Category: Pediatrics
Keywords: croup, laryngomalacia (PubMed Search)
Posted: 10/26/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: voriconazole (PubMed Search)
Posted: 10/25/2012 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
As everyone knows by now the New England Compounding Company has been implicated in contaminated steroid vials that were used for epidural injections. Patients that have pleocytosis on CSF after lumber puncture will be admitted and started on liposomal amphotericin B and IV voriconozaole.
IV Voriconazole Adverse Effects:
Vivid visual hallucinations
Visual Disturbances - 30 min after administration: Blurry, photosensitivity
Hepatotoxitcity
Photoxicity - associated with increased risk of squamous cell CA of the skin
Category: International EM
Keywords: international, fever, Borrelia, tick, louse (PubMed Search)
Posted: 10/24/2012 by Andrea Tenner, MD
(Updated: 2/2/2026)
Click here to contact Andrea Tenner, MD
University of Maryland Section for Global Emergency Health
Author: Gentry Wilkerson
Category: Critical Care
Posted: 10/22/2012 by Haney Mallemat, MD
(Updated: 10/24/2012)
Click here to contact Haney Mallemat, MD
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
Category: Visual Diagnosis
Posted: 10/22/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Trauma patient (...yes, that's the only history you're given). Diagnosis?
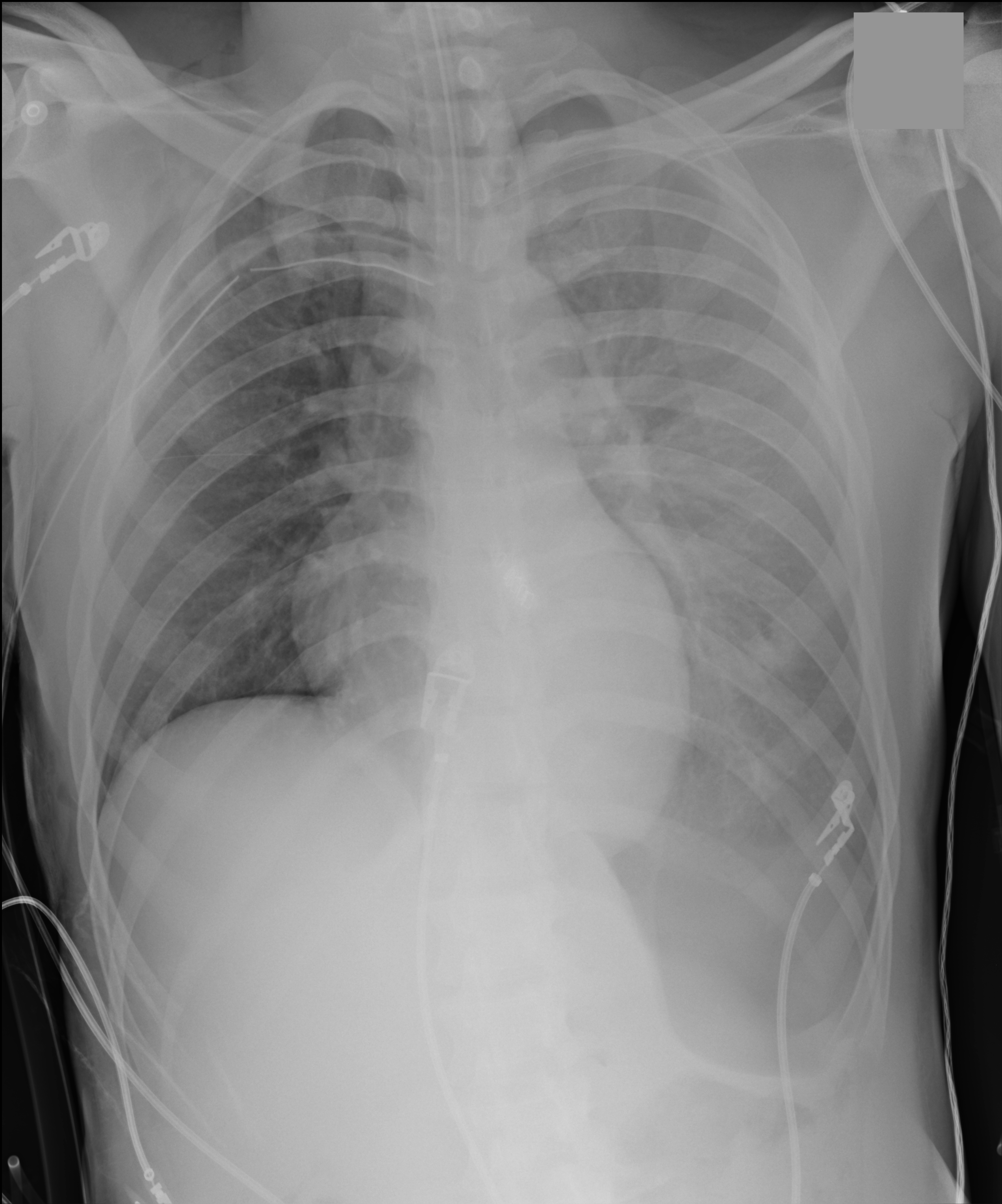
Answer: Inverted left hemidiaphragm (or deep sulcus sign) secondary to a tension pneumothorax. There is also a superimposed hemothorax.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Posted: 10/20/2012 by Semhar Tewelde, MD
(Updated: 10/21/2012)
Click here to contact Semhar Tewelde, MD
Cardiac amyloidosis can present along a spectrum from asymptomatic to severe CHF w/conduction abnormalities
ECG with low voltage + echocardiogram with thickened myocardium should heighten suspicion
Definitive Dx. is myocardial biopsy identifying the infiltrative lesion (MRI w/gad is also supportive)
AL (light chain) amyloidosis is an acquired disease from improperly functioning plasma cells
¨ Rapidly progressive and life threatening
¨ Tx. w/chemotherapeutic agents (+/- BMT)
Transthyretin-related (TTR) amyloidosis is produced by the liver (2 types)
Familial transthyretin-related amyloidosis (ATTR)
Senile systemic amyloidosis (SSA)
¨ Both are slowly progressive
¨ Tx liver transplant (ATTR) and supportive care (SSA)
Quarta C, Kruger J, Falk R. Cardiac Amyloidosis. Circulation. Sept 2012;126(2)178-182
Category: Toxicology
Keywords: methadone (PubMed Search)
Posted: 10/18/2012 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
Many who work in urban EDs and have a patient population that has a high rate of methadone use have probably wondered - why don't I see many STEMIs in the ED?
One study has actually attempted to answer the question - is methadone cardioprotective? Comparing 98 decedents with known long-term methadone exposure and compared autopsy coronary artery findings to match controls without, there was significant decrease in incidence of severe CAD:
5/98 Methadone Patients post-mortem had severe CAD vs 16/97 match controls
Better than a baby ASA, who knew?
[I thank Dr. Hoffman for citing this article to me]
Coronary artery disease and opioid use.
Marmor M, Penn A, Widmer K, Levin RI, Maslansky R.
Am J Cardiol. 2004 May 15;93(10):1295-7.
Category: Critical Care
Posted: 10/16/2012 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Delirium in the Critically Ill
Bienvenu OJ, Neufeld KJ, Needham DM. Treatment of four psychiatric emergencies in the intensive care unit. Crit Care Med 2012; 40:2662-2670.
Category: Visual Diagnosis
Posted: 10/15/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
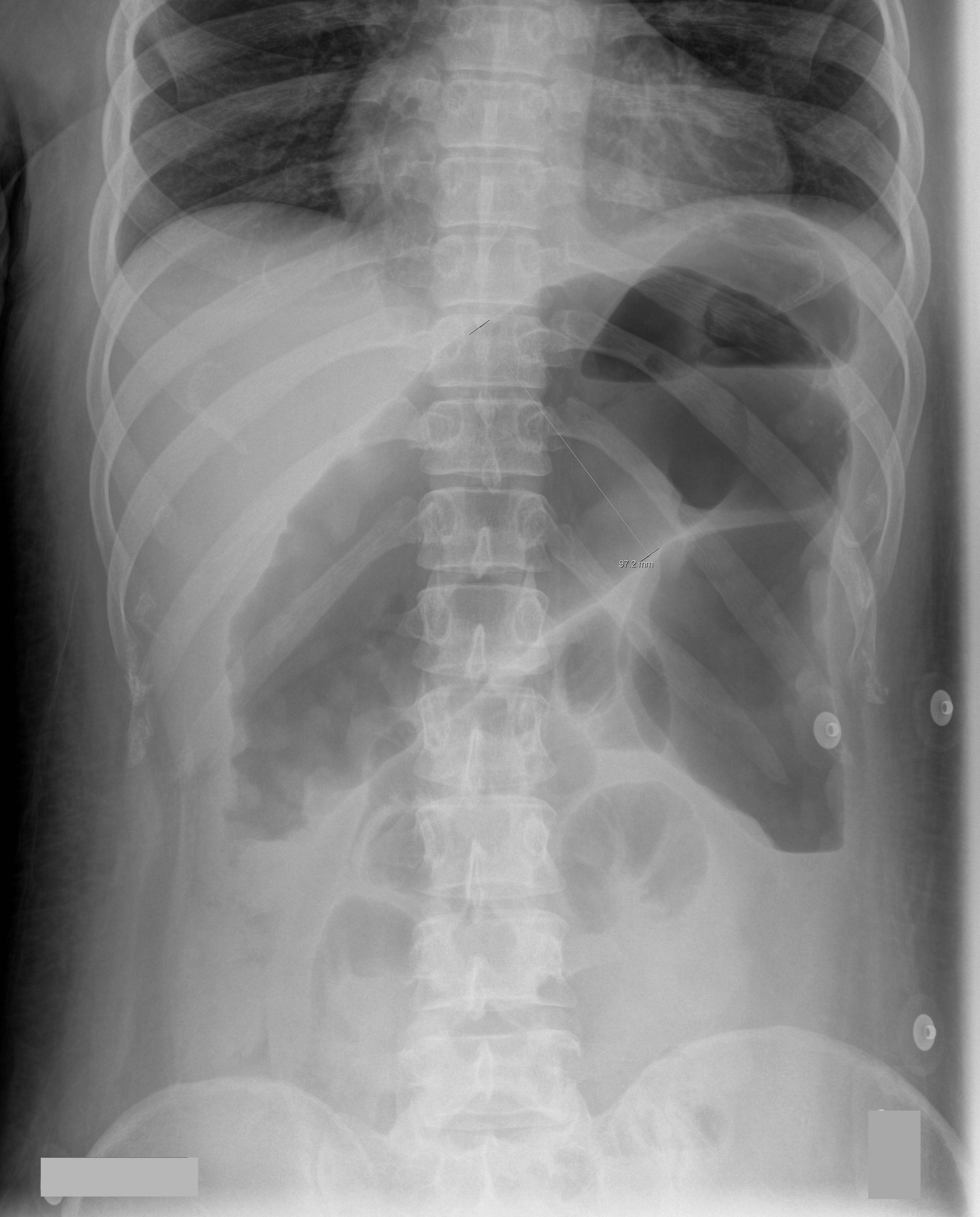
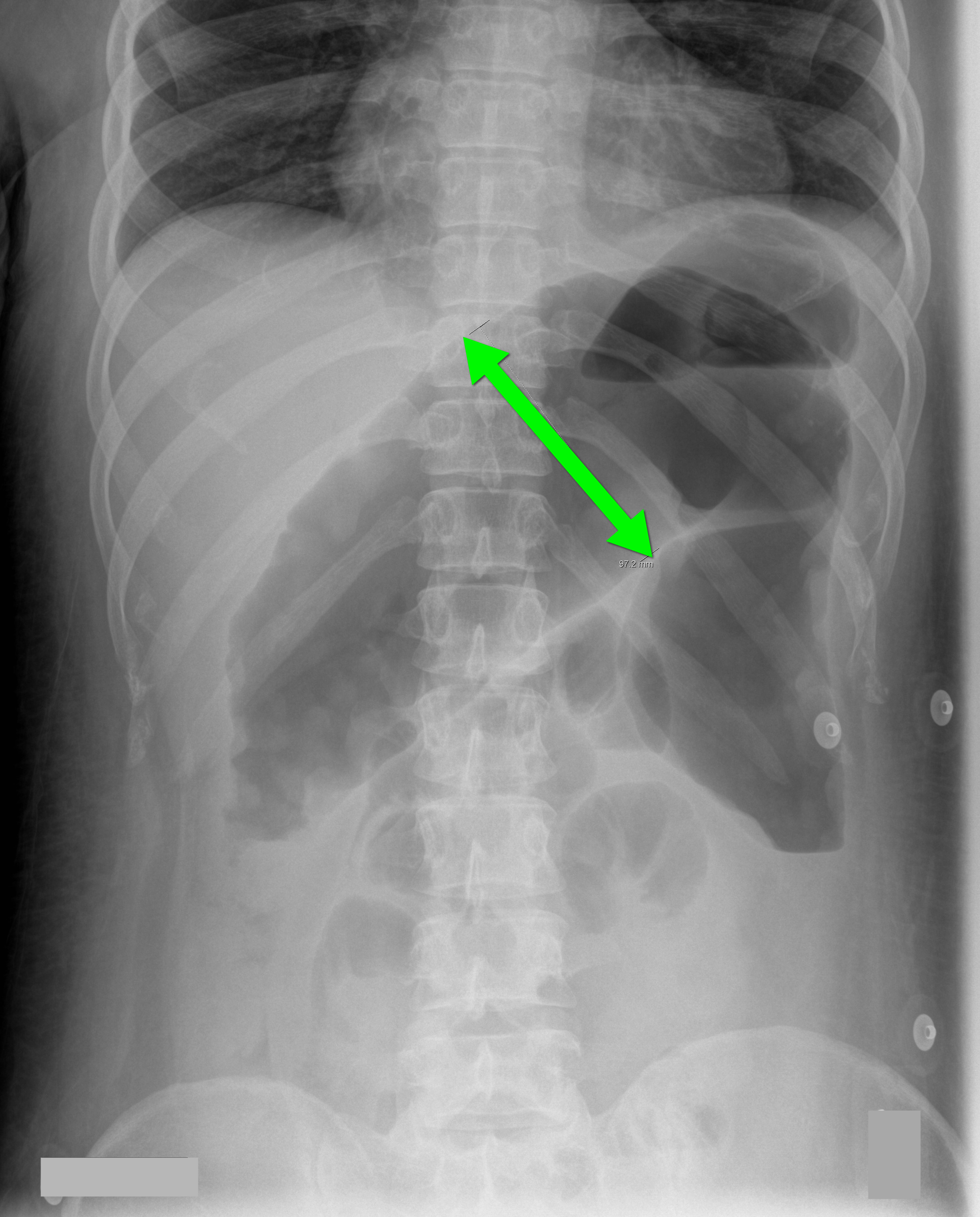
35 year-old male unrestrained driver following motor vehicle crash presents with blunt chest injury. There are multiple injuries on CXR (can you find them all?), but what's up with his right lung?
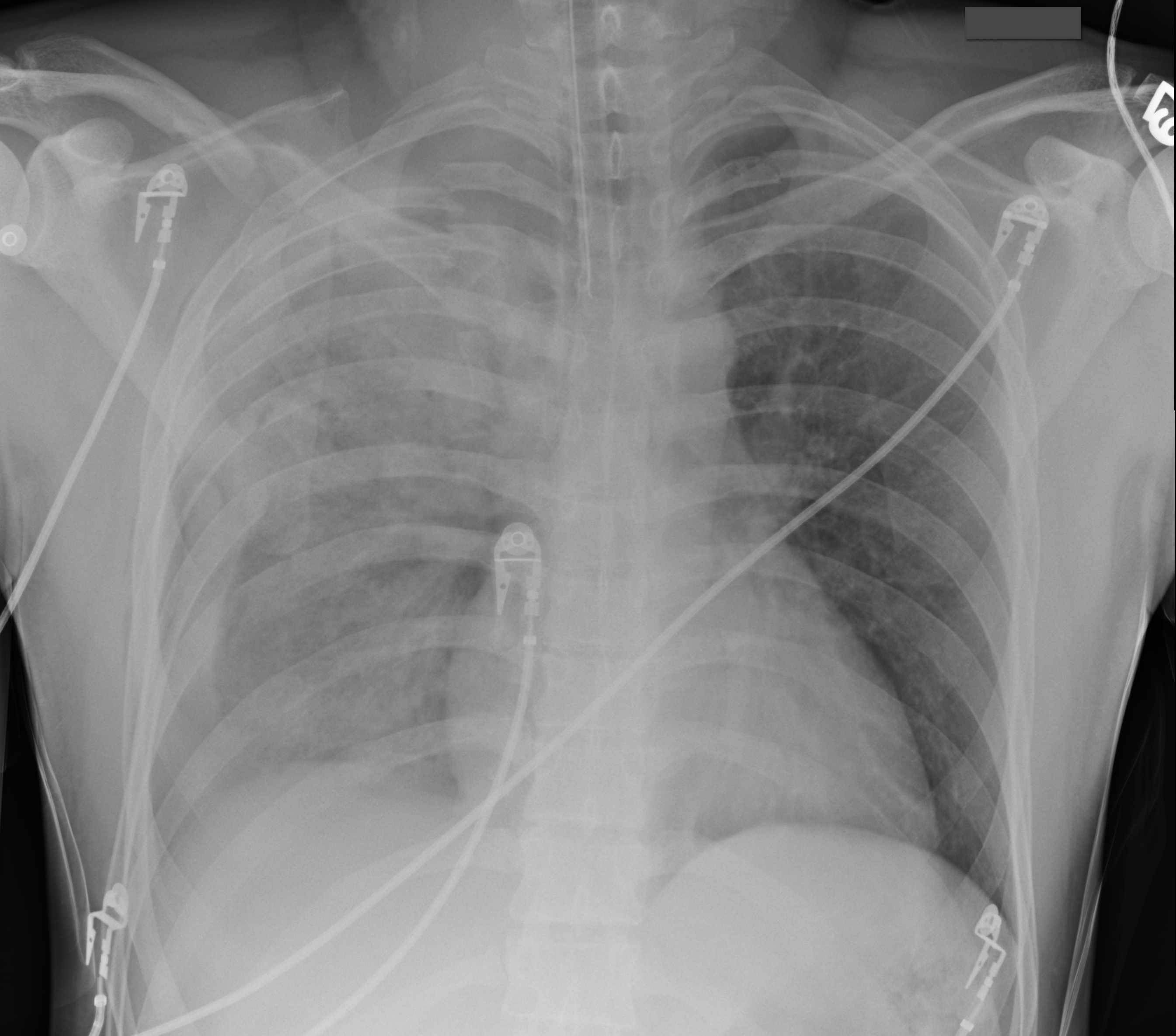
Answer: Pulmonary contusion
Blunt chest trauma may result in pulmonary contusion, a parenchymal lung injury resulting in blood and edema within the alveolar spaces.
The pathophysiologic effects result in reduced lung compliance and gas exchange (i.e., dead space ventilation and/or shunting), increased risk of ARDS, and increased pulmonary vascular resistance. The full pathophysiologic effects may take up to 48 hours to develop. Resolution usually occurs within 3-5 days.
Diagnosis is typically made on CXR, although early CXR may underestimate the severity of injury. CT scan is much more sensitive for diagnosis (see green arrows below).
Management is supportive and requires strict attention to oxygenation. Positive pressure ventilation is occasionally required for respiratory failure and is sometimes recommended prophylactically for elderly patients, because their pulmonary status can rapidly decline secondary to their reduced lung reserve.
Aggressive control of chest wall pain is also required. Pain reduces both the frequency and depth of respirations leading to atelectasis, a reduction in mucus clearance, and an increased risk of pneumonia. Analgesia should be administered systemically, by epidural, or by local nerve block at the level of injury.

Lively, M. Pulmonary contusion in a collegiate diver: a case report. J Med Case Rep. 2011 Aug 10;5:362.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Chagas Disease, AV Block (PubMed Search)
Posted: 10/13/2012 by Semhar Tewelde, MD
(Updated: 10/14/2012)
Click here to contact Semhar Tewelde, MD
Etiological agent is the parasite Trypanosoma cruzi
Elizari M, Chiale P. Cardiac arrhythmias in Chagas' heart disease. Journal of cardiovascular electrophysiology.1993 vol:4 iss:5 pg:596 -608
Category: Orthopedics
Keywords: Marathon, cardiac arrest, cardiac death (PubMed Search)
Posted: 10/13/2012 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Congratulations to today's Baltimore marathoners and the medical race staff
In honor of them:
Marathons are becoming increasingly popular with participation rising from an estimated 143,000 US marathon finishers in 1980 to a record high of 507,000 during 2010.
Most victims of exercise-related sudden cardiac arrest have NO premonitory symptoms
Autopsy reports show that
1) 65 - 70% of all adult sudden cardiac deaths are attributable to coronary artery disease.
2) 10% due to other structural heart diseases (HOCM, congenital artery abnormalities)
3) 5 - 10% due to primary cardiac conduction disorders (prolonged QT, ion channel disorders)
4) Remainder are due to non cardiac etiologies
Overall risk of sudden cardiac arrest is approximately from 1 in 57,000 and the risk of sudden cardiac death is approximately 1 in 171,000. Mortality without intervention after sudden cardiac arrest is greater than 95%. The majority occur in middle to late aged males.
V fib/V tach are the most common arrhythmias leading to sudden cardiac arrest. Most events occur in the last 4 miles of the racecourse.
Survival decreases by 7 - 10% with each minute of delayed defibrillation. Defibrillation within 3 minutes can produce survival rates as high as 67 - 74%. After 8 minutes, there is a dramatic decrease in survival. Prompt CPR increases survival from 2.5% to greater than 8%.
Sudden cardiac arrest and death in united states marathons. Webner D, Duprey KM, Drezner JA, Cronholm P, Roberts WO. Med Sci Sports Exerc. 2012 Oct;44(10):1843-5.
Category: Pediatrics
Posted: 10/12/2012 by Rose Chasm, MD
(Updated: 2/2/2026)
Click here to contact Rose Chasm, MD
Glaser N, Barnett P, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med 2001;344:264.
Category: Toxicology
Keywords: charcoal, prehospital, EMS, gastrointestinal decontamination (PubMed Search)
Posted: 10/9/2012 by Bryan Hayes, PharmD
(Updated: 10/11/2012)
Click here to contact Bryan Hayes, PharmD
Activated charcoal is most effective if given within 1 hour of overdose.
Prehospital administration of charcoal can be challenging, but may save significant time compared to waiting until arrival to the ED. The patient has to be transported by EMS, registered, seen by a provider, order for charocal placed...
Two studies evaluated the time difference between prehospital and hospital administration of GI decontamination.
Bottom line: Don't underestimate the amount of time that goes by before you evaluate non-crashing patients upon arrival to the ED. If the story supports an overdose and the patient doesn't have contraindications for receiving charcoal, recommend it be given in the prehospital setting for greatest potential benefit.
Wax PM, Cobaugh DJ. Prehospital gastrointestinal deconatmination of toxic ingestions: a missed opportunity. Am J Emerg Med 1998;16:114-6.
Crockett R, et al. Prehospital use of activated charcoal: a pilot study. J Emerg Med 1996;14(3):335-8.
Follow me on Twitter (@PharmERToxGuy)
Category: Critical Care
Posted: 10/9/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
70 year-old male recently treated for community-acquired pneumonia presents with bloody diarrhea, fever, and severe abdominal pain. Abdominal Xray is shown below. Diagnosis?
Answer: Toxic Megacolon
Toxic megacolon (TM) is an acute colitis with segmental or total colonic dilation (>6cm) plus systemic toxicity.
Actual incidence is unknown, but it is believed that TM is rising because of increasing cases of Clostridium difficile and the aging population.
The most common etiologies are ulcerative, chron, and pseudomembranous colitis, but other causes exist and can be categorized as:
The diagnosis is made based on clinical evidence of colitis plus evidence of colonic dilation on abdominal XR (diameter > 6cm, loss of haustra, or free intraperitoneal air secondary to perforation) or CT scan (demonstrating dilation or perforation).
Treatment includes:
Autenrieth, D et al. Toxic Megacolon Inflammatory Bowel Dis. 2011 Aug 29.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/7/2012 by Haney Mallemat, MD
(Updated: 10/8/2012)
Click here to contact Haney Mallemat, MD
26 year-old male from Indonesia presents with severe abdominal pain and weight loss for the past two months. He also states he found this "worm" in the toilet (see below) after a bowel movement. What is the medical treatment for this condition?
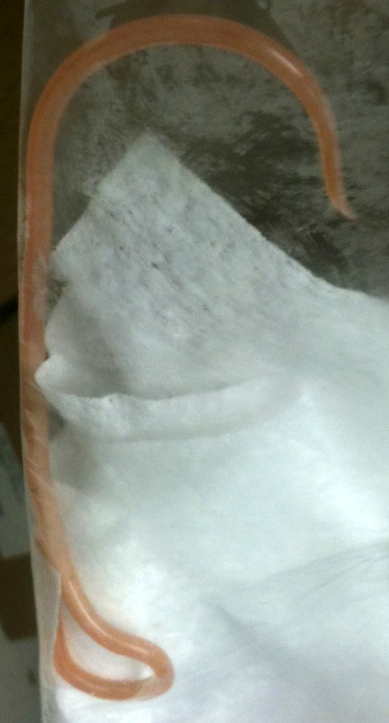
Answer: Mebendazole or albendazole
The image above shows an Ascaris Lumbricoides (AL), the most common intestinal roundworm infection in humans. It typically occurs in inhabitants of impoverished areas with poor sanitation.
Humans acquire AL from ingesting eggs from infected food or soil. Eggs hatch into larvae within the small intestine and then migrate through the mucosa to vascular beds of the alveoli within the lung. Larvae then migrate up the respiratory tree and are swallowed into the GI tract where they mate and more eggs are laid, maturing here or migrating to other organs within the body.
Most infections are asymptomatic, but signs and symptoms can range from nonspecific pulmonary (first two weeks secondary to larval migration into lungs) to severe (after six weeks secondary to the mechanical effects of high parasite load in the gut). Symptoms include:
Treatment during early infection is challenging because AL is non-specific and difficult to diagnose; symptomatic and supportive care is required. When the diagnosis is made, medications such as mebendazole and albendazole can be used to eradicate AL directly within the gut. Situations where worms cause intestinal obstruction, require manual debulking using scopes (e.g., colonoscopy) or surgery.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Autoantibody-associated Congenital Heart Block, neonatal lupus, CHB (PubMed Search)
Posted: 10/7/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Autoantibody-associated congenital heart block (CHB), also know as neonatal lupus, is responsible for the majority (~60-90%) of CHB
This is secondary to maternal antibodies that cross the placenta and may disappear postnatal
Neonatal lupus can result in diffuse myocardial disease both with and without conduction disturbances, structural defects, and electrophysiologic anomalies
Overall mortality is up to 30%, with 15% mortality before 3 months of age
More than 65% of surviving newborns require pacemakers
Maternal screening and fetal echocardiography has allowed routine prenatal diagnosis
Capone C, Buyon J, Friedman D, Frishman W. Cardiac Manifestations of Neonatal Lupus: A Review of Autoantibody-associated Congenital Heart Block and its Impact in an Adult Population. Cardiology Review. 2012, Mar-Apr;20(2):72-76
Category: Pharmacology & Therapeutics
Keywords: sulfa, allergy, cross-reactivity, antimicrobial, sulfonamide (PubMed Search)
Posted: 9/24/2012 by Bryan Hayes, PharmD
(Updated: 10/6/2012)
Click here to contact Bryan Hayes, PharmD
Patients frequently report having a sulfa allergy. In most cases, the allergic reaction was secondary to a sulfonamide antimicrobial agent, such as sulfamethoxazole-trimethoprim.
The question is: Can I use furosemide (or other non-antimicrobial agents containing a sulfa component)?
There is minimal evidence of cross-reactivity between sulfonamide antimicrobials and non-antimicrobials.
Despite this, the U.S. FDA-approved product information for many non-antimicrobial sulfonamide drugs contains warnings concerning possible cross-reactions.
Bottom line: If a patient had a true IgE-mediated anaphylatic reaction to a sulfonamide antimicrobial, it may be best to avoid other sulfa-related medications (use ethacrynic acid if a loop diuretic is needed). Otherwise, the available literature does not support cross-reactivity between sulfonamide antimicrobials and non-antimicrobials.
Strom BL, et al. Absence of cross-reactivity between sulfonamide antibiotics and sulfonamide nonantibiotics. N Engl J Med 2003;349(17):1628-35.
Hemstreet BA, et al. Sulfonamide allergies and outcomes related to use of potentially cross-reactive drugs in hospitalized patients. Pharmacother 2006;26(4):551-7.
Lee AG, et al. Presumed "sulfa allergy" in patients with intracranial hypertension treated with acetazolamide or furosemide: cross-reactivity, myth or reality? Am J Ophthalmol 2004;138(1):114-8.
Johnson KK, et al. Sulfonamide cross-reactivity: fact or fiction? Ann Pharmacother 2005;39(2):290-301.
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: Vaccines (PubMed Search)
Posted: 10/5/2012 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
We often ask our pediatric patients if there vaccines are up to date, but what does this mean?
Hepatitis B: birth, 2 and 6 months
Diphtheria/Tetanus and Acellular Pertussis: 2, 4 and 6 months
Pneumococcal vaccine: 2, 4 and 6 months
Haemophilus influenzae B : 2, 4 and 6 months
Polio: 2, 4 and 6 months
Rotavirus: 2 and 4 months or 2, 4 and 6 months depending on the brand.
Influenza: 6 months and older
Children less than 8 years old should receive 2 doses of flu vaccine at least 4 weeks apart during the first flu season that they are immunized. Children older than 2 years are eligible for the nasal vaccine if they do not have asthma, wheezing in the past 12 months or other medical conditions that predispose them to flu complications.
To see the full vaccine schedule including exact time frames between doses and catch up schedules, see: http://www.cdc.gov/vaccines/
Category: Toxicology
Keywords: propylene glycol, lorazepam, phenytoin (PubMed Search)
Posted: 10/4/2012 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
Ever have that alcholic who requires lorazapam doses that start to approach 10mg? 20mg? or even higher. The next step is usually a lorazepam infusion and then send them to the ICU. In the ICU, the patient develops an unexplained anion gap lactic acidosis.
Check a Lactate - lorazepam has 80% propylene glycol (PG). PG is metabolized to lactate which can accumulate when a lorazepam infusion at an elevated dose is running constantly. Hypotension, bradycardia and even other EKG changes have been reported. Simply discontinue the infusion and assess your acid-base status.
Other IV meds that contain PG:
lorazepam - 80% PG
Phenytoin - 40% PG
Phenobarbital - 67.8%
Diazepam - 40% PG
Category: Toxicology
Keywords: Cannabinoid,hyperemesis, marijauna (PubMed Search)
Posted: 10/4/2012 by Ellen Lemkin, MD, PharmD
(Updated: 2/2/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Michael Hiotis PharmD, CSPI. ToxTidbits. Maryland Poison Center Sep 2012
