Category: International EM
Posted: 3/6/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
-A genetic autosomal recessive blood disorders that result from a defect in either the alpha (α) or Beta (β) globin chain in the hemoglobin molecule.
-Most common in people from a Mediterranean origin.
-Three types depending on the affected globin chain, α, β, or Delta (δ)
-Presents as hemolytic anemia with hepato-splenomegaly.
-Can present as mild anemia and may be misdiagnosed as iron deficiency anemia.
-Diagnosis is made through studies such as bone marrow examination, hemoglobin electrophoresis, and iron studies.
-The disease can cause hemochromatosis, which may be worsened by repeated blood transfusions.
-Hemochromatosis damages multiple organs including the Liver, spleen, endocrine glands and the heart causing cardiomyopathy and consequently heart failure.
-Severe thalassemia usually requires blood transfusion on regular basis (first measure effective in prolonging life)
-Treatment of trait cases is symptomatic with analgesics, anti-inflammatory (steroids or NSAIDs)
-The introduction of chelating agents capable of removing excessive iron from the body has dramatically increased life expectancy.
-Deferasirox (Exjade) was approved by the FDA in January 2013 for treatment of chronic iron overload caused by nontransfusion-dependent thalassemia.
Delvecchio M, Cavallo L. Growth and endocrine function in thalassemia major in childhood and adolescence. J Endocrinol Invest. Jan 2010;33(1):61-8
Cunningham MJ, Macklin EA, Neufeld EJ, et al. Complications of beta-thalassemia major in North America. Blood. Jul 1 2004;104(1):34-9
Fucharoen S, Ketvichit P, Pootrakul P, et al. Clinical manifestation of beta-thalassemia/hemoglobin E disease. J Pediatr Hematol Oncol. Nov-Dec 2000;22(6):552-7
Claude Owen Burdick. "Separating Thalassemia Trait and Iron Deficiency by Simple Inspection". American Society for Clinical Pathology. http://ajcp.ascpjournals.org/content/131/3/444.short
Category: Critical Care
Posted: 3/5/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Ventilator-associated Pneumonia
Kollef MH. Ventilator-associated complications, including infection-related complications. Crit Care Clin 2013; 29:33-50.
Category: Visual Diagnosis
Posted: 3/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
65 year-old male with acute pulmonary edema. Ultrasound at the bedside shows this. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+(+criticalcarenow)
Category: Cardiology
Posted: 3/3/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Category: Pharmacology & Therapeutics
Keywords: ischemic stroke, hypertension, blood pressure (PubMed Search)
Posted: 2/25/2013 by Bryan Hayes, PharmD
(Updated: 3/2/2013)
Click here to contact Bryan Hayes, PharmD
The newest iteration of 'Guidelines for the Early Management of Patients with Acute Ischemic Stroke' was recently published. Here are the key revisions specific to blood pressure management:
If administering rtPA, blood pressure needs to be <185/110 mm Hg. That recommendation didn't change.
Jauch EC, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013 Jan 31 [Epub ahead of print]. PMID 23370205.
Follow me on Twitter (@PharmERToxGuy)
Category: Toxicology
Keywords: carbon monoxide, rhabdomyolysis, hydroxycobalamin (PubMed Search)
Posted: 2/28/2013 by Fermin Barrueto
Click here to contact Fermin Barrueto
A foley is inserted in a fire victim patient. Urine return is in picture. Describe the reason for this colored urine.
Special Thanks to Dr. Doug Sward for the urine picture
Rhabdomyolysis causes a tea colored urine and can be seen in carbon monoxide poisoning. This picture is NOT from rhabdomyolysis.
In some fires, especially if there was a lactate > 10mmol/L, patients may also suffer from inhaled cyanide poisoning. Adminstration of the cyanide antidote, hydroxycobalamin, will cause an artificial drop in your pulse ox during administration due to the color of the infused liquid. It will, as the picture is showing, also change the color of the urine.
Category: International EM
Keywords: disaster, Sphere, international, sanitation, hygiene, infectious disease, water (PubMed Search)
Posted: 2/27/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Background Information:
Ever wonder what you would do if you were the first on scene after the earthquake in Haiti or in the Superdome as Hurricaine Katrina survivors started to arrive? How could you save the most lives? As is typical of emergency medicine, blood and gore tend to get the most attention, but if you want to save lives you have to think about what is the greatest life threat. In a large-scale disaster, it turns out, lack of water and abundance of feces kill the most the fastest and need to be addressed first.
The Sphere Project Handbook:
-one of the core documents of humanitarian response
-outlines what should be done to save the most lives in the first days, weeks, and months of a disaster.
-available free online (see reference below)
Pertinent Conclusions: (need-to-know recommendations for the first few days)
-Water: 15L/person/day (any quality--sanitize as per our previous pearl)
-Latrines: max 20 people/latrine, <50m from dwellings, >30m from water sources
-What kind?
-First 2-3 days: demarcated defecation area
-days-2 months: trench latrines (shallow trenches to defecate in)
Other hygeine:
-Solid waste disposal: one 100L refuse container/10 households, emptied at least 2x/week
-Dead bodies: dispose of according to local custom. Generally not an immediate source of infection
-Shelter: >3.5 sq. meters/person of covered floor space
Bottom LIne:
People's need for water and defecation will not stop in a disaster and too little water and too much excrement are the greatest immediate life threats to disaster survivors. Plan to deal with these early to save the most lives.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
The Sphere Project. Sphere Handbook: Humanitarian Charter and Minimum Standards in Disaster Response, 2011, 2011, ISBN 92-9139-097-6, available at: http://www.sphereproject.org/handbook/
Category: Critical Care
Posted: 2/26/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Excessive and improper administration of local anesthetic (a.k.a. local anesthetic systemic toxicity or L.A.S.T.) can lead to cardiac toxicity with symptoms ranging from benign arrhythmias to overt cardiac arrest.
Administration of a 20% intra-lipid emulsion has been experimentally known to reverse L.A.S.T in animal models, but in 2006 the first documented human case of ILE was successfully used during cardiac arrest secondary to L.A.S.T. with hemodynamic recovery and good neurologic outcome. Many case reports have emerged since then, including the use of ILE in toxicity with other lipophilic drugs (e.g., calcium channel blockers, tricyclic antidepressants, etc.)
Several mechanisms have been proposed explaining how ILE works. They include:
Dosing of ILE:
Check out this video by our own Dr. Bryan Hayes(@PharmERToxGuy) and Lipidrescue.org for more information.
Weinberg, G. Lipid emulsion infusion: resuscitation for local anesthetic and other drug overdose. Anesthesiology 2012 Jul;117(1):180-7.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 2/24/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Noninvasive Cardiac Screening in Young Athletes With Ventricular Arrhythmias. Steriotis A, Nava A, et al. The American Journal of Cardiology. Feb 2013:111;4, 557-562.
Category: Orthopedics
Keywords: head injury, concussion, return to play, cognitive rest (PubMed Search)
Posted: 2/23/2013 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Just before you upgraded your old computer, recall what happened when you had Excel, Word and PowerPoint all open at the same time. In the concussed state, the brain is essenatially functioning like your old computer... and the more tasks it must perform, the slower it will work and slower it will recover. Hence the concept of cognitive rest. Below is taken from the AMSSM position statement of concussion in sport.
Return to school
There are no standardized guidelines for returning the injured athlete to school. If the athlete develops increased symptoms with cognitive stress, student athletes may require academic accommodations such as a reduced workload, extended test-taking time, days off or a shortened school day.
Some athletes have persistent neurocognitive deficits following a concussion, despite being symptom free. Consideration should be made to withhold an athlete from contact sports if they have not returned to their ‘academic baseline’ following their concussion (level of evidence C).
The CDC developed educational materials for educators and school administrators that are available at no cost and can be obtained via the CDC website. Additional resources for academic accommodations should be developed for both clinicians and educators (level of evidence C).
Adam Friedlander shared the practical application of this which I found amusing:
" I always recommend what Peds neuro called "a brain holiday" - my favorite part. All of our nurses look at me like I'm nuts, but it is now on our official concussion/CHI DC instructions. I always say to the kiddo: "You'll love this part. No homework, no reading." Then I turn to mom and dad and tell them they'll love the next part: "No TV, no video games."
Thank you for sharing Adam!!
American Medical Society for Sports Medicine position statement: concussion in sport
Category: Pediatrics
Posted: 2/22/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Luu JL, Wendtland CL, Gross MF, et al. Three percent saline administration during pediatric critical care transport. Ped Emerg Care 2011;27(12):1113-1117
Category: Toxicology
Keywords: opioid, withdrawal, seizure (PubMed Search)
Posted: 2/21/2013 by Fermin Barrueto
Click here to contact Fermin Barrueto
Typical opioid withdrawal include clinical symtpoms of piloerection, nausea, vomiting and diarrhea. If you were to see seizure, another etiology other than opioid withdrawal should be investigated.
Except in the case of neonates borne to women who have been taking opioids chronically such as a methodone patient. Once the child is born, symptoms of withdrawal may take days to weeks to materialize though seizures typically occur <10 days. The child is at increased risk of SIDS as well.
Category: International EM
Keywords: japanese encephalitis, international, virus, infectious disease (PubMed Search)
Posted: 2/20/2013 by Andrea Tenner, MD
(Updated: 2/2/2026)
Click here to contact Andrea Tenner, MD
Japanese Encephalitis
http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/japanese-encephalitis.htm#2473
Category: Critical Care
Posted: 2/19/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Managing Traumatic Hemorrhagic Shock
Bougle A, et al. Resuscitative strategies in traumatic hemorrhagic shock. Annals of Intensive Care 2013; 3.
Category: Visual Diagnosis
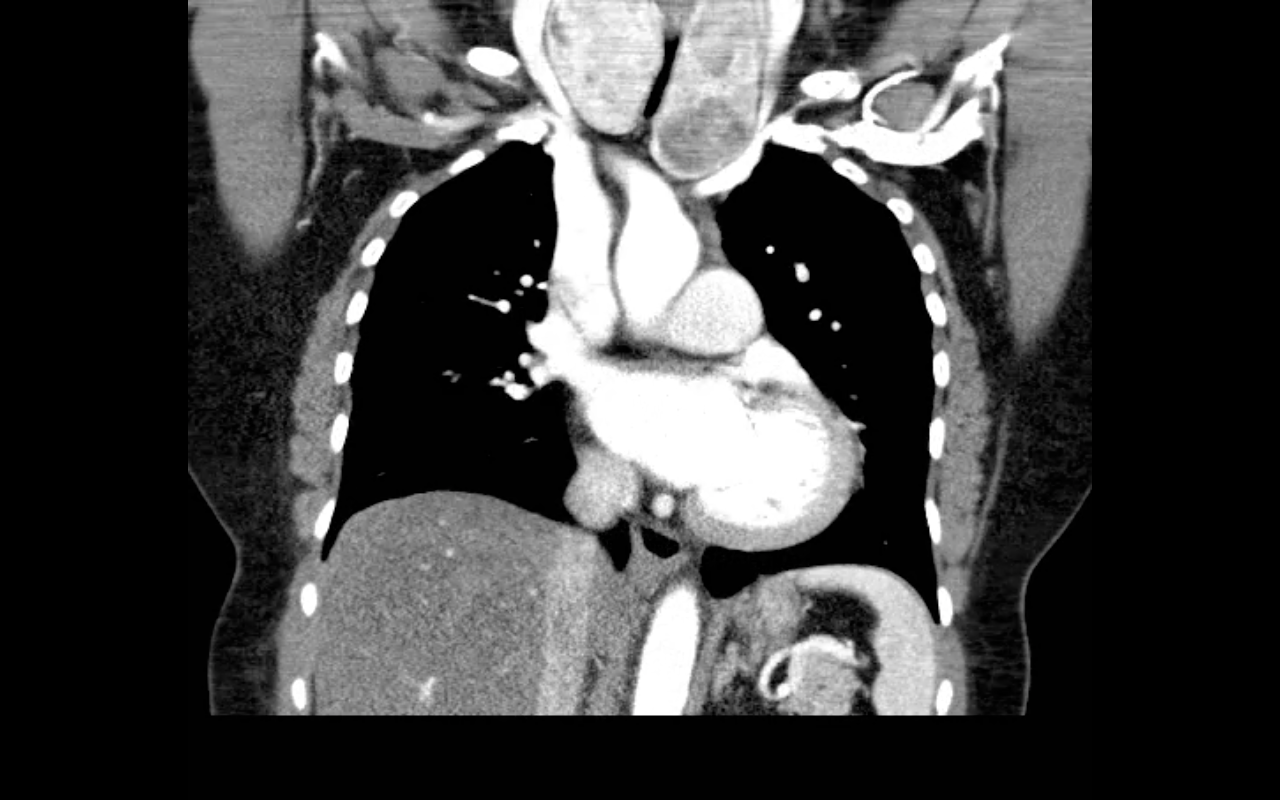
Posted: 2/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
68 year-old female presents with stridor and palpable goiter. Here's a clip from CT of the chest. What's the diagnosis?
Category: Cardiology
Keywords: Transcatheter Aortic-Valve Replacement (TAVR) (PubMed Search)
Posted: 2/17/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Makkar R, Fontana G, et al. Transcatheter Aortic-Valve Replacement for Inoperable Severe Aortic Stenosis. NEJM. May 2012: 366; 18.
Category: Toxicology
Keywords: antidote, pregnancy, ethanol, amyl nitrate, methylene blue, penicillamine, lorazepam, diazepam (PubMed Search)
Posted: 2/13/2013 by Bryan Hayes, PharmD
(Updated: 2/14/2013)
Click here to contact Bryan Hayes, PharmD
Most antidotes have not been adequately studied in pregancy and hold a Pregnancy Risk Category 'C' by the FDA. However, there are a few antidotes that hold a category 'D' or 'X' rating (contraindicated).
In most cases, the benefits of short-term use probably outweigh the risk, especially when accounting for the health and prognosis of the mother.
Lexi-Comp Online, Lexi-Drugs Online, Hudson, Ohio: Lexi-Comp, Inc.; February 14, 2013.
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Posted: 2/13/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
- The most common disease producing enzymopathy in humans
- Affects 400 million people worldwide
- Highest prevalence is among persons of African, Asian, and Mediterranean descent
- Patients can be asymptomatic but may present with symptoms of acute hemolytic anemia, which may be precipitated by certain medications (Oxidative medications) or foods (some types of beans)
- Avoid oxidative drugs (consult your PharmD when your patient has G6PDd)
- Diagnosis: Measure the actual enzyme activity of G6PD rather than the amount of the enzyme. A more practical test is the presence of Indirect hyperbilirubinemia, but it is non specific
- Treatment consists of oxygen and bed rest in minor cases. However, severe cases may require PRBC transfusion
Beutler E. Glucose-6-phosphate dehydrogenase deficiency: a historical perspective. Blood. Jan 1 2008;111(1):16-24
Nkhoma ET, Poole C, Vannappagari V, et al. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. May-Jun 2009;42(3):267-78
Category: Critical Care
Posted: 2/12/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Propofol is generally a well-tolerated sedative / amnestic but occasionally it can lead to the propofol infusion syndrome (PRIS); a metabolic disorder causing end-organ dysfunction.
Suspect PRIS in patients with increasing lactate levels, worsening metabolic acidosis, worsening renal function, increased triglyceride levels, or creatinine kinase levels. End-organ effects include:
The true incidence of PRIS is unknown, however, certain risk factors have been identified:
Prevent PRIS by using adequate analgesia (with morphine or fentanyl) post-intubation, which may reduce the overall dosage of propofol ultimately reducing the risk.
If PRIS develops, stop propofol and provide supportive care; IV fluids, ensuring good urine output, adequate oxygenation, dialysis (if indicated), vasopressor and inotropic support.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/10/2013 by Haney Mallemat, MD
(Updated: 2/11/2013)
Click here to contact Haney Mallemat, MD
A 25 year-old female presents complaining of a "net-like" rash bilaterally on her medial thighs. She denies any pain but states that the rash looks “pretty scary” What's the diagnosis?

Answer: Erythema ab igne (a.k.a. "toasted-skin syndrome")
Erythema ab igne
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
