%),
Joint swelling (sensitivity, 78%; 95% CI, 71%-85%),
Fever (sensitivity, 57%; 95% CI, 52%-62%).
Vs.
Sweats (sensitivity, 27%; 95% CI, 20%-34%)
and rigors (sensitivity, 19%; 95% CI, 15%-24%) were less common findings in septic arthritis.
The probability of septic arthritis increases progressively with higher synovial WBC counts:
PMN percentage ?90% suggests septic arthritis with LR 3.4 (95% CI, 2.8-4.2)
VS
PMN <90% lowers the likelihood (LR 0.34, 95% CI 0.25-0.47).
Margaretten ME, Kohlwes J, Moore D, Bent S. Does This Adult Patient Have Septic Arthritis? JAMA. 2007;297(13):1478-88.
Category: Ultrasound
Keywords: knee effusion, ultrasound, method (PubMed Search)
Posted: 1/21/2026 by Kerith Joseph, MD
(Updated: 1/22/2026)
Click here to contact Kerith Joseph, MD
Study Overview
Title: Identification of Knee Effusions With Ultrasound: A Comparison of Three Methods
Design: Prospective cohort study
Setting: Outpatient orthopaedic clinic
Participants: 52 adults (104 knees), including 57 painful knees
Objective
Determine whether two simple dynamic techniques improve ultrasound detection of suprapatellar knee effusions compared with static scanning.
Ultrasound Methods Compared
Static scanning: Patient relaxed; standard long- and short-axis views.
Parapatellar pressure (Method 1): Examiner compresses medial and lateral parapatellar recesses during scanning.
Quadriceps contraction (Method 2): Patient actively contracts quadriceps during scanning.
Outcome Measure
Presence of fluid in the suprapatellar recess (graded using a standardized ultrasound effusion scale).
Key Results
Effusions detected:
Static scanning: 45
Parapatellar pressure: 58
Quadriceps contraction: 77
Comparative performance:
Quadriceps contraction was superior to parapatellar pressure for detecting:
All effusions (PR 1.33; P < 0.001)
Painful knees (PR 1.24; P = 0.036)
Painless knees (PR 1.50; P = 0.006)
Both dynamic methods outperformed static scanning.
Additional detection beyond static scanning:
Parapatellar pressure: +16.9% of knees
Quadriceps contraction: +54.2% of knees
Reliability (Inter-rater Agreement)
Static scanning: ? = 0.771
Parapatellar pressure: ? = 0.686
Quadriceps contraction: ? = 0.846
All methods showed high reliability, with quadriceps contraction highest.
Conclusions
Both parapatellar pressure and patient-initiated quadriceps contraction significantly improve ultrasound detection of suprapatellar knee effusions.
Quadriceps contraction is the most effective method, especially for small or occult (grade 1) effusions.
Category: EMS
Keywords: VT, VF, shockable, pad placement (PubMed Search)
Posted: 1/21/2026 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
The European resuscitation council recommends AL (anterior-lateral) pad positioning while the American Heart Association recommends AL or AP (anterior-posterior) pad placement for defibrillation.
This was a prospective cohort study over a 4 year period in a single EMS jurisdiction. Adult patients with a medical cardiac arrest with an initial rhythm of VT/VF were included. The primary outcome was ROSC at any period of time.
Patients with AP pad placement (compared to AL) had a higher adjusted odds ratio of ROSC at any time (1.34), but not statistically different odds of pulse in the ED, survival to hospital admission or discharge, or functional status at hospital discharge.
The AP pad placement group also required less shocks on average and had earlier and initial sustained rates of ROSC. Further research is needed with respect to initial pad placement in the cardiac arrest population.
Lupton JR, Newgard CD, Dennis D, Nuttall J, Sahni R, Jui J, Neth MR, Daya MR. Initial Defibrillator Pad Position and Outcomes for Shockable Out-of-Hospital Cardiac Arrest. JAMA Netw Open. 2024 Sep 3;7(9):e2431673. doi: 10.1001/jamanetworkopen.2024.31673. Erratum in: JAMA Netw Open. 2024 Nov 4;7(11):e2448135. doi: 10.1001/jamanetworkopen.2024.48135. PMID: 39250154; PMCID: PMC11385052.
Category: Critical Care
Keywords: sepsis, subtypes, long term mortality, disability (PubMed Search)
Posted: 1/20/2026 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Settings: Secondary analysis of the Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis (CLOVERS) trial.
Participants:
1368 patients who survived on day 28 after enrollment, and were retrospectively assigned different subtypes:
Low risk, barriers to care. Younger patients with few comorbidities, less severe disease,
Unhealthy baseline with severe illness: Previously healthy with severe illness and complex needs after discharge, barriers to care.
Multimorbidity. Older patients with more comorbidities and are frequently readmitted.
Low functional status: Poor functional status. Older patients with high prevalence of frailty at discharge and high functional needs who are often discharged to a facility.
Unhealthy baseline with severe illness: Existing poor health with severe illness and complex needs after discharge. Older patients with severe comorbidities, more severe illness, high functional needs, prolonged hospital stay,
Outcome measurement:
A) 90-day mortality,
B) 6-month and 12-month EuroQol 5D five level score
Study Results:
A) 90-day mortality:
Unhealthy baseline with severe illness (37.6%) > low functional status (45.5%) > multimorbidity (17.4%) > unhealthy baseline, severe illness (13.2%) > Low risk (5.1%).
B) 6-month EuroQol 5D-Five Level: lower score, lower functional outcomes)
Unhealthy baseline with severe illness (0.53) > unhealthy baseline, severe illness (0.68) > low functional status (0.69) > multimorbidity (0.78) > Low risk (0.80).
Discussion:
a) The framework, readily available to clinicians provides good prognostic tools for mortality.
b) Although there was prediction of poor functional outcomes at 6-month and 12-month, the differences between subtypes in their EuroQoL 5D-5L did not seem to correspond to 90-day mortality. Low functional status group had 2nd-highest rate of mortality, but only 3rd in their EuroQoL 5D-3L score. Thus, there needs to be more studies in these nuances.
Conclusion:
Sepsis survivor subtypes—assigned using only three routinely available discharge variables—are strongly associated with 3-month mortality and long-term disability and HRQOL up to 12 months
Flick RJ, Kamphuis LA, Valley TS, Armstrong-Hough M, Iwashyna TJ. Association of Sepsis Survivor Subtypes With Long-Term Mortality and Disability After Discharge: A Retrospective Cohort Study. Crit Care Med. 2026 Jan 1;54(1):45-54. doi: 10.1097/CCM.0000000000006933. Epub 2025 Nov 13. PMID: 41231072.
Category: Ultrasound
Keywords: POCUS, GI, Hernia (PubMed Search)
Posted: 1/19/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/1/2026)
Click here to contact Alexis Salerno Rubeling, MD
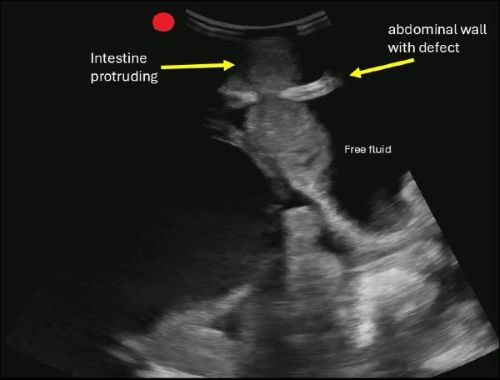
POCUS can help you identify signs of a hernia.
Begin by asking the patient to localize the point of maximal tenderness, then place a linear or curvilinear transducer over the area of concern. If there is concern for an inguinal hernia, you can have the patient perform a Valsalva maneuver while holding the probe in the area to evaluate dynamic changes.
A hernia is diagnosed when omental fat or intestinal contents are seen protruding through a defect in the abdominal wall.
If you are concerned about an incarcerated hernia, sonographic findings may include absence of peristalsis, presence of surrounding free fluid, with preserved blood flow on color Doppler. If a hernia progresses to strangulation, you may notice the absence of flow on color and power Doppler.
Boccatonda A, Brighenti A, Tiraferri V, Doglioli M, Iazzetta L, De Meis L, Safai Zadeh E, Dietrich CF, Serra C. POCUS for acute abdominal pain: practical scan protocols on gastrointestinal diseases and an evidence review. J Ultrasound. 2025 Dec;28(4):851-871. doi: 10.1007/s40477-025-01088-7.
Category: Geriatrics
Keywords: Delerium, antihistamine, geriatrics (PubMed Search)
Posted: 1/18/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In 261 ED patients over age 65 receiving first generation antihistamines, 15% had an adverse reaction. Most common was delirium and urinary retention. Age over 85, previous cognitive impairment and multiple doses increased the risk of adverse reaction. Along with previous literature, this should discourage use of first generation antihistamines in older ED patients.
Killen, E., Cusumano, M., Zhang, Z., Newman, R., Voigtmann, J., Sanford, A. M, & Bitter, C. C. (2025). First-Generation Antihistamine Use in Geriatric Emergency Department Patients: Retrospective Review. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 27(1). http://dx.doi.org/10.5811/westjem.47491 Retrieved from https://escholarship.org/uc/item/7230n5z1
Category: Pediatrics
Keywords: PNA, CXR (PubMed Search)
Posted: 1/16/2026 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
This was a retrospective study at a tertiary pediatric emergency department over a 10 year period. Authors sought to determine the number of patients who developed radiographic pneumonia after an initial normal CXR.
9957 patients with suspected pneumonia were included. 240 had an additional CXR within 14 days and 27 (11% of those with a 2nd CXR) had developed PNA on the CXR. Overall, the rate was 1/370 children went on to have radiographic PNA in the next 14 days after an initial CXR. Tachypnea, hypoxia and dehydration at the initial visit were shown to be associated with later development of PNA on CXR.
Hirsch AW, Wagner A, Lipsett SC, Monuteaux MC, Neuman MI. Risk of Subsequent Pneumonia After a Negative Chest Radiograph in the ED. Pediatrics. 2025 May 1;155(5):e2024069829. doi: 10.1542/peds.2024-069829. PMID: 40189217.
Category: Toxicology
Keywords: Opiate use disorder, MOUD, initiation (PubMed Search)
Posted: 1/15/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
In this study reviewing data from the American College of Emergency Physicians’ Emergency Quality Network substance use disorder program, EDs prescribed naloxone in 27% of patients discharged after opioid overdose. Only 7% received ED administered or prescription for buprenorphine, etc. There is a lot of room for improvement in the care we provide for this subset of ED patients.
Weiner, Scott G. et al.
Annals of Emergency Medicine, Volume 0, Issue 0
Category: Critical Care
Posted: 1/13/2026 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Recall that MAP = (cardiac output) x (systemic vascular resistance)
Consequently, a patient can be normotensive due to increased SVR despite a very low cardiac output and shock. In fact, normotensive shock may have worse outcomes compared to patients with isolated hypotension.
Take home points:
Yerasi C, Case BC, Pahuja M, et al. "The Need for Additional Phenotyping When Defining Cardiogenic Shock." JACC Cardiovasc Interv. 2022;15(8):890-895.
Category: Obstetrics & Gynecology
Posted: 1/12/2026 by Jennifer Wang, MD
Click here to contact Jennifer Wang, MD
At this point, I think we've all heard about vacuum-induced uterine tamponade (where negative pressure is used to draw down the uterine walls and stop postpartum hemorrhage), which is achieved in our OBGYN colleagues world with the Jada device, something that costs between 600-1200 USD and that most emergency medicine doctors are not trained on. However, our colleagues in Columbia and South Africa have come up with an alternative: the simple gastric tube.

59 patients were enrolled in this randomized feasibility trial with the goal to look for a 50% reduction in the primary outcome (blood loss >1000ml) comparing a 24 Fr Levin gastric tube and standard balloon uterine tamponade. Patients were given a survey asking about their experiences with the two devices.
Researchers analyzed this both with intention-to-treat and with per-protocol analysis looking at their primary outcome, and while their intention-to-treat analysis fell sort of significance (p value = 0.07), their per protocol just snuck to significance (p value = 0.04). They had one patient who had to switch over from the suction tube/gastric tube over to a balloon tamponade method, which was responsible for the change in their intention-to-treat analysis falling short. Still, the fact that a gastric tube reduced postpartum hemorrhage >1000ml around 40% compared to standard balloon uterine tamponade is both impressive and intriguing to me. Additionally, patients reported that the suction tube was much less painful than the balloon tamponade.
Some caveats: a very small number of patients, lack of dedicated research staff/missing data, only in Columbia and South Africa
So if you're ever in a desperate situation with a hemorrhage postpartum patient without the appropriate resources, a gastric tube could be your best friend!
Singata-Madliki M, Nieto-Calvache AJ, Rivera Torres LF, et al. Suction tube uterine tamponade versus uterine balloon tamponade for treatment of refractory postpartum hemorrhage: A randomized clinical feasibility trial. Int J Gynaecol Obstet. 2025;170(1):326-337. doi:10.1002/ijgo.16164
Category: Trauma
Keywords: Prehospital, transfusion, non-trauma (PubMed Search)
Posted: 1/11/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
Much has been written about the benefits of prehospital blood transfusion for traumatic hemorrhage. Can this success be ascribed to non-traumatic hemorrhage as well? This small study (50 patients over 10 years!) says there were improvements in patient physiology (shock index) for those patients receiving blood for GI bleed, etc. Much more research is needed however this could be a beneficial practice in the future.
Kodakadath, H., Dillane, S., Griggs, J. et al. Pre-hospital blood transfusion in non-traumatic major haemorrhage: a retrospective observational study. Scand J Trauma Resusc Emerg Med 33, 191 (2025). https://doi.org/10.1186/s13049-025-01495-z
Category: Administration
Posted: 1/10/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Plain films are often the first imaging test ordered in patient’s with knee injuries.
Plain films do NOT directly show the ACL but may reveal indirect signs of an ACL tear.
Key Plain Film Findings:
1) Effusion
ACL injury generates a large joint effusion (swelling/hemarthrosis). The presence of a fat/fluid interface (lipohemarthrosis) suggests associated bone injury.
This may be seen as joint fluid on the plain film lateral view. This view is best obtained with the patient in the supine position. This allows a layering of fluid in the suprapatellar bursa. A fat/fluid level indicates the presence of a lipohemarthrosis, signifying the likelihood of an intraarticular fracture.
http://radiologykey.com/wp-content/uploads/2019/03/f10-02ad-9781437727791.jpg
( A ) The normal suprapatellar bursa is seen on the lateral view as a line extending obliquely anterior and superior from the superior/posterior surface of the patella to the posterior surface of the quadriceps tendon.
(B) A small to moderate-sized effusion.
(C) A larger effusion.
In (D) the quadriceps tendon is bulged outward by an even larger joint effusion.
In the correct clinical setting, the presence or absence of a new fusion can be highly suggestive of ACL tear. Effusion can usually accurately be assessed on both physical exam and the lateral plain film. The absence of a knee effusion makes acute tear of the ACL unlikely as clinical practice suggests a rapidly developing hemarthrosis. Effusion of the knee may be associated with other entities such as intraarticular fracture or underlying arthritis. Typically, patients with acute ACL tears are young and do not have chronic infusions. Most acute meniscal tears and chondral injuries do not develop acute large effusions due to lack of significant vascularity.
Category: Orthopedics
Posted: 1/10/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Plain films are often the first imaging test ordered in patient’s with knee injuries.
Plain films do NOT directly show the ACL but may reveal indirect signs of an ACL tear.
Key Plain Film Findings:
1) Effusion
ACL injury generates a large joint effusion (swelling/hemarthrosis). The presence of a fat/fluid interface (lipohemarthrosis) suggests associated bone injury.
This may be seen as joint fluid on the plain film lateral view. This view is best obtained with the patient in the supine position. This allows a layering of fluid in the suprapatellar bursa. A fat/fluid level indicates the presence of a lipohemarthrosis, signifying the likelihood of an intraarticular fracture.
http://radiologykey.com/wp-content/uploads/2019/03/f10-01ae-9781437727791.jpg
( A ) The normal suprapatellar bursa is seen on the lateral view as a line extending obliquely anterior and superior from the superior/posterior surface of the patella to the posterior surface of the quadriceps tendon.
(B) A small to moderate-sized effusion.
(C) A larger effusion.
In (D) the quadriceps tendon is bulged outward by an even larger joint effusion.
In the correct clinical setting, the presence or absence of a new fusion can be highly suggestive of ACL tear. Effusion can usually accurately be assessed on both physical exam and the lateral plain film. The absence of a knee effusion makes acute tear of the ACL unlikely as clinical practice suggests a rapidly developing hemarthrosis. Effusion of the knee may be associated with other entities such as intraarticular fracture or underlying arthritis. Typically, patients with acute ACL tears are young and do not have chronic infusions. Most acute meniscal tears and chondral injuries do not develop acute large effusions due to lack of significant vascularity.
Category: Pediatrics
Keywords: Pediatrics, BLS, resuscitation, CPR (PubMed Search)
Posted: 1/9/2026 by Kathleen Stephanos, MD
(Updated: 2/1/2026)
Click here to contact Kathleen Stephanos, MD
In 2025, the AHA and AAP teamed up for the latest Cardiac arrest guides- worth a read overall, Peds had a couple tweaks which should be recognized.
2-finger CPR is OUT. It has been shown to be ineffective, so the Two Thumb–Encircling Hands Technique should be used on ALL infants.
Grab your AED early. While a staple of adult BLS, this is now being emphasized in pediatrics as well.
For foreign body aspiration, remember to start with 5 back blows, but if the child is <1year old follow with chest thrusts, those who are older may receive abdominal thrusts. Repeat as needed. This has been in the literature for a while but was re-enforced due to potential injury to infants who receive abdominal thrusts.
Lasa JJ, Dhillon GS, Duff JP, Hayes J, Kamath-Rayne BD, Levy A, Mahgoub M, Morgan RW, McCormick T, Roberts JS, Ross CE, Schexnayder SM, Sweberg T, Valdés SO, Topjian AA. Part 8: Pediatric Advanced Life Support: 2025 American Heart Association and American Academy of Pediatrics Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2025 Oct 21;152(16_suppl_2):S479-S537. doi: 10.1161/CIR.0000000000001368. Epub 2025 Oct 22. PMID: 41122885.
