Category: Cardiology
Posted: 2/10/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
-Common life-threatening cardiovascular effects of cocaine intoxication include tachydysrhythmias, ventricular fibrillation, myocardial ischemia, and infarction.
-Emergency management of acute cocaine intoxication relies mainly on supportive and symptomatic treatment, w/liberal use of gamma-aminobutyric acid receptor agonists such as benzodiazepines.
-Intravenous lipid emulsion (ILE) therapy has been used successfully to treat cardiac toxicity associated with a variety of lipid-soluble drugs, such as local anesthetics, calcium/beta-blockers, tricyclic anti-depressants, and cocaine.
-The current hypothesis, called the “lipid sink” hypothesis, suggest that ILE infusion creates an expanded lipid phase in the plasma that absorbs the circulating lipophilic toxin and decreases the amount of free unbound toxin available to bind to the myocardium.
-When life-threatening cardiac arrhythmias (e.g. wide-complex tachycardia/prolonged QT) are not amenable to standard therapy (e.g. sodium bicarbonate/magnesium) consider ILE as a potential option to the current algorithm.
Arora N, Berk W, et al. Usefulness of Intravenous Lipid Emulsion for Cardiac Toxicity from Cocaine Overdose. The American Journal of Cardiology. Volume 111, Issue 3. Feb 2013.
Category: Orthopedics
Keywords: head injury, concussion, return to play (PubMed Search)
Posted: 2/9/2013 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Estimated 3.8 million sport-related concussions per year (likely significantly higher due to underreporting)
Most patients recover within a 7-10 day period
** Children and teenagers require more time than college and professional athletes
This "accepted" time for recovery is not scientifically established and there is a large degree of variability based on multiple factors including age (as above), sex & history of prior concussions
Approximately 10% of athletes have persistent signs and symptoms beyond 2 weeks (which may represent a prolonged concussion or the development of post-concussion syndrome)
During this time the patient should have complete rest from all athletic activities, close follow-up with PCP and be educated re concussions.
If practical, "cognitive rest" should also be prescribed. This is one of the most frequently neglected aspects of post-concussion care and will be discussed in a future pearl.
Category: Toxicology
Keywords: anabolic, bodybuilding, weightlifting, beta agonist, myocardial infarction (PubMed Search)
Posted: 2/7/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Category: International EM
Keywords: Melioidosis, Burkholderia pseudomallei (PubMed Search)
Posted: 2/7/2013 by Andrea Tenner, MD
(Updated: 2/2/2026)
Click here to contact Andrea Tenner, MD
Just a quick clarification to last week's melioidosis pearl:
An astute reader noted the typo: "The patient should also be covered for melioidosis, and infection caused by Burkholderia pseudomallei." The sentence should read "...meliodosis, an infection caused by Burkholderia pseudomallei."
Just to clarify, melioidosis is caused by the bacteria Burkholderia pseudomallei.
Many apologies for any confusion this might have caused.
Thanks for reading!
Andi Tenner, MD, MPH
Category: International EM
Keywords: Rifapentine, latent tuberculosis, international, infectious disease (PubMed Search)
Posted: 2/6/2013 by Andrea Tenner, MD
(Updated: 2/2/2026)
Click here to contact Andrea Tenner, MD
Background Information:
Active tuberculosis (TB) develops in 5-10% of individuals who become infected with M. tuberculosis, typically after a latency period of 6-18 months (but sometimes decades later). Compliance with the 9 month self-supervised isoniazid (INH) regimen has been porr with completion rates <60%. Until recently, daily rifampin for 4-6 months has been the only alternative when the bacterium is resistant or INH cannot be used.
Pertinent Study Design and Conclusions:
Bottom LIne:
A substantially shorter course of therapy with INH-RPT is now the recommended treatment for latent TB.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
MMWR Morb Mortal Wkly Rep. 2011 Dec 9;60(48):1650-3.
Category: Critical Care
Posted: 2/5/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Needle Decompression - Are we Teaching the Right Location?
Inaba K, et al. Optimal positioning for emergent needle thoracostomy: A cadaver-based study. J Trauma 2011; 71:1099-1103.
Inaba K, et al. Radiologic evaluation of alternative sites for needle decompression of tension pneumothorax. Arch Surg 2012; 147:813-8.
Martin M, et al. Does needle decompression provide adequate and effective decompression of tension pneumothorax? J Trauma 2012; 73:1412-1417.
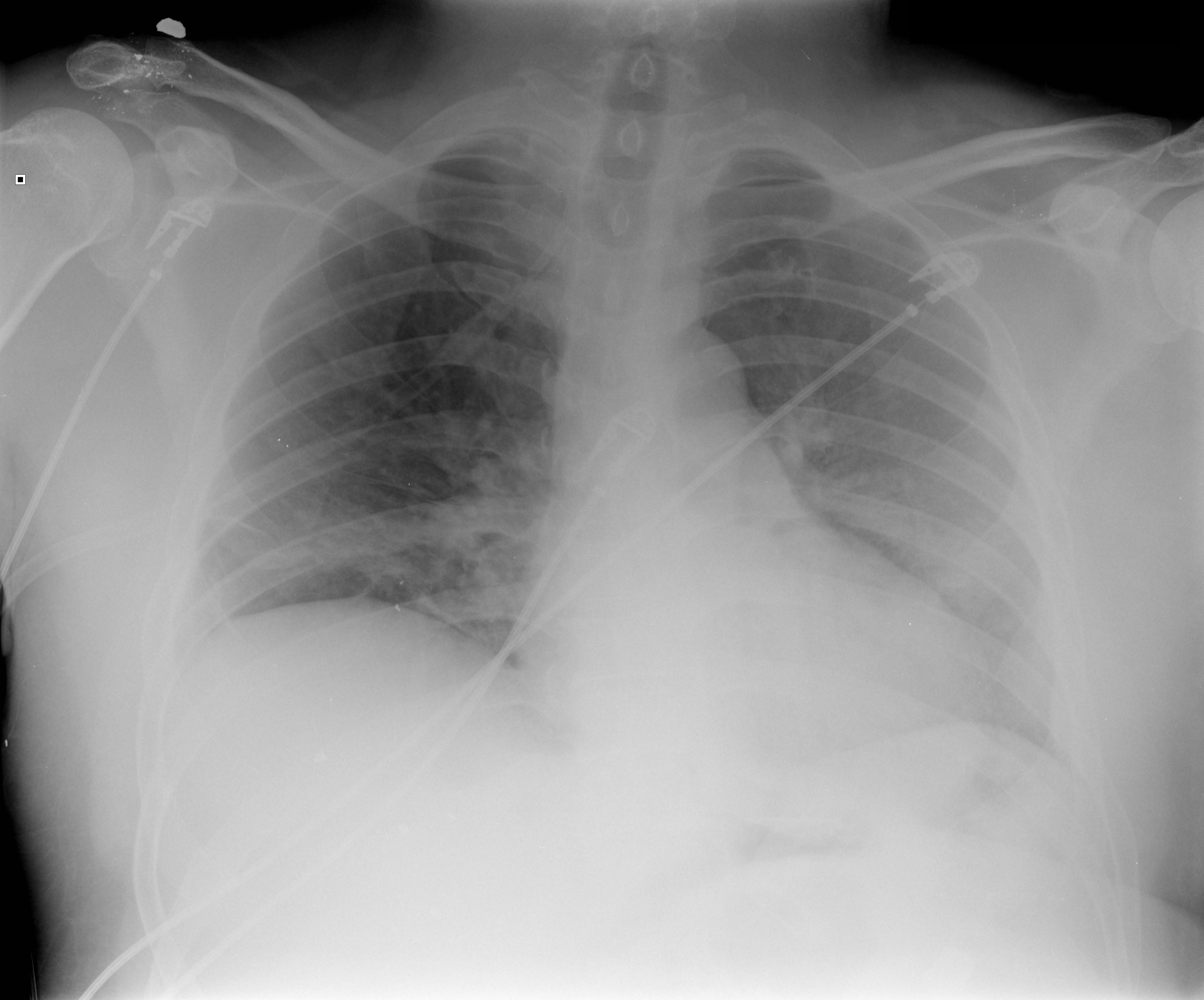
Category: Visual Diagnosis
Posted: 2/4/2013 by Haney Mallemat, MD
(Updated: 3/20/2013)
Click here to contact Haney Mallemat, MD
40 year-old male presents with fever, chills, & cough. What’s the diagnosis and the MOST likely cause?
Answer: Pneumatocele from MRSA pneumonia
Pneumatocele
Pneumatoceles are thin-walled, air-filled cysts with lung parenchyma; they may be solitary or multiple
Most commonly a sequellae to pneumonia secondary to Staphylococcus aureus (up to 85% of cases), although other etiologic agents have been found (Streptococcus pneumonia, E. coli, Klebsiella, Adenovirus and Tuberculosis). Non-infectious causes include trauma, hydrocarbon ingestion, and positive pressure ventilation.
Pneumatoceles are typically asymptomatic and require treatment of the inciting etiology (e.g., antibiotics for pneumonia), but complications may occur including tension pneumatocele, pneumothorax, and secondary infection of the pneumatocele.
Surgical resection is typically not needed but percutaneous catheter drainage may be required if the pneumatocele involves >50% of the hemithorax
Advise patients against exposure to high altitudes, skydiving and scuba diving until pneumatocele(s) resolve, to avoid progression to pneumothorax.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 2/3/2013 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
Dumas F, Rea T, et al. Chest compression alone cardiopulmonary resuscitation is associated with better long-term survival compared with standard cardiopulmonary resuscitation.Circulation. 2013 Jan 29;127(4):435-41.
Category: Pharmacology & Therapeutics
Keywords: lidocaine, intraosseus, IO (PubMed Search)
Posted: 1/2/2013 by Bryan Hayes, PharmD
(Updated: 2/2/2013)
Click here to contact Bryan Hayes, PharmD
Intraosseus (IO) access has become quite popular in critically ill patients requiring immediate resuscitation. In a patient responsive to pain, however, pain and discomfort is associated with the force of high-volume infusion through the established line.
Before flushing the line, consider administering preservative-free 2% lidocaine (without epinephrine) for patients responsive to pain prior to flush.
The suggested dose is 20-40 mg (1-2 mL) of the 2% lidocaine, followed by the 10 mL saline flush.
If preservative-free 2% lidocaine is not stocked in your ED, now is the time to consider adding it.
Fowler RL, Pierce, Nazeer S, et al. Powered intraosseous insertion provides safe and effective vascular access for emergency patients. Ann Emerg Med 2008;52(4):S152.
Ong MEH, Chan YH, Oh JJ, et al. An observational, prospective study comparing tibial and humeral intraosseus access using EZ-IO. Am J Emerg Med 2009;27(1):8-15. [PMID 19041528]
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Posted: 2/1/2013 by Lauren Rice, MD
Click here to contact Lauren Rice, MD
This winter season has brought a rise in influenza and RSV activity in Maryland and in many parts of the country. It is also important to remember other potentially lethal infections that are prevalent in the winter and early spring months, such as Neisseria meningitidis. In fact, a recent study2 showed a potential increase in meningococcal disease when influenza and RSV activity is high.
What:
Encapsulated, gram-negative diplococcus
Where:
Found in nasopharyngeal secretions, carrier rates 2-30% in normal populations
Who:
Age of incidence has 2 peaks: children < 2 years old, teens 15-19 years old
Young adults who live in shared housing, such as college dorms and military recruits
Clinical Presentation:
Early non-specific symptoms of URI, fever, malaise, myalgias
Meningitis: non-specific prodrome + headache, stiff neck (not found in younger children who often present atypically with irritability and/or vomiting)
Meningococcemia: above symptoms + hypotension + petechial rash (>60% of patients)
Treatment:
Early (!) antibiotics: 3rd generation cephalosporins (<3mo: cefotaxime; older infants, children, and teens: ceftriaxone); PCN G is antibiotic of choice for susceptible isolates
Early and aggressive management of shock
Prevention:
Tetravalent vaccine, MCV4 (Menactra, Menveo), available for serogroups A, C, Y and W-135 is given routinely at age 11-12 years old with an additional booster at 16-17 years old. MCV4 does not protect against serogroup B which accounts for 30% of infections.
1. Cross JT, Hannaman RA. Infectious Disease. MedStudy Pediatrics Board Review Core Curriculum: 5th edition. 2012; 5-11.
2. Jansen AG, Sanders EA, VAN DER Ende A, VAN Loon AM, Hoes AW, Hak E. Invasive pneumococcal and meningococcal disease: association with influenza virus and respiratory syncytial virus activity?. Epidemiol Infect. Nov 2008;136(11):1448-54.
3. Javid MH. Meningococcemia. Available at http://emedicine.medscape.com/article/221473. Medscape Reference. Last updated Aug. 2. 2012.
Category: Toxicology
Keywords: atorvastatin, acetylcysteine (PubMed Search)
Posted: 1/31/2013 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
There have been many attempts to reduce the incidence of contrast-induced nephropathy. Mechanism usually centers around antioxidant properties or free radical scavengers that prevent the acute kidney injury that may result after intravenous contrast. IV Fluid hydration, sodium bicarbonate and acetycysteine have been studied with only some evidence. There is also some controversial data that is beginning to surface regarding the use of atorvastatin with a recent article in Circulation 2012 that showed high dose atorvastatin (80mg) 24 hrs prior to angiography prevented contrast-induced acute kidney injury in patients with mild to medium risk. Link to article has been provided:
http://circ.ahajournals.org/content/126/25/3008
Category: International EM
Keywords: melioidosis, pneumonia, Thailand, international, infectious disease (PubMed Search)
Posted: 1/30/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Case Presentation:
A 43 year old diabetic woman presents with dyspnea and a dry cough. Her vital signs are: BP 84/42, HR 135 RR 37 T 38.5. Lobar consolidation is seen on chest xray. She decompensates and is intubated, a central line is placed, and IV fluids are started. Her husband reports that they had just returned from a vacation in Thailand one week earlier.
Clinical Question:
Does the recent travel change your choice of empiric antibiotics?
Answer:
The patient should also be covered for melioidosis, and infection caused by Burkholderia pseudomallei.
Bottom Line:
Patients presenting with severe infections and recent travel to an endemic area should receive emperic antibiotics with ceftazidime or a carbapenem until another source is identified.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD, MPH
Wiersinga WJ, Currie BJ, Peacock SJ. Melioidosis. N Engl J Med. 2012;367(11):1035-44.
http://www.cdc.gov/melioidosis/index.html
Category: Critical Care
Posted: 1/29/2013 by Haney Mallemat, MD
(Updated: 1/30/2013)
Click here to contact Haney Mallemat, MD
The updated Surviving Sepsis Guidelines have been released (click here) and here are some recommendations as they pertain to hemodynamic management (grades of recommendations in parenthesis).
Fluid therapy
Vasopressors (targeting MAP of at least 65 mmHg)
Corticosteroids
Inotropic Therapy
Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock. Crit Care Med. 2013 Feb;41(2):580-637.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/28/2013 by Haney Mallemat, MD
(Updated: 1/29/2013)
Click here to contact Haney Mallemat, MD
40 year-old female drove into a ditch. Right sided chest pain and stable vitals. Here's the CT but what do you think the initial CXR showed (Hint: it's a trick)?
Here's the initial CXR. Click here for the video presentation.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 1/27/2013 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
Category: Orthopedics
Keywords: Hematoma Block, anesthesia, fracture reduction (PubMed Search)
Posted: 12/27/2012 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Hematoma Block
Provides good aesthesia for reduction of fractures. Onset in approximately 5 minutes
Benefits: No need for NPO, simple and easy to perform & can be done without additional personnel (unlike w/ procedural sedation)
Contraindications: Open fractures, dirty or infected overlying skin
1) Identify fracture site with x-ray and palpation
2) Clean skin w/ Betadine
3) Insert needle into the hematoma. * Confirm placement by aspirating blood *
4) Inject anesthetic (lidocaine 1 or 2%) into the fracture cavity and adjacent periosteum
http://www.youtube.com/watch?v=tjnsdjfwMmY
Category: Toxicology
Keywords: cyclophosphamide (PubMed Search)
Posted: 1/24/2013 by Fermin Barrueto
Click here to contact Fermin Barrueto
Cyclophosphamide-induced hemorrhagic cystitis is a well known to oncologists. This unique complication of this chemotherapeutic drug has a defined mechanism and could be seen in your Emergency Department.
- Hemorrhagic cystitis occurs in 46% of patients that receive cyclophosphamide
- Can occur even months after administration
- 5% can actually die from the hemorrhage
- Treatment: Bladder irrigation, hydration, supportive. Oral adminsitration of MESNA (2mercaptoethan sulfonate) and bladder irrigation with prostaglandins and even methylene blue have been attempted.
Category: International EM
Keywords: neurocysticercosis, seizure, Taenia, tapeworm (PubMed Search)
Posted: 1/23/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
A 38 year old man is brought in by ambulance for a seizure. His medical history is not known. On exam he is post-ictal and otherwise has a non-focal neurologic exam. He has an abrasion above the right eye, a small tongue laceration, and was incontinent of urine. A head CT was done and is shown below. What was the cause of this man's seizure?

Neurocysticercosis--a parasitic infection of the nervous system by the pork tapeworm, Taenia solium.
Bottom Line:
Neurocysticercosis is a common cause of seizures globally, often with evidence of disease on CT imaging.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg
Carpio, A. Neurocysticercosis: an update. Lancet Infect Dis 2002; 2: 751–62.
Ong S, Talan DA, Moran GJ, Mower W, Newdow M, Tsang VC, Pinner RW; EMERGEncy ID NET Study Group. Neurocysticercosis in radiographically imaged seizure patients in U.S. emergency departments. Emerg Infect Dis 2002; 8: 608-13.
Garcia HH, Del Brutto OH; Cysticercosis Working Group in Peru. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol 2005; 4: 653-61.
Category: Critical Care
Posted: 1/22/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Postintubation Hypotension
Heffner AC, Swords D, Kline JA, et al. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care 2012; 27:417e9-417e13.
Heffner AC, Swords D, Nussbaum ML, et al. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care 2012; 27:587-593.
Category: Visual Diagnosis
Posted: 1/21/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
45 year-old male complains of chest pain and cough. He also tells you, "...oh, and by the way doc, I just smoked something." What's the diagnosis?
Visual pearls is two years old!!! I want to take this time to thank you all for your support....and now, your answer.
Restrepo, C. et al. Pulmonary complications from cocaine and cocaine-based substances: imaging manifestations. Radiographics. Jul-Aug 2007; 27(4): 941-56
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
